-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Virology and Molecular Biology
p-ISSN: 2163-2219 e-ISSN: 2163-2227
2025; 14(4): 43-45
doi:10.5923/j.ijvmb.20251404.01
Received: May 17, 2025; Accepted: Jun. 12, 2025; Published: Jun. 17, 2025

Modern Approaches to the Diagnosis and Therapy of Bronchial Asthma Considering Infectious and Dysplastic Factors
Abdullayeva Dilorom Telmanovna1, Ilmuratova Munisa Abduqayum qizi2
1PhD, Associate Professor, Department of Pediatric Diseases, Tashkent Medical Academy, Tashkent, Uzbekistan
2Assistant, Department of Pediatric Diseases, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Abdullayeva Dilorom Telmanovna, PhD, Associate Professor, Department of Pediatric Diseases, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Bronchial asthma is a chronic inflammatory disease of the airways, characterized by variable airflow obstruction and bronchial hyperresponsiveness. In recent years, increasing attention has been given to the role of infectious agents and connective tissue dysplasia in the pathogenesis, clinical course, and treatment outcomes of bronchial asthma. This abstract highlight modern diagnostic strategies that incorporate the identification of infectious triggers, as well as structural abnormalities associated with connective tissue dysplasia, particularly in pediatric patients. Therapeutic approaches now emphasize personalized medicine, targeting underlying dysplastic changes and optimizing anti-inflammatory and antimicrobial therapies. Early identification of comorbid conditions, including connective tissue dysplasia-related anomalies, is crucial for effective asthma control and improved quality of life. Integrating multidisciplinary methods enhances both diagnostic accuracy and therapeutic efficacy in managing bronchial asthma with complex etiological backgrounds.
Keywords: Bronchial asthma, Connective tissue dysplasia, Children, Atypical infections, Chlamydia pneumoniae, Mycoplasma pneumoniae, Cytomegalovirus
Cite this paper: Abdullayeva Dilorom Telmanovna, Ilmuratova Munisa Abduqayum qizi, Modern Approaches to the Diagnosis and Therapy of Bronchial Asthma Considering Infectious and Dysplastic Factors, International Journal of Virology and Molecular Biology, Vol. 14 No. 4, 2025, pp. 43-45. doi: 10.5923/j.ijvmb.20251404.01.
Article Outline
1. Introduction
- Relevance of the Problem Bronchial asthma (BA) is one of the most common chronic non-communicable diseases in children and adolescents. According to estimates by the World Health Organization (WHO), its prevalence continues to increase, with cases of severe and difficult-to-control asthma becoming more frequent [2]. This necessitates the identification of additional factors that influence disease outcomes and treatment efficacy. Special attention is being given to hidden pathogenetic mechanisms, including connective tissue dysplasia (CTD)—a congenital systemic condition characterized by structural and functional abnormalities of connective tissue components. In children with BA, the presence of CTD worsens the clinical course of the disease by reducing the elasticity of the bronchial tree, promoting bronchial hyperreactivity, and contributing to the chronicity of inflammation [1,4,6]. At the same time, atypical pathogens—Chlamydia pneumoniae, Mycoplasma pneumoniae, and cytomegalovirus (CMV)—can persist in the body for extended periods, cause chronic inflammation and immune imbalance, and disrupt asthma control. These infections often have an asymptomatic course, which complicates their timely detection and treatment [2,3]. The relevance of this topic is supported by the results of a clinical study involving 92 children with bronchial asthma, in which more than 65% of patients with CTD were found to have markers of current or past infection. It was shown that the combination of CTD and atypical infections is associated with a more severe disease course, shorter remission periods, and the need for more intensive therapy. Thus, studying the role of infectious and dysplastic factors in the pathogenesis of bronchial asthma in children is of high scientific and practical importance. This area offers promising opportunities for more accurate diagnostics, prognosis, and the development of personalized treatment strategies.
2. Purpose of the Research
- To assess the impact of connective tissue dysplasia (CTD) and atypical infections (Chlamydia pneumoniae, Mycoplasma pneumoniae, CMV) on the clinical course of bronchial asthma in children and to substantiate the need for a personalized approach to diagnosis and therapy.
3. Materials and Methods
- A prospective study was conducted involving 92 children aged 3 to 18 years who were hospitalized in the Department of Pediatric Allergology at the 2nd Clinic of the Tashkent Medical Academy (TMA) and the Pediatric Department of the Republican Specialized Scientific-Practical Center of Allergology and Clinical Immunology. All participants were divided into two groups based on the presence of signs of connective tissue dysplasia (CTD): the first group included 59 children diagnosed with CTD according to the criteria of T.A. Kadurina (2009), and the second group included 33 children without phenotypic features of CTD. The diagnosis of bronchial asthma was established based on GINA guidelines. CTD assessment was carried out using a point-based system based on phenotypic features and signs of disembryogenesis: 0–4 points — normal, 5–10 — mild CTD, 11–20 — moderate, over 21 — severe CTD. Each child underwent a comprehensive clinical and laboratory examination, including medical history, determination of exacerbation frequency and clinical severity, as well as physical examination. Serological testing was performed using ELISA to detect IgM and IgG antibodies to Chlamydia pneumoniae, Mycoplasma pneumoniae, and cytomegalovirus (CMV). In selected cases, additional immunological markers were measured, including IgE levels and the CD4/CD8 ratio. Statistical data analysis included descriptive statistics, Pearson’s chi-square test to assess the relationship between CTD and infection frequency, and Pearson correlation analysis (r coefficient). A p-value of less than 0.05 was considered statistically significant.
4. Results and Discussion
- Analysis of data from 92 children with bronchial asthma revealed significant differences between the groups with connective tissue dysplasia (CTD+) and without it (CTD−) in terms of both the frequency of atypical infections and the severity of the clinical course and treatment needs.In the CTD+ group (n = 59), infections were detected in 41 children (69.5%).
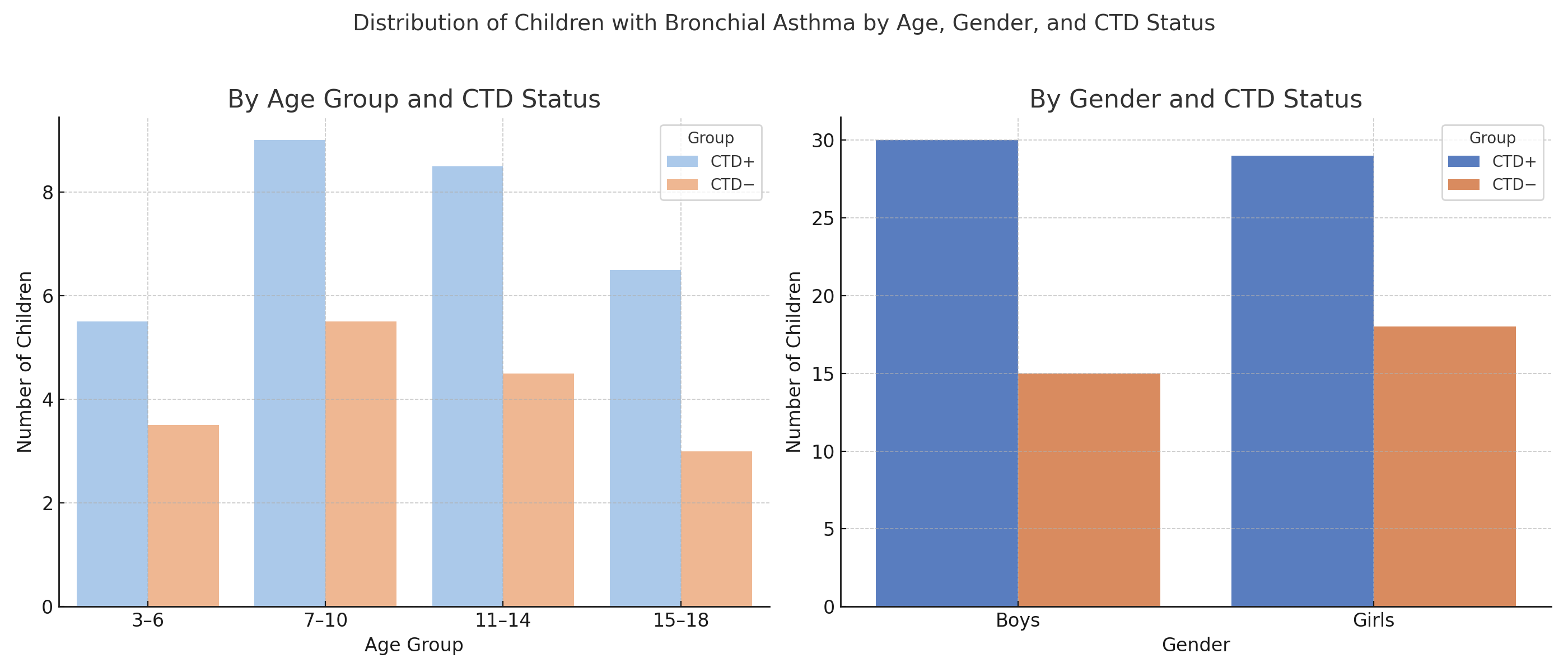 | Figure 1 |
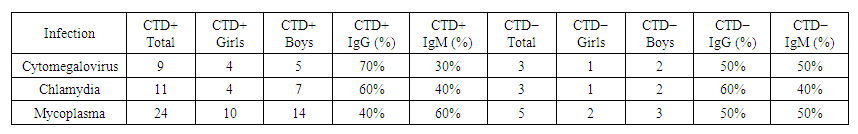 | Table 1 |
5. Conclusions
- This study, which included 92 children with bronchial asthma, demonstrated that the presence of connective tissue dysplasia (CTD) significantly influences the course of the disease and the prevalence of atypical infections. In the CTD+ group, the frequency of infections with Chlamydia pneumoniae, Mycoplasma pneumoniae, and CMV was 69.5%, compared to only 33.3% in the CTD− group. The association between CTD and infection was statistically significant (χ² test, p = 0.033), and a positive correlation was found between the severity of dysplasia and the need for combined therapy (r = +0.42; p = 0.015). Clinically, children with CTD exhibited a more severe course of bronchial asthma, with more frequent exacerbations, shorter remission periods, and a greater need for advanced therapy. These patients were more frequently treated with antibacterial and antiviral agents, immunomodulators, and enhanced baseline therapy regimens requiring individualized adjustments. In contrast, children from the CTD− group showed stable disease control with standard therapy and rarely required additional treatment. Thus, incorporating an assessment of CTD signs and conducting serological screening for atypical infections into the diagnostic algorithm for children with bronchial asthma allows for a more precise identification of pathogenetic factors, the development of personalized treatment plans, and significant improvement in clinical outcomes. A comprehensive approach to managing these patients enhances treatment effectiveness, reduces the risk of complications, and improves the child's quality of life. Therefore, in children with bronchial asthma on the background of connective tissue dysplasia, the disease is characterized by a more severe course and reduced quality of life. Early medical surveillance of such patients may facilitate successful implementation of pathogenetic therapy and help prevent serious complications, including persistent and poorly controlled asthma.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML