-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Virology and Molecular Biology
p-ISSN: 2163-2219 e-ISSN: 2163-2227
2025; 14(4): 46-50
doi:10.5923/j.ijvmb.20251404.02
Received: May 17, 2025; Accepted: Jun. 10, 2025; Published: Jun. 17, 2025

Hormonal Imbalance in a Patient with Bronchial Asthma: Key Aspects
Abdullaeva Dilafruz Gayratovna1, Abdullaeva Dilorom Telmanovna2, Akramkhujaeva Aziza Bakhodir qizi2
1Department of Children and Adolescents’ Hygiene, and Nutrition of Tashkent Medical Academy, Tashkent, Uzbekistan
2Department of Children Diseases of Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Abdullaeva Dilafruz Gayratovna, Department of Children and Adolescents’ Hygiene, and Nutrition of Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

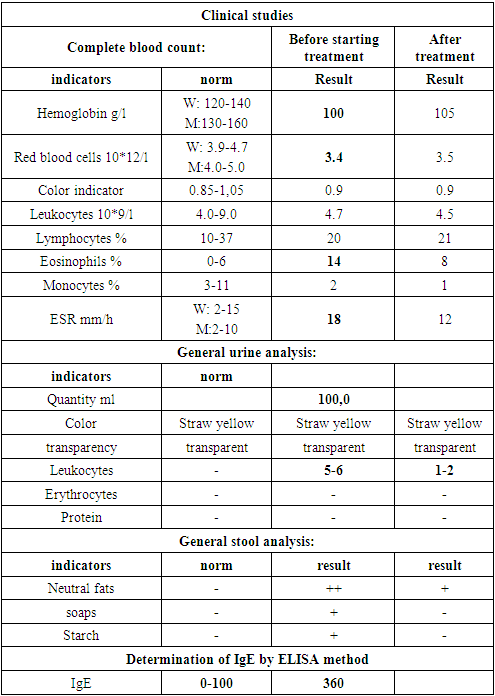
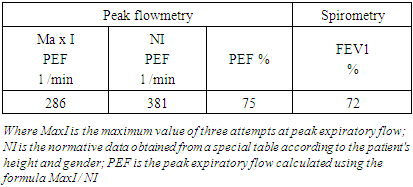
Chronic inflammation contributes to the remodeling of the repiratory tract, resulting in irreversible structural alterations and a progressive decline in pulmonary function. These pathological changes inevitably compromise the quality of life in pediatric patients, heightening the risk of early disability and adversely influencing their psychoemotional well-being. Morever, bronchial obstruction and hypoxic states in individuals with bronchial asthmaprofoundly impact the regulation of hormonal mechanisms within the reproductive system. Objective. The patient with bronchial asthma with the hormonal balance features. Materials and methods. 16-year-old patient case report, which is including the anamnesis vitae, anamnesis morbi, family anamnesis according to the disease, complaints, objective and physical methods of investigation, laboratory analysis CBT, hormones analysis by CLIA method, instrumental methods to establish the stages of BA. Results and discussion. Based on patient’s hormonal profile, elevated levels of prolactin and testosterone were identified, suggesting that stress-induced adaptive mechanisms, along with hormone therapy administered due to the chronic hypoxic state, inevitably influenced the pituitary function within endocrine system. Conclusion. Sex hormones play a crucial role in pathogenesis and progressin of bronchial asthma. Estrogens contribute to heightened bronchial hyperreactivity, whereas testosterone, in contrast, exhibits protective effects.
Keywords: Bronchial asthma, Adolescent, Sex hormones, Menstrual cycle, Hypoxmia, Estrogen, Prolactin, Testosterone
Cite this paper: Abdullaeva Dilafruz Gayratovna, Abdullaeva Dilorom Telmanovna, Akramkhujaeva Aziza Bakhodir qizi, Hormonal Imbalance in a Patient with Bronchial Asthma: Key Aspects, International Journal of Virology and Molecular Biology, Vol. 14 No. 4, 2025, pp. 46-50. doi: 10.5923/j.ijvmb.20251404.02.
1. Introduction
- One of the most pressing problems in pediatrics is bronchial asthma (BA), which is highly heterogeneous among other diseases, characterized by chronic inflammatory disease of the bronchi, accompanied by respiratory symptoms such as wheezing, shortness of breath, chest tightness, cough and decreased exercise tolerance. Clinical manifestations of BA depend on its severity and the degree of airway obstruction [1].In children, the main pathogenetic mechanisms for the development of bronchial asthma are often immune and neurogenic reactions of the body in response to allergens, where a key role is played by inflammatory cells such as mast cells, eosinophils, T- lymphocytes and neutrophils, which contribute to the activation of inflammatory mediators, including histamines, leukotrienes and bradykinins, thereby causing bronchial hyperreactivity, increased mucus secretion and bronchial constriction [2].Long-term inflammation can cause remodeling of the respiratory tract, leading to irreversible structural changes and progressive deterioration of lung function. These processes inevitably affect the child’s quality of life, increasing the risk of early disability and having a negative impact on his psychoemotional state [1,2].Not only immune and neurogenic factors, but also endocrine mechanisms play a special role in pathogenesis of bronchial asthma. The role of sex and gonadotropic hormones in the pathogenesis of bronchial asthma in adolescents is currently an undoubted, but poorly studied problem. Bronchial obstruction and hypoxic condition in patients with bronchial asthma significantly affect the regulation of hormonal mechanisms of the reproductive system. Analysis of data reflecting the severity of the disease and the characteristics of broncho-obstructive syndrome depending on gender revealed certain patterns. In girls, despite a shorter duration of the disease, a more pronounced degree of bronchoconstriction was noted compared to boys, which may indicate the influence of sexual factors on the pathophysiological mechanisms of bronchial obstruction.Sex hormones estrogens, progesterone and testosterone have a significant impact on the development and course of bronchial asthma, which explains gender differences in the prevalence and severity of the disease at different ages. Estrogens have the ability to activate the immune response, namely Th 2 and allergic inflammation, i.e. they promote an increase in the production of IgE, eosinophils and the release of inflammatory mediators. Under the influence of estrogens, the reactivity of the bronchi to triggers (allergens, infections, physical and psychoemotional stress) of this nosology increases. Comorbidity of bronchial asthma and a constantly high level of estrogens can contribute to remodeling of the airways in persistent forms with frequent attacks. It was also found that estrogens reduce the sensitivity of β2- adrenergic receptors, which explains the reduced effectiveness of treatment with bronchodilators of this group. The manifestation of estrogens in the course of asthma according to age category and gender is determined by the fact that in childhood before puberty, asthma is more common in boys, but after puberty, its prevalence becomes higher in girls. In adolescent girls, a worsening of symptoms before menstruation (premenstrual asthma) may be observed due to fluctuations in the level of estrogens and progesterone. Progesterone is also involved in the regulation immune response and respiratory function and the main mechanisms of influence of progesterone is its ability to dilate the bronchi, suppress inflammatory reactivity by reducing the activation of eosinophils and the production of cytokines.Testosterone has a predominantly protective effect on bronchial asthma, which partly explains the lower prevalence of the disease in men after puberty. Testosterone helps suppress IgE production and reduce eosinophil activity, reducing allergic inflammation, reducing bronchial hyperreactivity, and suppressing the release of inflammatory mediators.When analyzing the signs of secondary sexual development, it was found that some girls had a delay in the rate of sexual maturation. In such cases, the signs of sexual maturation developed slowly or the process of their formation stopped, as a result of which menarche did not occur. According to the study conducted by L.I. Muradosilova and N.N. Kaladze, hormonal changes during puberty in girls with bronchial asthma (BA) were studied. The study included girls aged 7 to 16 years, who were in the phase of exacerbation and remission of the disease. The study found that during the transition from prepuberty (7-11 years) to puberty (12 years), girls experience a significant increase in LH levels (with reliability p<0.05); at the age of 12-16 years, a significant increase in testosterone levels was recorded, while estradiol levels demonstrated an inverse relationship with reliability.In girls with bronchial asthma, an increase in the levels of gonadotropic hormones was observed both in the exacerbation phase and in the remission phase. In the group of girls aged 7-11 years, the level of LH was significantly increased during the period of bronchial asthma exacerbation (p<0.05), which indicates the body's response to stress factors associated with the disease. In the group of girls aged 12-16 years, a significant decrease in the level of prolactin was recorded during the period of exacerbation, which may be associated with insufficient adaptation of the body to stress during this period. In girls aged 12-16 years, the level of testosterone remained high during the remission phase, while its fluctuations with age were insignificant. Estradiol also remained stable during the remission phase, but with age its level decreased in both phases of bronchial asthma with reliability (p<0.01) [4,5].Thus, sex hormones have a significant impact on the development and course of bronchial asthma. Estrogens and progesterone under certain conditions can increase bronchial hyperreactivity, while testosterone, on the contrary, has a protective effect. Gender differences in the prevalence and severity of bronchial asthma are associated with changes in hormonal levels at different age periods and this is explained by the fact that it is necessary to take into account a personalized approach to the treatment and control of the disease.
2. Clinical Case
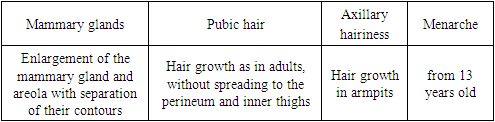
- Patient M.M.Kh. was admitted to the allergology department of the Tashkent Medical Academy, a multidisciplinary clinic, with complaints of shortness of breath, asthma attacks, distant wheezing, nasal congestion, and cough with difficult-to-separate sputum.It is known from the medical history that the patient has been ill since the age of 10. The disease began with attacks of shortness of breath and suffocation with difficulty breathing after an infectious disease. These attacks can be observed all year round, regardless of the season. Bronchial hyperreactivity to dust triggers is mainly observed. The child received inpatient treatment in the allergology department of TMA No. 1 in September 2020, in August 2022 and in March 2023. The patient receives continuous outpatient treatment, since 2020 he has been receiving ICS with the active substance budesonide. 5 days before admission to the hospital, the patient fell ill with an acute respiratory infection (ARI), after which attacks of bronchial asthma began.From the anamnesis of life it is known that the child from the 2nd pregnancy is the 2nd child, born on time with a body weight of 3500 g, and a height of 55 cm, without any pathological changes and pathological manifestations of the processes of labor. The child was breastfed until 1.5 years. The girl grew and developed according to her age.Allergological anamnesis also includes a history of atopic dermatitis, received all vaccinations without any particular pathological reactions. Alimentary allergies: citrus fruits, legumes, nuts, sweets. Hereditary burden: the patient's father has bronchial asthma.Epidemiological history:1. From infectious diseases (typhoid fever, paratyphoid fever, salmonellosis, tuberculosis, venereal diseases).2. Past illnesses: in March 2009, she had viral hepatitis A and received inpatient treatment. In August of the same year, she had chickenpox and received inpatient treatment.3. The patient did not receive FFP, Albumin, Histoglobulins.Status praesens objectivus: general condition of the patient upon arrival, the girl's condition was assessed as moderate. Consciousness is clear. Decreased appetite. The skin is clean, without rashes. The palatine tonsils are unchanged. The posterior wall of the oral cavity is hyperemic. The peripheral lymph nodes are not enlarged, motionless and painless. Mixed breathing. The respiratory rate is 22 per minute, a box-like sound is detected during percussion of the lungs. During auscultation of the lungs, dry wheezing is heard against the background of harsh breathing. Cough with difficult-to-separate sputum. From the cardiovascular system: no pathological changes are observed. Heart sounds are muffled, the pulse is rhythmic, of satisfactory filling and tension. PS - 85 per minute. Gastrointestinal tract: the tongue is clean, not coated. The abdomen is soft, painless, tympanic sound on percussion. The size of the liver and spleen are within normal limits. The act of defecation is 1-2 times a day. From the side of signs of sexual development and the urinary system, there are no changes and correspond to the norm. Phenotypic indices of secondary sexual characteristics
|
|
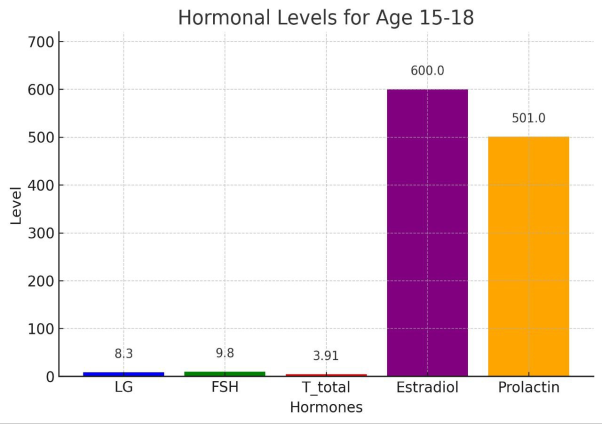 | Figure 1. Patient’s hormonal parameters |
|
3. Conclusions
- Bronchial asthma, as a chronic inflammatory disease associated with a significant stress burden, can activate prolactin secretion, which enhances T-cell activation and the release of pro-inflammatory cytokines, potentially exacerbating the severity of disease. Hypoxic conditions resulting from bronchial obstruction may stimulate the pituitary gland to secrete hormones that regulate reproductive function, thereby disrupting the balance of sex hormones. Sex and gonadotropic hormones affect the course of the disease, while gender differences in the prevalence and severity of bronchial asthma are associated with changes in hormonal levels at different age periods. It is known that bronchial asthma is more common in girls after puberty than in boys, which is explained by changes in the concentrations of estrogens, progesterone and testosterone [4,5]. Estrogens activate the Th2-mediated immune response, promoting an increase in the production of IgE, eosinophils and inflammatory mediators, which increases the reactivity of the bronchi to triggers. High estrogen levels can lead to remodeling of the airways in persistent forms of bronchial asthma, as well as reduce the sensitivity of β2-adrenergic receptors, which explains the decrease in the effectiveness of bronchodilators [6]. In adolescent girls, worsening asthma symptoms are observed before menstruation, which is associated with fluctuations in estrogen and progesterone levels (premenstrual asthma) [7].Progesterone has the ability to dilate the bronchi and suppress inflammatory activity by reducing the production of eosinophils and proinflammatory cytokines. However, its effect depends on the concentration and interaction with other hormones, which requires further study [8]. Testosterone, on the contrary, has a protective effect by suppressing the synthesis of IgE, reducing the activity of eosinophils and allergic inflammation, reducing bronchial hyperreactivity and the release of inflammatory mediators. This explains the lower prevalence of bronchial asthma in boys after puberty [9].Clinical studies show that girls with bronchial asthma may experience delayed puberty, which is expressed in slow development of secondary sexual characteristics and late onset of menarche. According to studies conducted by L. I. Muradosilova and N. N. Kaladze, girls with bronchial asthma during puberty showed a significant increase in luteinizing hormone (LH) levels, as well as a decrease in prolactin levels during an exacerbation of the disease. In girls aged 12-16 years, a significant decrease in prolactin levels was observed during exacerbation period, which was associated with insufficient adaptation to stress. During the remission phase, testosterone levels remained elevated and showed minimal variation with age, a similar trend was noted for estradiol. However, estradiol levels decreased with age in both phases of the disease. In addition, patients with bronchial asthma showed a decrease in estradiol levels during the remission phase, which made indicate an endocrine imbalance [10].Thus, sex hormones have a significant impact on the pathogenesis and course of bronchial asthma. Estrogens and progesterone can increase bronchial hyperreactivity, while testosterone, on the contrary, has protective properties. Gender differences in the prevalence and severity of bronchial asthma are associated with changes in hormonal levels, which requires a personalized approach to diagnosis, treatment and monitoring of the disease in children and adolescents.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML