-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Tumor Therapy
p-ISSN: 2163-2189 e-ISSN: 2163-2197
2018; 7(1): 34-37
doi:10.5923/j.ijtt.20180701.03

Endoscopic Miniinvasive Alternative Treatment Methods for Disseminated Cancer of the Thoracic Esophagus
F. G. Nazirov, M. I. Davidov, Z. M. Nizamkhodjaev, O. M. Gulamov, F. U. Muzaffarov, L. P. Strusskiy
Republican Specialized Scientific-Practical Centre of Surgery, named after Academician V. Vakhidov, Tashkent, Uzbekistan
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to the actual problem - miniinvasive surgical treatment of patients with disseminated cancer of the thoracic esophagus, discussion of modern treatment tactics for this pathology, estimation of the possibilities of new techniques. The analysis of indications, volume and minimally invasive manipulations at the treatment of esophageal cancer in accordance with the localization and the process prevalence was carried out.
Keywords: Esophageal cancer, Esophageal stenting, Gullet bougienage
Cite this paper: F. G. Nazirov, M. I. Davidov, Z. M. Nizamkhodjaev, O. M. Gulamov, F. U. Muzaffarov, L. P. Strusskiy, Endoscopic Miniinvasive Alternative Treatment Methods for Disseminated Cancer of the Thoracic Esophagus, International Journal of Tumor Therapy, Vol. 7 No. 1, 2018, pp. 34-37. doi: 10.5923/j.ijtt.20180701.03.
1. Introduction
- The methods of chemotherapy and radiation therapy take a special place in the complex treatment for pathologic growth impairment and prevention of disseminated esophageal cancer’s spread [1-2, 7]. In majority of cases a surgical treatment in the early stage of oncologic diseases allows to get a successful outcome in the patients with esophageal cancer for a long time [1-4, 10, 12]. Anatomical position of esophageal cancer stipulates the risk of esophageal anastomosis sutures inefficiency in the early postoperative period and the absence of adequate feeding in such cases leads to the accelerated alimentary failure. Alimentary cachexia makes any surgical intervention be impossible without the risk of severe patients’ life [9, 11]. The performance of radical surgeries is provided at verified esophageal cancer. Radical surgeries are impossible at the following conditions: late stages of esophageal cancer with the signs of tumor dissemination; at the presence of esophago-organ fistulas; at the dissemination to lymph nodes; at the shift of tumor to the other organs; at the patient’s cachectic physical condition with inefficiency of plastic organs-donors for performing radical surgeries [5-6].The patients with neglected esophageal cancer mainly suffer from dysphagia and a total absence of esophageal obstruction, a chronic hunger bereaves their hope for recovery and life. From our point of view, endoscopic alternative methods can alleviate this fate and increase patients’ life quality.
2. Aim
- To validate a performing of endoscopic alternative methods for correction of dysphagia and recovery of esophagus patency in patients with disseminated cancer of the esophagus thoracic part.
3. Material and Methods
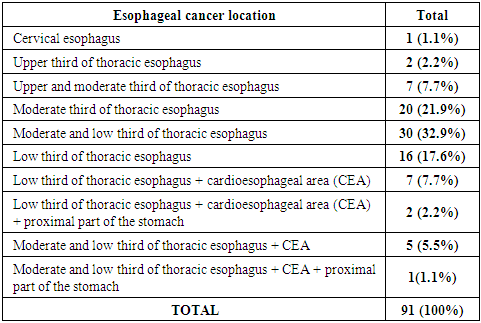
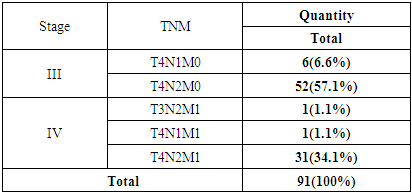
- The total number of patients diagnosed with irresectable stages of the thoracic esophagus cancer was 91. There were 61 males and 30 females. The patients age ranged from 39 to 78 years. All the patients have been treated in our Centre between 2007 and 2018. Esophageal cancer was diagnosed by standard diagnostics methods and histologic verification. The disease stage was defined subject to: the beginning of pathologic process, the estimation results of high-precision diagnostic methods and while performing surgical interventions. Cancer of the thoracic esophagus and cardioesophageal area (CEA) was revealed by endoscopy results: in upper third - 9 (9.9%) cases; in middle third – in 50 (54.9%) and in low third – in 15(16.5%) patients. The extent of esophageal cancer and lumen’s diameter practically in all cases made up critical digits: extent – 5-6 cm, lumen’s diameter 0.5-0.8 cm – in 50% of patients. Computer tomography is characterized by higher digits of diagnostics: sensitivity – 54.5%, specificity – 72.2% and accuracy – 82.8%. All the patients were performed MSCT or MRI because such investigations allow to determine distant metastases and invasion of the main process to the adjacent structures. A histologic verification of biopsy materials showed that a majority of patients (84 (92.3%)) were with epidermoid esophageal cancer of varied differentiation levels: highly differentiated carcinoma – in 53 (63.1%), moderate differentiated carcinoma – in 16 (19.0%) and low differentiated carcinoma – in 15 (17.8%). Adenocarcinoma was diagnosed in 16 (7.7%) patients.
|
|
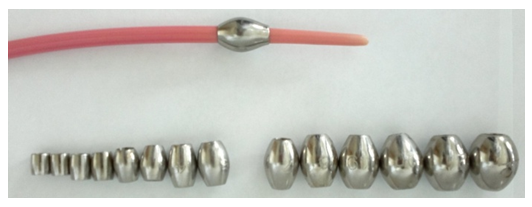 | Figure 1. The set of metal olives for endoscopic bougienage |
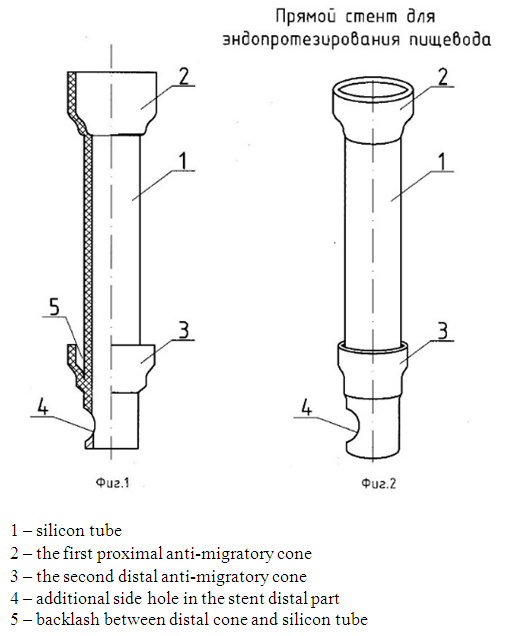 | Figure 2. The scheme of a direct stent for esophagus endoprosthesis replacement |
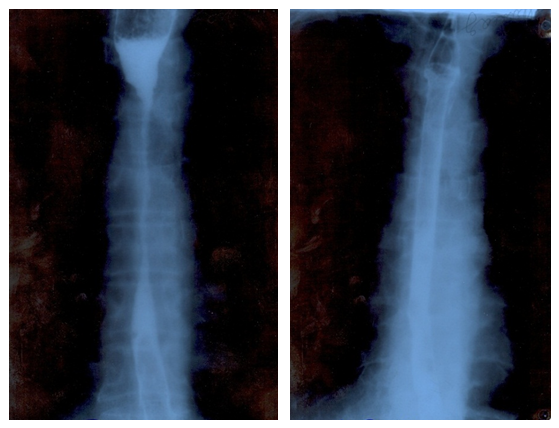 | Figure 3. X-ray pattern before and after stenting |
 | Figure 4. Self-expansible covered knitted nitinol esophageal stent |
4. Results and Analysis
- All 91 patients with III - IV stage of disseminated esophageal cancer had a severe dysphagia and a part of them had a complete esophageal obstruction. 23 of patients were performed only conservative therapy (intravenous infusion) due to the undermaintenance of pathologic process and their extremely severe condition. Endoscopic alternative interventions were not performed due to the following reasons: total absence of esophageal lumen on the cancerous lesion level, ulceration, hemorrhagic diathesis, tumor tissue destruction, evident pain syndrome, a high risk of hollow organ wall’s injury. The rest of 68 patients were performed various interventions: in 3 – shunt esophagocoloplasty; in 19 cases we carried out gastrostomy; in 28 cases the surgery was completed by exploration; 46 patients were performed diathermotunnelization, gullet bougienage and esophagus endoprosthesis replacement. Hard standard bougies in rising order and the probes with changeable olives were used. At the occurrence of evident pain syndromes and evident resistance the procedure was suspended for several days. The gullet bougienage was performed for achieving the most optimal patency before endoprosthesis replacement. All 68 (74.7%) patients undergone endoscopic interventions were performed endoprosthesis replacement (including 28 cases with exploration). We used two types of prosthetic devices for esophageal cancer: the first device above described was developed and offered by our group of researchers and they were used in 45 (66.17%) cases.The second type of prosthetic devices are Ni-Ti (China) and TaeWoong Medical (South Korea) was used in 23 (33.8%) patients.Esophageal cancer prosthetics at its location in the cervical part cannot be performed because timorous strictures of esophagus cervical part are situated close to the crico-pharyngeal muscle. We carried out gastrostomy at the impossibility of performing endoprosthesis replacement. The control with the use of X-ray contrast was carried out after endoprosthesis replacement for estimation of prosthetic device location in the esophageal lumen and its patency, the level of the device proximal and distal ends. The patients were discharged home after receiving good results to be observed by oncologist. Hereby, from the total quantity of patients (91) in 23 cases the treatment was limited by conservative therapy due to the patients severe condition and impossibility of the surgery. In 3(3.29%) cases we performed shunt esophagocoloplasty, gastrostomy – in 19(20.8%) patients. 28(30.7%) among 46 (50.5%) patients were earlier performed exploration and then in all 46 (50.5%) patients we performed endoscopic alternative method as an adequate treatment.
5. Conclusions
- Esophageal cancer of III-IV stage in 72% of cases is disseminated and its course in all cases is complicated by severe dysphagia or a complete esophageal obstruction. Endoprosthesis replacement is effective in 50.57% of patients at unresectable disseminated esophageal cancer with a location in the moderate or low third of the esophageal thoracic part and it is a method of choice for the treatment of such patients type. Gastrostomy is the only method for enteral feeding in the patients with disseminated esophageal cancer of the upper third or esophagus cervical part.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML