Kipsang A. K.1, Burugu M. W.2, Arodi W. O.1
1Department of Medical Laboratory Science, Kenyatta University, Kenya
2Department of Biochemistry and Biotechnology, Kenyatta University, Kenya
Correspondence to: Kipsang A. K., Department of Medical Laboratory Science, Kenyatta University, Kenya.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Any nation must ensure that the prevalence and incidence of particular disease is kept in check and that the population is aware in case of an increase in incidences and prevalence of a particular disease. Viruses are responsible for a large proportion of respiratory illnesses, including pneumonia. Mechanical ventilation as part of intensive care is used to support the lungs and cannot reverse any underlying diseases; however secondary complications that occur include bacterial and viral respiratory infections. These infections prolong the length of hospital stay hence impacting on available resources, in addition it also increases morbidity and mortality rates especially in patients with chronic illnesses and those who are immunosuppressed. The aim of the study was to assess the prevalence of influenza virus, rhinovirus, respiratory syncytial virus, Human Parainfluenza virus, Human metapneumovirus, adenovirus and Coronavirus in patients who are mechanically ventilated and those in the intensive care unit. It is a comparative study that sought to determine the burden of these viruses in this group of patients. The study was done at Moi teaching and referral hospital in Uasin Gishu County. Sample collection period was from 1st April 2017 to 30th August 2017. A total of 186 samples of broncho-alveolar lavage was collected and transported at 2-8°C to KEMRI Centre for Virus Research for analysis. The viral nucleic acid was detected using reverse transcriptase polymerase (RT-PCR) chain reaction. Analysis of variance (ANOVA) was used to aid in coding, entry and analysis of data. Viral test results were log-transformed to ensure normal distribution of the data and expressed as mean±standard deviation. Comparison of the viral type based on the sex of the patient and ward type was determined using ANOVA with Bonferroni’s post-test using GenStat Release 14.1 (PC/Windows). Majority of the study population was in the age bracket of above 65 years old which represented 28.8% of the study population, age group 50 to 64 years represented 24.4%, 35 to 49 years (20%), 5 to 19 years (13%), less than 5 years (11%) while the minority was age group of 20 to 34 years with 3% of the study population. Male represented 57.2% of the population that was involved and 42.3% were female. From this study the results indicate that viral respiratory tract infections are prevalent in patients both in the intensive care unit and those under mechanical ventilation in the general wards at Moi Teaching and Referral Hospital. It is evident that the infections occur across all age groups; however children less than 5 years and the elderly above 65 years recorded a higher prevalence in most viral infections as compared to other age groups. This data will find utilization in Moi Teaching and Referral Hospital in the management of the patients in the ICU and those under mechanical ventilation and overall it will contribute significantly to the reduction of mortality.
Keywords:
Prevalence, Mechanical ventilation, Co-infection, Nosocomial, Mortality, Lower respiratory tract, Upper respiratory tract
Cite this paper: Kipsang A. K., Burugu M. W., Arodi W. O., Prevalence of Viral Severe Acute Respiratory Infections in Patients in the Intensive Care Unit and Those under Mechanical Ventilation in Moi Teaching and Referral Hospital, Uasin Gishu County, Kenya, International Journal of Virology and Molecular Biology, Vol. 7 No. 1, 2018, pp. 1-10. doi: 10.5923/j.ijvmb.20180701.01.
1. Introduction
Mechanical ventilation helps to save life, however it is associated with complications that include pneumothorax, airway injury, alveolar damage, and ventilator-associated pneumonia. In addition diaphragm atrophy, decreased cardiac output, and oxygen toxicity may occur. The primary complications in patients who are mechanically ventilated are acute lung injury (ALI)/ and acute respiratory distress syndrome (ARDS) [1] which are significant contributors to patient morbidity and mortality. Secondary complications are also a challenge and they include bacterial and viral respiratory infections. Acute Viral respiratory infections are common and are usually confused as bacterial infection by clinicians [2]. Intensive care units (ICUs) are highly specialized facilities that provide special care to patients who suffer from critical disease conditions. Patients in ICU are closely monitored by a team of professionals who are highly trained and often require medication to keep them comfortable [3]. Acute respiratory infections due to viruses are very common illnesses experienced by individuals across all age groups worldwide. Upper respiratory tract (URIs) like flu is common especially in infants and young children below five years and will continue to be common with advancing age. Several episodes of cold occur in Infants and young children per year; for example those who are in day-care centers usually have many episodes per year [4, 5]. Complications like acute otitis media, asthma exacerbation occur in infections of the upper respiratory tract and finally leading to a lower respiratory tract infection (LRIs). Bronchiolitis and pneumonia rarely occur, they lead to increased morbidity and some mortality hence they have an impact on healthcare costs [6, 7]. Approximately 30% of children develop a lower respiratory tract infection within the first year of life; this decreases to less than 10% during early years of schooling and continue to decrease in preadolescent to healthy adult years [8, 9]. Patients in the intensive care unit and those who are mechanically ventilated have a higher risk of infection with these viruses because most of them have underlying chronic illnesses like cancer, hypertension and diabetes [10]. They are likely to be immunosuppressed either due to the underlying disease or due to chemotherapeutic agents they are using. Infection by these viruses therefore is likely to occur leading to poor prognosis, increased morbidity and mortality rate. This prolongs the length of hospital stay leading to increased economic burden to the individual and the hospital. Acute respiratory viral infections cause huge emotional and social burden on families and societies [11]. The matter will be more significant when the prevalence and complications due to these infections are well documented. These infections are usually neglected since they are not easily diagnosed as compared to bacterial infections. This problem can be managed by prompt diagnosis and the risk of exposure be assessed. In addition they also increase morbidity and mortality rates especially in patients with chronic illnesses and those who are immunosuppressed hence the need for their prompt diagnosis and treatment [12]. The objective of the study was to determine the prevalence of viral severe acute respiratory infections in patients in the intensive care unit and those under mechanical ventilation. The prevalence rate in patients will make an important understanding of additional respiratory viruse burdens that affect them and will contribute to their improved management and overall reduction in morbidity and mortality rates.
2. Materials and Methods
2.1. Study Area and Study Site
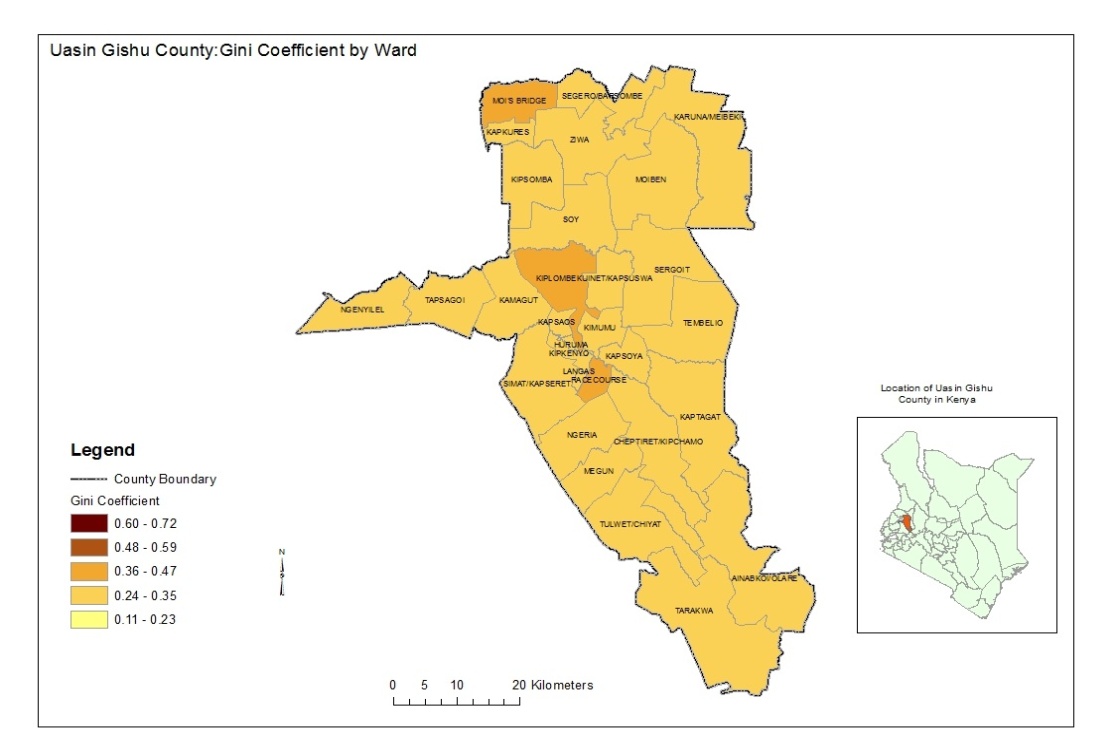
The study was done at Moi Teaching and Referral Hospital (MTRH), Uasin Gishu County in Kenya. Moi Teaching and Referral Hospital is located in Eldoret town; Uasin Gishu County in the mid-West of Kenya’s Rift Valley. It lies between Longitudes 340 50′ East and 350 37 West and Latitudes 00 03 South and 00 55 North (Kenya county guide, 2015). The population of this county stood at 894,179 as per the 2009 Population and Housing Census. It has a population growth rate of 3.8% and a population density of 267 persons per square Kilometer. The hospital has a bed capacity of 800 and receives patients from Uasin Gishu County, Nandi County, Pokot County, Turkana County, Tranzoia County, Elgeyo-Marakwet County, Bungoma County and other neighbouring regions like Eastern Uganda and South Sudan. The study population comprised of patients in the intensive care unit and those under mechanical ventilation who consented in the study regardless of their age.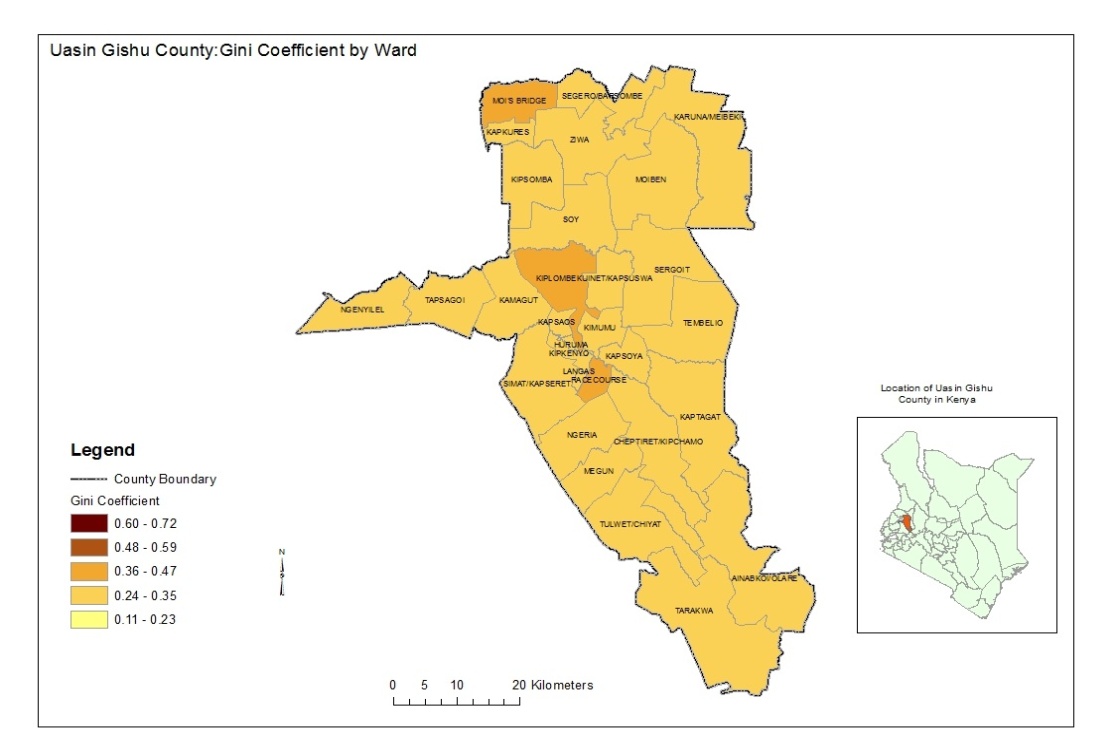 | Figure 1. Map of Uasin Gishu County (Source: Uasin Gishu county, 2016) |
2.2. Study Design
The study was a cross-sectional analytical, hospital based study where consented participants were tested for the presence of influenza, human Parainfluenza, Rhinovirus Adenovirus, Respiratory syncytial virus, Human metapneumovirus and Coronavirus using RT-PCR.
2.3. Sampling Technique and Sample Size Determination
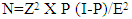
All patients in the intensive care unit and those under mechanical ventilation who consented were consecutively sampled. The sample size calculation was determined by the formula of [13] Fisher et al., 1998 based on 95% level of confidence and anticipated prevalence of 85.9%. The estimate in prevalence was based upon previous study in Thailand.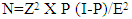 | (1) |
Where:N=Desired sample sizeZ=Standard normal deviation=1.96(from the tailed normal table).P=Incidence rate of viral respiratory infectionsE=the desired degree of accuracy at 95% confidence level=0.5N=1.962 X 0.859(0.141)/0.05=186 samples.Therefore 186 patients in the intensive care unit and those under mechanical ventilation at Moi Teaching Referral Hospital were involved.
2.4. Sample Collection
Broncho-alveolar washing/lavage was collected using standard bronchoscopy (Broncho-alveolar lavage) technique. The broncho-alveolar region was lavaged with normal saline; the specimen was then collected in a clean specimen container. Virus transport media was added immediately after collection in a volume equal to the specimen collected. Each container was then labeled with patient’s number and site source. The specimen was stored at 4°C in the lab and during transport to KEMRI Nairobi where analysis was done.
2.5. Laboratory Analysis
Sample analysis was carried out using the Protocol for One Taq® 2X Master Mix with Standard Buffer (M0482).
2.6. Protocol for cDNA Synthesis (Applied Biosystems™ Kit)
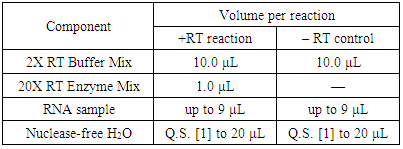
Approximately 2 μg of total RNA per 20-μL reaction was used. The reagent kit components were allowed to thaw on ice and then the volumes required were calculated depending on the required number of reactions. The RT reaction mix was aliquoted into tubes and sealed with the appropriate seal and then centrifuged to spin down the contents and to eliminate any air bubbles. The tubes were placed on ice until the reverse transcription reaction was ready to begin then followed by Incubation at 37°C for 60 minutes. The reaction was stopped by heating to 95°C for 5 minutes and holding at 4°C then stored at -25°C.Table 1. cDNA synthesis reaction components
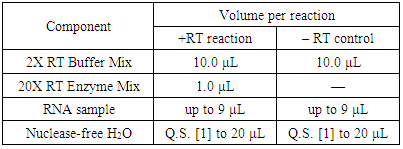 |
| |
|
2.7. Protocol for One Taq® 2X Master Mix
The reaction components were assembled on ice and transferred to thermocycler preheated to the denaturation temperature (94°C) then transferred to a sterile PCR tube, mixed gently and centrifuged to obtain the liquid. The PCR tubes were then transferred to a PCR machine for thermocycling. Denaturation was performed for 30 seconds at 94°C to amplify the targets from pure DNA template then annealing was done for 60 seconds at 45°C.
2.8. Data Analysis
The quantitative data was coded and analyzed using percentages, means and standard deviations while inferential statistics (correlation) was used to make conclusions. Analysis of variance (ANOVA) was used to aid in coding, entry and analysis of data. Viral test results were log-transformed to ensure normal distribution of the data and expressed as mean±standard deviation. Comparison of the viral type based on the sex of the patient and ward type was determined using ANOVA with Bonferroni’s post-test using GenStat Release 14.1 (PC/Windows).
2.9. Ethical Consideration
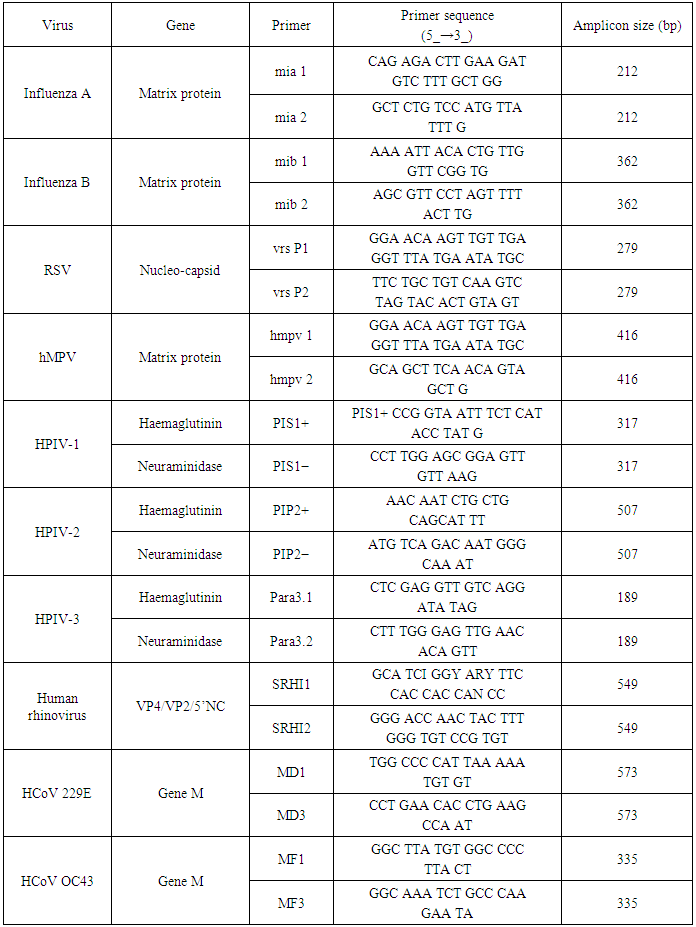
All patients gave informed written consent. The study was approved by institution research and ethics committee (IREC) and Moi Teaching and referral Hospital. The information obtained was treated with confidentiality. Codes were used instead of names on patient’s details.Table 2. Primer sequence of the respiratory viruses
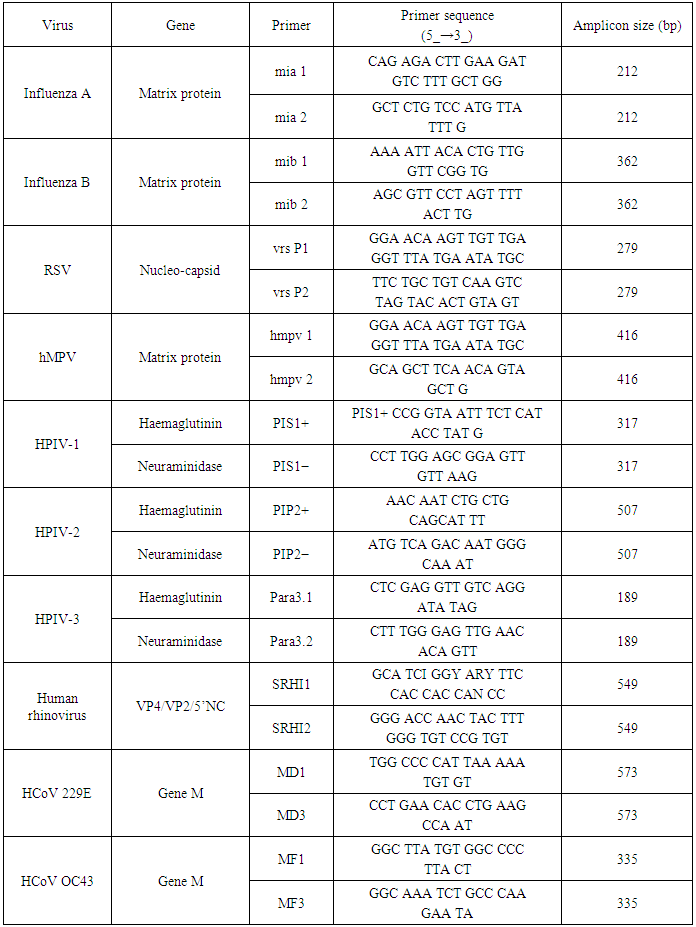 |
| |
|
3. Results
3.1. Demographic Characteristics of the Study Population
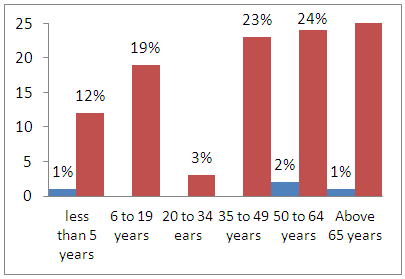
Age and gender of the study population was captured to help investigate variations in prevalence of viral severe acute respiratory infections among various age groups and gender. Majority of individuals in the study population were in the age bracket above 65 years representing 28.8% of the study population. Individuals in the age group 50 to 64 years, 35 to 49 years, 5 to 19 years and less than 5 years represented 24.4%, 20%, 13% and 11% respectively. Individuals in the age group of 20 to 34 years were the minority representing 3% of the study population. These age categories are relevant in this study because most studies done in the past have focused on the elderly and children below five years. This study has captured the trend of these infections across all age groups. Majority of the study population were male representing 57.2% of the population that was involved in the study and 42.3% were female.
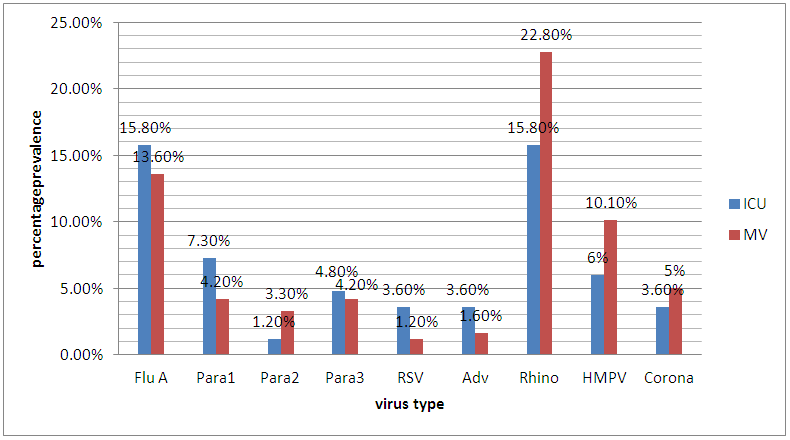
3.2. General Prevalence of Viral Infections in ICU and MV
The percentage prevalence of the different viruses in ICU and MV are presented in figure 2. Generally all the viruses that were analyzed had higher prevalence in patients in ICU except para 2 and HMPV which had higher prevalence in MV. Percentage prevalence of Flu A, para 1, para 2, para 3, RSV, adenovirus, Rhinovirus, HMPV, coronavirus and was 15.8%, 7.3%, 1.2%, 4.8%, 3.6%, 3.6%, 15.8%, 6.0%, and 3.6% in ICU and 13.6%, 4.2%, 3.3%, 4.2%, 1.2%, 1.6%, 22.8%, 10.1% and 5.0% in MV respectively.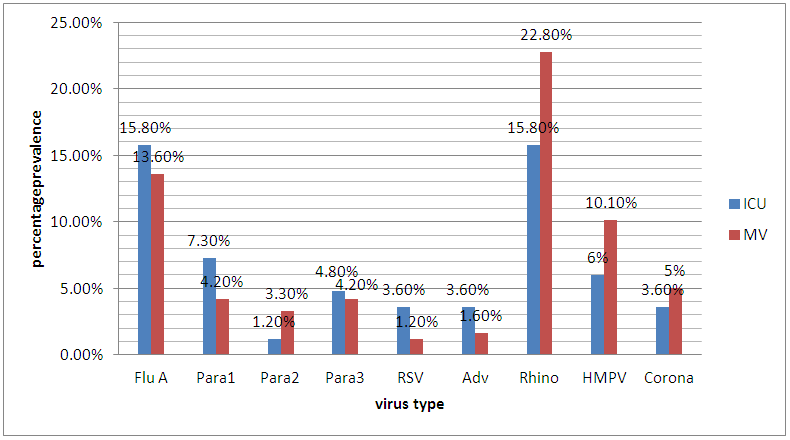 | Figure 2. General prevalence in ICU and MV |
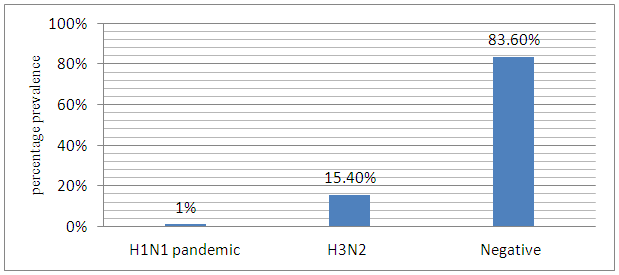
3.3. Prevalence of Influenza A
The prevalence of Influenza A virus subtypes are presented in figure 3. Out of the Total samples analyzed, only 1% of the patients tested positive for H1N1 pandemic, while 15.4% tested positive for H3N2.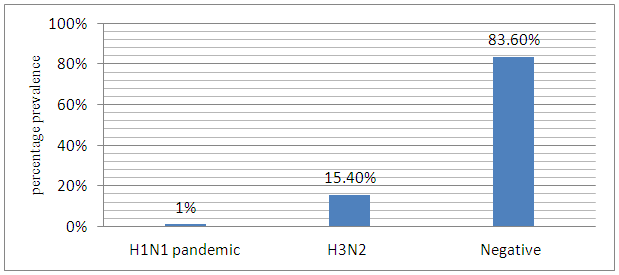 | Figure 3. Prevalence of Influenza A virus Subtypes |
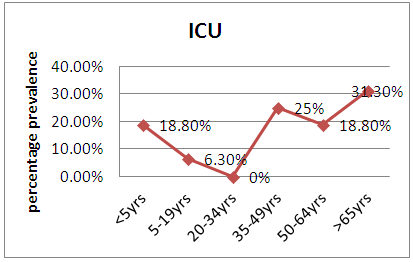
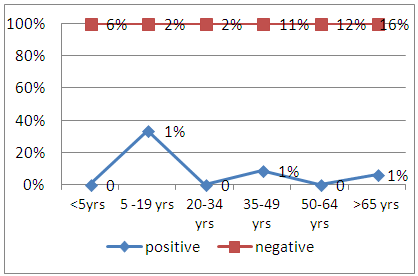
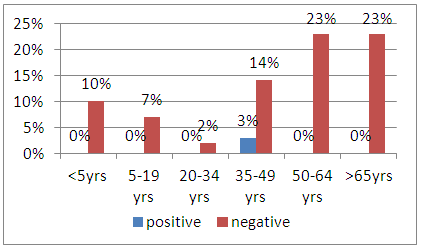
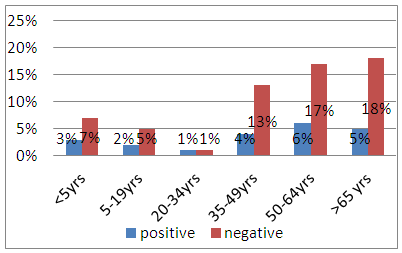
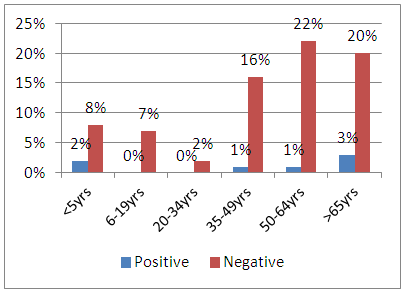
3.3.1. Prevalence of Flu A in ICU and MV in Relation to Age
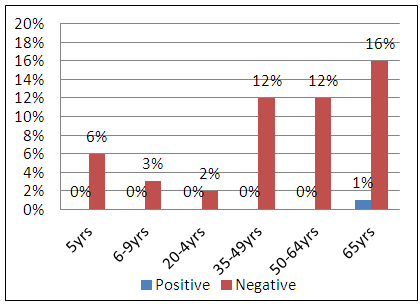
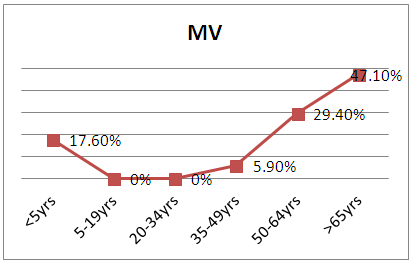
The results for the prevalence of Flu A virus in ICU and MV patients in the different age groups are represented in figure 4. (a) and (b). In ICU, patients in age groups above 65 years, 35 to 49, years, 50 to 64 years, less than 5 years, and 5 to 19 years had a prevalence infection of 31.3%, 25%, 18.8%, 18.8%, 6.3%% respectively. No infection was observed in age group 20 to 34 years. In MV, patients in age group above 65 years, 50 to 64years, less than 5 years and 35 to 49 years had percentage prevalence of 47.1%, 29.4%, 17.6 and 5.9% respectively. No infection was observed in both age group 5-19 and 19 to 34 years.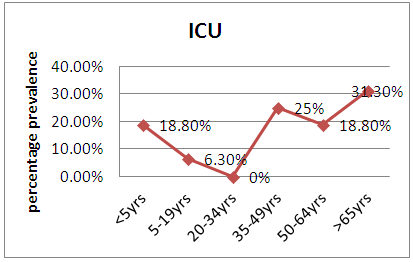 | Figure 4(a). Prevalence of influenza A in ICU |
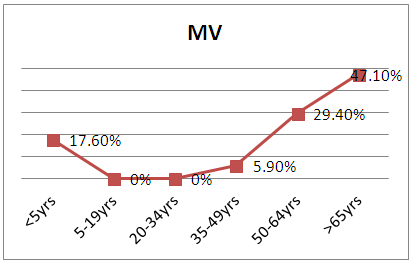 | Figure 4(b). Prevalence of influenza A in MV |
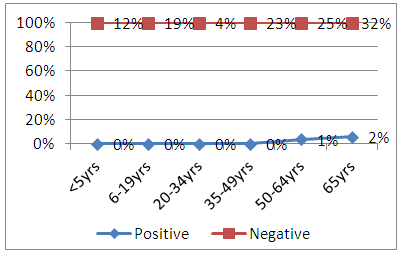
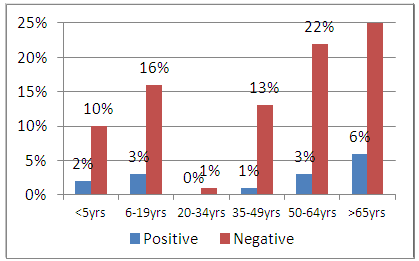
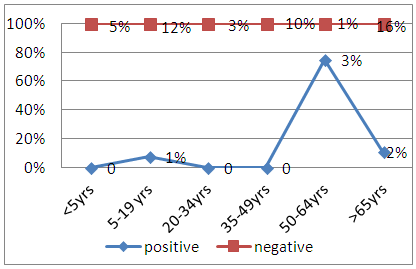
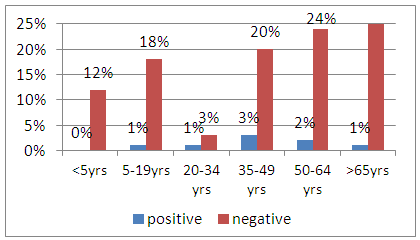
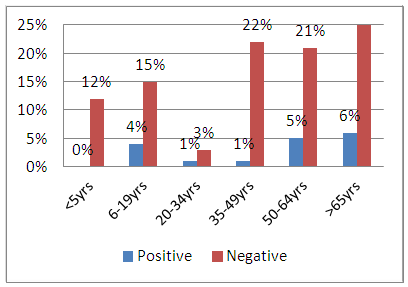
3.4. Parainfluenza 1 in ICU and MV
The results for the prevalence of Parainfluenza 1 virus infection in patients ICU and MV in the different age ranges are represented in figure 5.(a) and (b). In ICU, 2% of the patients were infected in the age range 5-19yrs whereas 1% of patients were infected in both age range 35-49 and >65years. No infection was recorded in age ranges <5, 20-34 and 50-64 years. In MV, patients in age range 50-64years, >65 years and 5-19 years were infected with parainfluenza 1 virus with percentage prevalence of 3, 2 and 1 respectively. None of the patients were infected with parainfluenza virus in patients in age ranges <5years, 20-34 years and 35-49 years.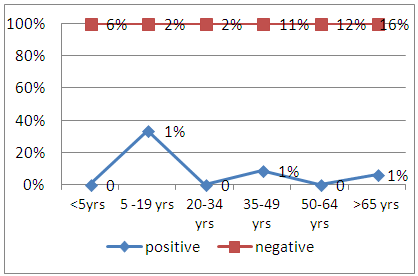 | Figure 5(a). Parainfluenza 1 virus in ICU |
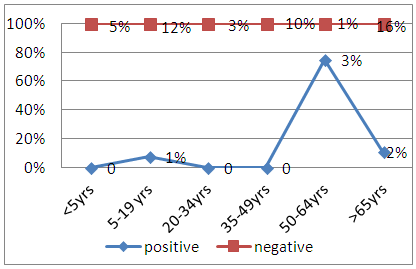 | Figure 5(b). Parainfluenza 1 virus in MV |
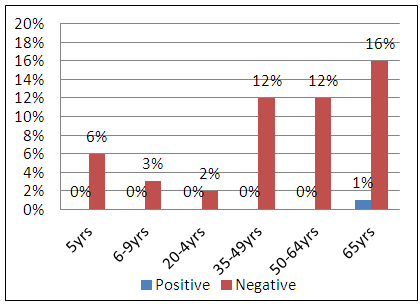
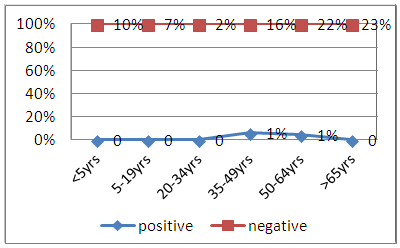
3.5. Parainfluenza 2 Virus in ICU and MV
The results on the prevalence of parainfluenza 2 in MV and ICU in the different age groups studied are represented in Figure 6 (a) and (b). In MV, Patients in the age range >65 years had a percentage prevalence of 2, while patients in age range 5-19 years and 35-49 years had a percentage prevalence of 1. None of the patients in age range <5, 20-34 and 50-64 were infected with Parainfluenza 2. In the intensive care unit, the only age group that was affected was >65 years with a 1 percent infection rate.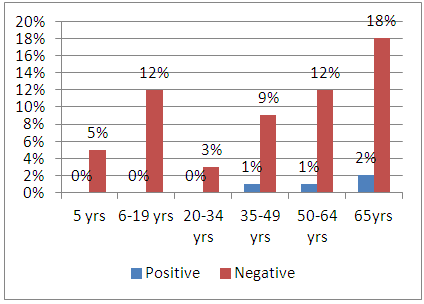 | Figure 6(a). Parainfluenza 2 virus in MV |
 | Figure 6(b). Parainfluenza 2 virus in ICU |
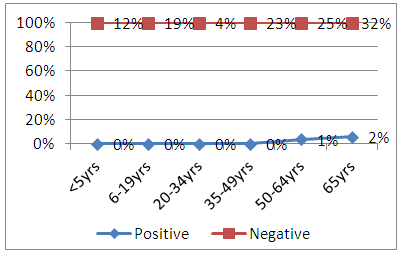
3.6. Parainfluenza 3 Virus in ICU and MV
The results for the prevalence of Parainfluenza 3 virus both in ICU and MV patients in the different age groups are represented in Figure 7 (a) and (b). Infection was recorded in patients in the age range of 35-49 with a 3 percent infection rate in ICU. In MV, a 3 percent and 2 percent prevalence was recorded in patients in the age range of 35-49 and 50-64 respectively while in age ranges 5-19, 20-34 and >65, a 1 percent prevalence was recorded. No infection was observed in age range <5 years.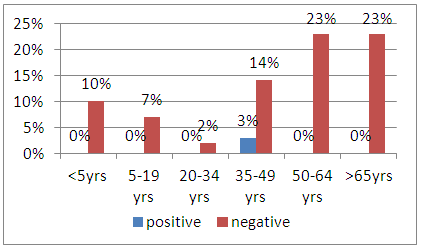 | Figure 7(a). Parainfluenza 3 in ICU |
 | Figure 7(b). Parainfluenza 3 in MV |
3.7. Adenovirus in ICU and MV
The results for the prevalence of Adenovirus in ICU and MV in he different age groups are represented in Figure 8(a) and (b). In ICU, a 2 percent and 1 Percent prevalence was recorded for the age ranges>65 and 50-64 years respectively. No infection was observed in age group <5, 5-19, 20-34 and 35-49 years. In MV, Percentage infection rate of 1 percent was recorded in both age groups35-49 years and 50-64 years.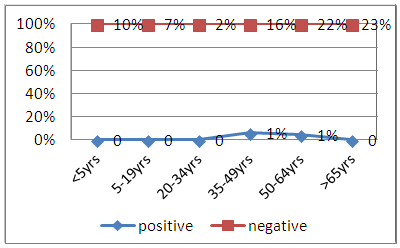 | Figure 8(a). Adenovirus in ICU |
 | Figure 8(b). Adenovirus in MV |
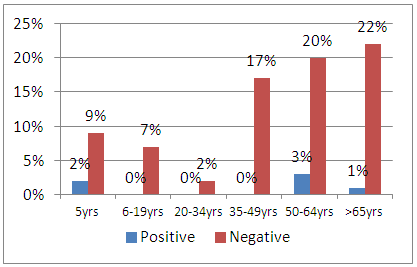
3.8. Rhinovirus in Relation to Age in ICU and MV
The results for the prevalence of Rhinovirus in patients in ICU and MV in the different age groups are represented in Figure 9 (a) and (b). In ICU; rhinovirus affected all the age groups. Percentage prevalence in age range 50-64, >65, 35-49, <5 and 20-34 years were 6%, 5%, 4%, 3%, 2% and 1% respectively. In mechanical ventilation, patients in age range above 65 years had the highest prevalence of 4% while those in age range 20-34 years had a prevalence of 1%. No infections were reported in age range <5, 5-19, 35-49 and 50-64 years.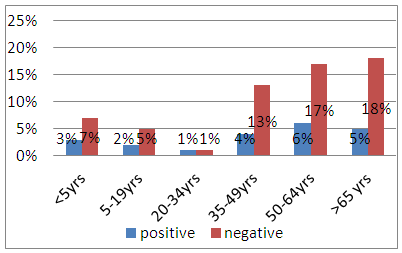 | Figure 9(a). Prevalence of Rhinovirus in ICU |
 | Figure 9(b). Prevalence of Rhinovirus in MV |
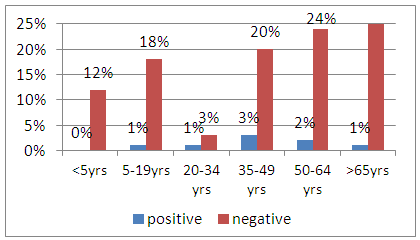
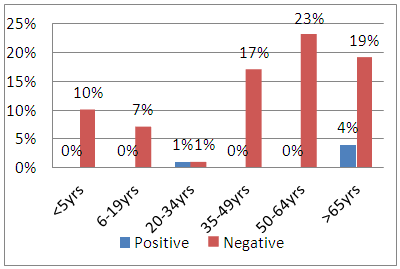
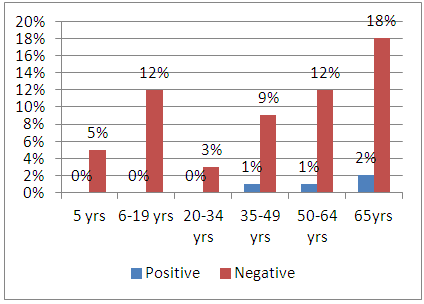
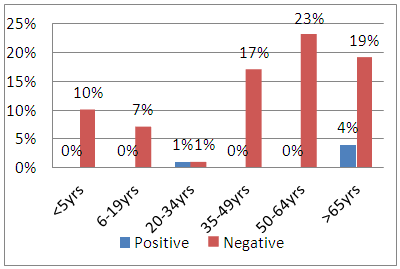
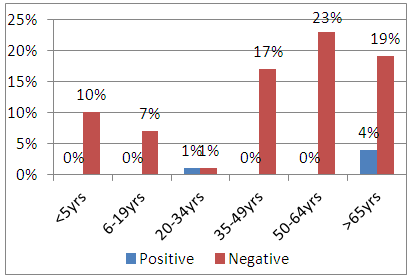
3.9. Respiratory Syncytial Virus in ICU AND MV
The results for the prevalence of Respiratory syncytial virus in patients in ICU and MV in the different age groups are represented in figure 10 (a) and (b). Percentage prevalence in age range 50-64, <5 and >65 years was 3%, 2% and 1% respectively in ICU patients. No infection was reported in both age range 20-34 and 35-49 years. In MV, patients in age range <5, 6-19, 50-64 and 35-49 years had percentage prevalence of 5, 3, 3 and 1 respectively. No infection was reported in age range 20-34 years. 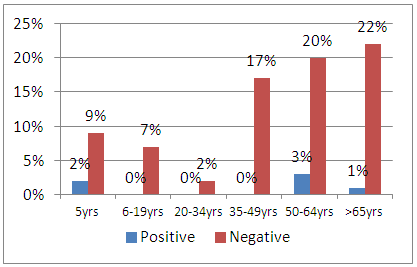 | Figure 10(a). Prevalence of RSV in ICU |
 | Figure 10(b). prevalence of RSV in MV |
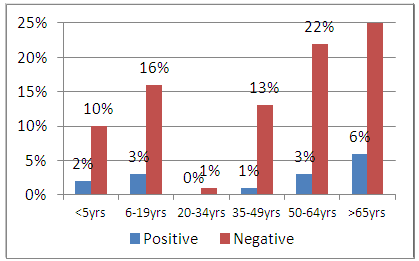
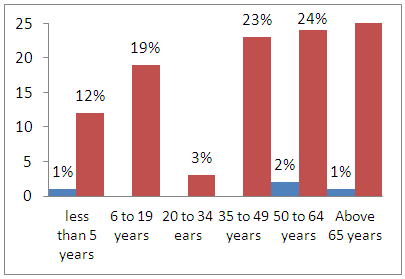
3.10. Human Metapneumovirus in ICU and MV
The results for the prevalence of metapneumovirus in patients in ICU and MV in the different age groups are represented in figure 11 (a) and (b). In ICU, patients in age range>65 and <5 years had a percentage prevalence of 3 and 2 respectively while those in age range 35-49 and 50-64 both had 1% prevalence. Patients in age range 5-19 and 20-34 years were not infected. In patients under mechanical ventilation, a percentage prevalence of 6, 5 and 4 were recorded in age range >65, 50-64 and 5-19 years respectively, while in both age range 20-34 and 35-49 years, a 1% prevalence was recorded. Patients in age range <5 years were not infected.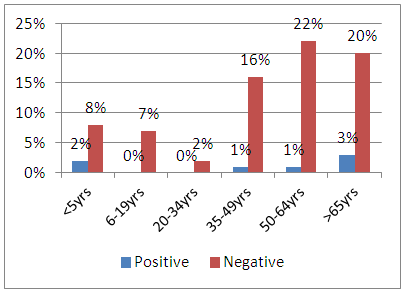 | Figure 11(a). Prevalence of HMPV in ICU |
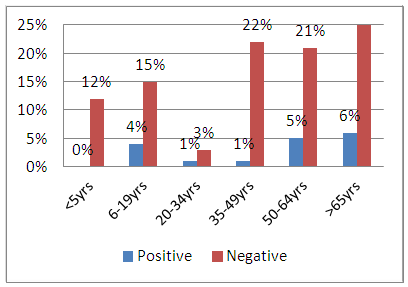 | Figure 11(b). Prevalence of HMPV in MV |
3.11. Prevalence of Coronavirus in ICU and Mv
The results for the prevalence of coronavirus in patients in ICU and MV in the different age groups are represented in figure 12 (a) and (b). The prevalence of coronavirus among ICU patients in the age range 20-34 and above 65 years was 1% and 4% respectively while patients in the other age range were not infected. The prevalence of coronavirus among patients in both age range <5 and >65 years in MV was at 1%, while those at age range 50-64 years was at 2%. The rest of the age groups were not infected.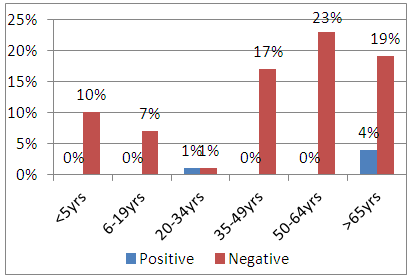 | Figure 12(a). Prevalence of Coronavirus in ICU |
 | Figure 12(b). Prevalence of Coronavirus in MV |
4. Discussion
Severe acute respiratory tract infections are an underestimated cause of illness in all age groups. Improvements in diagnosis of these infections over the past has shown that viral respiratory tract infections are associated with significant rates of morbidity and mortality comparable to those seen with bacterial community acquired and nosocomial pneumonia [14]. According to [15] Flu A, RSV, PIV types 1–4, rhinovirus, and adenovirus was detected in children below 5 years. RSV was the most common in 18% of 685 samples obtained from patients with respiratory tract Infections (RTI), and hMPV was the second most common viral pathogen, in 48 (7%) from patients with RTI. hMPV was the most detected than human Parainfluenza (9, 2, 7, and 0 samples were positive for PIV types 1–4, respectively), adenovirus (8 samples), rhinovirus (28 samples), and Flu A and B (11 and 7 samples, respectively). From this study the number of positive samples was 33, 12, 8, 11, 19, 5, 42, 22, and 9 for Influenza A, PIV1, 2, 3, RSV, Adenovirus, Rhinovirus, HMPV and Human coronavirus respectively. Influenza virus causes seasonal epidemics, especially during the winter months with an average annual mortality rate of only 1.4 to 16.7 deaths per 100 000 persons. Increased mortality occur in adults >65 years of age. ICU admissions are relatively common. One observational study performed over a 3-year time period estimated that 8% of ICU admissions for unspecified Lower Respiratory Tract Infections (lrti) were related to influenza infection [16]. There is similarity with the findings in this study where a prevalence of 15.6% was recorded for H3N2 and 1% for H1N1 pandemic. Rhinovirus is also a major cause of viral upper respiratory tract infection and LRTIs in immune-compromised patients that require ICU care. In a study of adults admitted to the ICU with acute respiratory failure, 9% tested positive for rhinovirus. In a retrospective study of immune-compromised individuals requiring ICU care with acute respiratory failure, rhinovirus infections associated case fatality approached 30%, this is similar to the case fatality rate observed during the 2009 H1N1 influenza pandemic [17]. This is comparable with this study where rhinovirus accounted for 15.8% of all the infections in the ICU. Coronavirus infections are usually self-limiting and cause upper respiratory symptoms. It is a cause of severe LRTI in elderly adults. Because of different testing techniques accurate estimates of the annual incidence and prevalence of coronavirus infections are not well documented. Approximately 7% of immune competent adults admitted to the ICU with acute respiratory failure may have coronavirus infections [18]. This study recorded a prevalence of 3.6% and 5.0% for Human Coronavirus in ICU and MV respectively. It is evident that RSV occurs in 2% to 6% of patients admitted to the ICU with acute respiratory failure. Mortality in patients with RSV infections is as high as 12%. The findings in this research are comparable to studies performed in developed countries, where RSV is considered the main viral agent of lower respiratory tract infections, with rates of 5 to 40% in cases of pneumonia [19]. From this study, the study population aged less than five years recorded a prevalence of 2% for HMPV in ICU, 2% RSV in both ICU and MV, 3% Rhinovirus in ICU and 1% Parainfluenza 1 in ICU, this is comparable with a study of 78 children less than five years with acute respiratory failure under mechanical ventilation where nosocomial infection with viral etiology was identified in 29.5%, RSV was found in 14.1%, followed by influenza A virus at 10.2% [20].The impact of disease due to these viral respiratory pathogens in the elderly is increasingly being recognized. For instance, Influenza and RSV are the leading cause of viral lower respiratory illness (LRI). In addition, other viruses have been included in the list of significant pathogens in the elderly; these include Parainfluenza (PIV), human rhinoviruses, coronaviruses, and human metapneumovirus (hMPV). These viruses are responsible for 13 to 31% of LRI in elderly adults [21]. In this study there was significant prevalence in the elderly both in ICU and MV. For instance rhinovirus recorded a prevalence of 5%, RSV 6%, HMPV 6% in study subjects above 65 years. PIV 1, 2, 3 and adenovirus recorded a prevalence of 2% each in the same age category of above 65 years.
5. Conclusions and Recommendations
From this study the results indicate that viral respiratory tract infections are prevalent in patients both in the intensive care unit and those under mechanical ventilation in the general wards at Moi Teaching and Referral Hospital. It is evident that the infections occur across all age groups; however children less than 5 years and the elderly above 65 years recorded a higher prevalence in most viral infections as compared to other age groups. Viral nosocomial infections have long been underestimated but it is clear from this study that these infections should not be underestimated as they lead to increased morbidity and mortality in our healthcare facilities. Continues surveillance is needed to help understand the trends of infection by these respiratory viruses and other emerging viruses. More studies needs to be done especially in this group of patients and also other patient groups like those with chronic diseases like cancer, diabetes, hypertension and those who are immunosuppressed in our hospital set ups.
ACKNOWLEDGEMENTS
We are grateful to Moi Teaching and Referral Hospital and Kenya Medical Research Institute for their input in this project. We thank Mr. Ben Kiptorgor, Samuel Symekher and Edwin mutai who assisted in sample collection, sample analysis and data analysis respectively.
References
| [1] | Ryland et al., (2011). Complications of mechanical ventilation. |
| [2] | Balmes et al., (2003). American occupational contribution in airway diseases, thoracic Society, www.thoracic.org, (2003). |
| [3] | Dominic et al., (2000). Intensive Care Unit (ICU) Overview. |
| [4] | Berger et al.,. (2009). Prospective population-based study of RSV-related intermediate care and intensive care unit admissions in Switzerland over a 4-year period (2001–2005). Infection.2009; 37: 109–116. |
| [5] | Matías et al., (2015). Trends of Respiratory Syncytial virus infections in children under 2 Years of Age in Puerto Rico. P R Health Sci J. 2015 Jun;34(2):98-101. |
| [6] | Hall, B. (2001). Respiratory syncytial virus and parainfluenza virus. N Engl Journal Med; 344: 1917-28. |
| [7] | Fransen et al., (1969). Infections with viruses in patients hospitalized with acute respiratory illness, Scand Journal Infect Disease; 1: 127-36. |
| [8] | Emelda et al., (2012). The Incidence and Clinical Burden of Respiratory Syncytial Virus Disease Identified through Hospital Outpatient Presentations in Kenyan Children. |
| [9] | Omballa et al (2012). Incidence and subtypes of Human metapneumovirus among Selected rural and urban Populations of Kenya, 2006-2009. |
| [10] | Nair et al., (2010). Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010; 375: 1545–1555. |
| [11] | Mullins et al., (2004). Human metapneumovirus infection among children hospitalized with acute respiratory illness, Emerg Infect Dis.10: 4; 700-705. |
| [12] | Scott et al., (2008). Pneumonia research to reduce childhood mortality in the developing world, J Clin Invest 118: 4: 1291-1300. |
| [13] | Fisher et al., (2004). Sample size determination for different study designs in medical Research. |
| [14] | Christopher et al., (2015). Viral respiratory infections of adults in the intensive care unit. |
| [15] | Bernadette et al., (2003). Prevalence and clinical symptoms of Human Metapneumovirus infection in hospitalized patients The Journal of Infectious Diseases, Volume 188, Issue 10, Pages 1571–1577. |
| [16] | Daubin et al., (2005). Nosocomial viral ventilator-associated pneumonia in the intensive care unit: a prospective cohort study. Int Care Med. 2005; 31(8): 1116–1122. |
| [17] | Karhu et al., (2014). Lowe respiratory tract virus findings in mechanically ventilated patients with severe community-acquired pneumonia. Clin Infect Dis.; 59(1): 62-70. |
| [18] | Legoff et al., (2005). A. High prevalence of respiratory viral infections in patients hospitalized in an intensive care unit for acute respiratory infections as detected by nucleic acid-based assays. J Clin Microbiol.;43(1):455-457. |
| [19] | Anderson et al., (1990). Association between respiratory syncytial virus outbreaks and lower respiratory tract deaths of infants and young children. J. infect. Dis., 161: 640-646. |
| [20] | Edna et al., (2005). Incidence of respiratory viruses in preterm infants submitted to mechanical ventilation. |
| [21] | Talbot et al., (2010). The diagnosis of viral respiratory disease in older adults. Clin Infect Dis. Mar 1;50(5):747-51. doi: 10.1086/650486. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML