-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Tumor Therapy
p-ISSN: 2163-2189 e-ISSN: 2163-2197
2014; 3(2): 21-24
doi:10.5923/j.ijtt.20140302.01
Pure Choriocarcinoma of Testis with Scleral Metastasis
Ujwala Gunnal MD, Avantika Chenna MD, Chidiebere Maquincy Ibekwe MD, Myra Rose MD
Morehouse School of Medicine 720 Westview Drive, Atlanta Georgia 30310
Correspondence to: Ujwala Gunnal MD, Morehouse School of Medicine 720 Westview Drive, Atlanta Georgia 30310.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Pure choriocarcinoma of testis is a rare germinal tumor which accounts for less than 1 % of all testicular tumors. Choriocarcinoma is one of the most aggressive tumors in young men with tendency for early metastasis. Most common sites of metastasis include lung, liver, brain, bone and retroperitoneal lymph nodes [1]. Ocular metastasis from Choriocacinoma is uncommon and most importantly metastasis to sclera is very rare. Per our literature review so far, this is the first reported case of its kind.
Keywords: Choricarcinoma, Metastasis, Sclera
Cite this paper: Ujwala Gunnal MD, Avantika Chenna MD, Chidiebere Maquincy Ibekwe MD, Myra Rose MD, Pure Choriocarcinoma of Testis with Scleral Metastasis, International Journal of Tumor Therapy, Vol. 3 No. 2, 2014, pp. 21-24. doi: 10.5923/j.ijtt.20140302.01.
1. Introduction
- Testicular tumors are most common malignancies in men aged 15-35 years and account for about 1-1.5% of all tumors [1]. Pure choriocarcinoma of testis is a rare germinal tumor which accounts for less than 1 % of all testicular tumors. Most common sites of metastasis include lung, liver, brain, bone and retroperitoneal lymph nodes [1]. Ocular metastasis from choriocarcinoma is uncommon and most importantly metastasis to sclera is very rare. Per our literature review so far, this is the first reported case of its kind.
2. Case Description
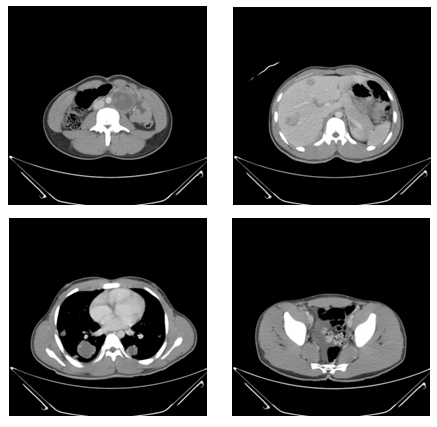
- A 20 year old male with no significant past medical history presented with 2 weeks history of gradually enlarging painless left testicular mass with associated lower back pain. Three days prior to presentation, he reported history of haziness, decreased peripheral vision in left eye which progressed to include central vision loss with associated floaters. The patient denied any flashes, eye pain, redness, discharge or headache. He denied any history of Human immunodeficiency virus (HIV), other sexually transmitted diseases, trauma to testis, history of cryptorchidism or family history of cancer. Social history was negative for smoking, alcohol or illicit drug use. Review of symptoms was positive for fatigue, weight loss and night sweats. Initial vital signs were, blood pressure – 120/52millimeters of mercury, heart rate – 92 per minute, Respiratory rate- 18 per minute, pulse oximetry -99 %. Physical exam was significant for 9 x 6 centimetre’s mass in the left testis with normal right testis and no inguinal lymphadenopathy. Visual acuity in right eye was 20/20 and left eye was 20/800. Fundoscopy was significant for large intraorbital lesion surrounded by fovea medially and at the superior arcade, elevated retina with change in pigmentation and subretinal fluid along the edges of the lesion. Initial labs were significant for Hemoglobin 9.6 grams per decilitre(g/dl) (13.5 – 17.5 g/dl), WBC 12.8 (4.5-11k/mcl ), Platelet count 342 (140-440k/mcl), sodium 131 (132-144meq/L), Aspartate aminotransferase 34 U/L(10-42), Alanine aminotransferase 29 Units per litre(U/L) (17-63), Bilirubin 0.6 mg/dl (0.3-1.6), Alkaline phosphate 90 U/L(38-126), Lactate dehydrogenase 786 U/L (91- 180), Alpha fetoprotein of 255 gm/ml(< 9) and Beta human chorionic gonadotropin of >1000mIU/ml, HIV and purified protein derivative were negative.Chest radiograph showed multiple round masses and nodules within bilateral lungs, consistent with metastatic disease. CT abdomen and pelvis showed large left testicular mass consistent with primary testicular malignancy and metastatic disease including cannonball lung metastases, liver metastases and retroperitoneal nodal metastases [Fig -2]. MRI of the brain and orbit showed multiple hemorrhagic areas consistent with metastatic disease in cortical and subarachnoid areas without mass effect. There was an ovoid mass within the posterior aspect posterior chamber of the left globe which measured approximately 1 cm x1 cm x 0.5 cm and attached to the sclera. There was some enhancement along the posterior aspect of the left globe adjacent to the lesion. There was no evidence of extra ocular involvement [Fig-1].
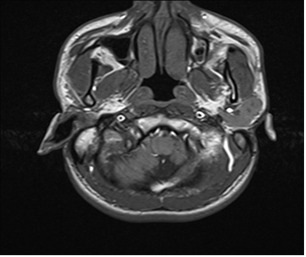 | Figure 1. MRI of brain including facial orbit and mass attached to sclera |
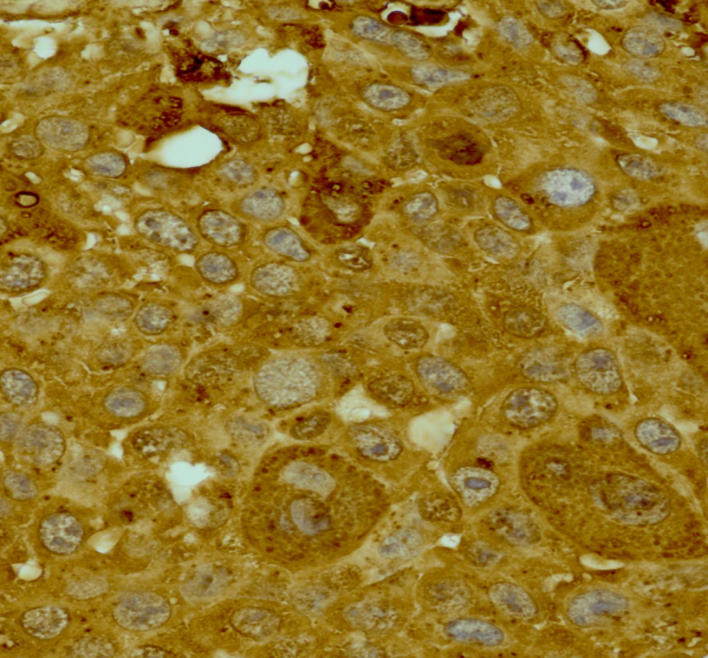 | Figure 3. Histopathological slide of Testis-cells are multinucleated with positive HCG, synctiotrophoblasts staining |
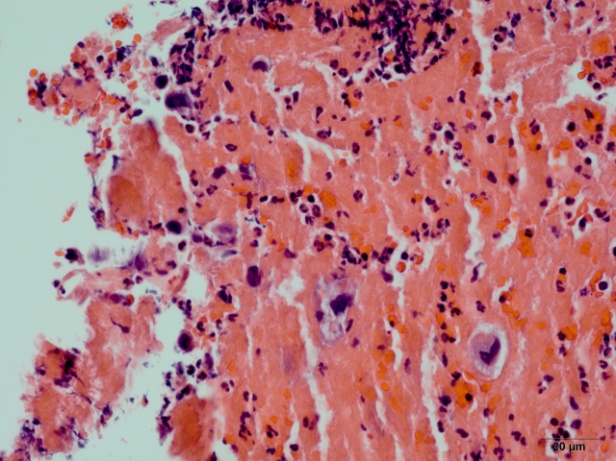
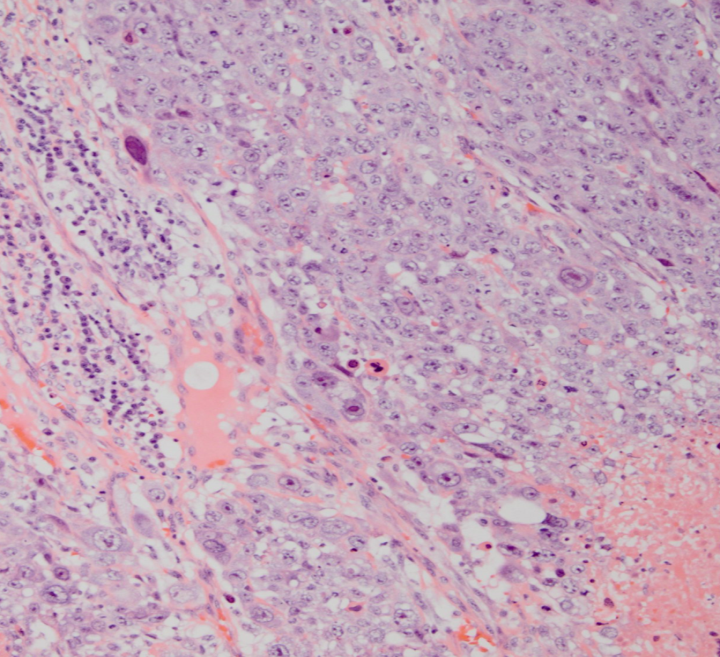 | Figure 4. Hematoxylin stained sheets of tumor cells with high grade malignant tumor with hemorrhage and multinuclei |
 | Figure 5. Multinucleated giant cells in the Jejunum with remnants of synctiotrophoblasts |
3. Discussion
- Testicular cancers are classified as germ cell and non-germ cell tumors per North American Standard Classification. [1]. As per histological classification, testicular germ cell tumors are divided into Seminoma, which resemble primordial germ cells (PGCs), and Non-Seminoma, which are either undifferentiated (embryonal carcinoma) or differentiated (exhibiting a degree of embryonic (teratoma) or extra-embryonic (yolk sac choriocarcinoma) patterning) [2]. Most common risk factors for testicular cancers include ages of 20 to 34, cryptorchidism, family history of testicular cancer, cancer of contralateral testis, infertility, Klinefilter syndrome, Intratubular germ cell neoplasia (IGCNU) and maternal estrogen exposure. Additional less common factors which are still being evaluated as possible causes include tallness, marijuana use, vasectomy, trauma, mumps and human immunodeficiency (HIV) [2, 3]. Also, per literature review we found that men who have two copies of the common version of the c-KIT ligand (KITLG) gene have a 4.5-fold higher risk of testicular cancer than men who do not. [4] Choriocarcinoma is a non-seminomatous germ cell (NSGCT) tumor accounting for less than 1% to 3% of all the testicular neoplasms. It typically originates from chorionic epithelium of the placenta in females as seen in hydatidiform mole. On rare occasions it arises from germ cells in testis or ovary [1]. It is the malignant growth of trophoblastic cells, which is characterized by secretion of HCG. Choriocarcinoma of the testis has a particularly high-risk histology and the patients with this tumor are more likely to present with symptoms from metastases rather than a testicular mass. [5].Less than 8% of the testicular germ cell tumors contain a choriocarcinoma component and pure choriocarcinoma accounts for only 0.3% of all the primary testicular germ cell tumors [5]. Choriocarcinoma can present as pure choriocarcinoma, which comprises components of syncytiotrophoblasts and cytotrophoblasts, or it can be a mixed germ cell tumor, which contains choriocarcinoma as one of the components [1]. Choriocarcinomas are aggressive tumors with the potential for early metastases to the lung, liver, gastrointestinal tract, brain, bone, retroperitoneal lymph nodes. Pure choriocarcinoma has the worst prognosis of all germ cell tumors [1, 6]. The most common presenting symptoms include hemoptysis, difficulty breathing secondary to pulmonary metastases, back pain secondary to retroperitoneal spread, gastrointestinal bleeding due to gastrointestinal tract metastases and neurological symptoms that are due to brain metastases [5]. Tumoral specific markers are an important diagnostic criteria in patients with choriocarcinoma. Beta-human chorionic gonadotropin serum concentrations are increased in all patients with pure choriocarcinoma and alpha-fetoprotein concentrations may be elevated in 30-60% of choriocarcinomas, usually in mixed histological forms with other germ-cell tumors [7].Ocular metastasis account about 10% of systemic malignancies [8]. Cancer metastases that appear in and around the eye are usually from a breast cancer in women and lung cancer in men. Other less common sites of origin include the prostate, the kidney, the thyroid, and gastrointestinal tract. Hematological cancers like lymphoma and leukemia can also metastasize to the eye and orbit. [9] Unlike other metastatic ocular disease, significant hemorrhage is associated with metastases from choriocarcinoma in more than 85% of cases and should raise suspicion for this type of primary malignancy. [8]Of all the structures in eye, the posterior choroid is frequently involved as it is rich in vasculature [9]. Per our literature review, few cases of choroidal metastasis from choriocarcinoma have been reported so far, but no case of pure choriocarcinoma with metastasis to sclera has been reported. Metastatic choriocarcinoma is one such malignant disease with high remission rate and 5 year survival rate of 70-80%. Important prognostic factors include chemorefractory status, beta human gonadotropin concentrations higher than 1000 mIU/ml and primary mediastinal tumor. [10]Prognosis of testicular tumors was poor until the introduction of cisplatin based chemotherapy in mid 1970’s [8]. The advent of cisplatin-based chemotherapy for the treatment of advanced germ cell tumor, led the need to stratify patients into good and poor-risk groups. Inspite of many classifications being proposed for stratification, choriocarcinoma likely belongs to poor-risk group than the good- or intermediate-risk groups, given the highest metastatic potential [10]. Since this is a rare type of malignancy, there is lack of definite guidelines regarding the treatment options and henceforth, there is a need for further studies in this area. While other NSGCTs are highly sensitive to cisplatin-based chemotherapy, with cure rates of approximately 80% for advanced disease and nearly 100% for early stage disease. However, pure choriocarcinoma is not as sensitive to chemotherapy as mixed NSGCT. Standard chemotherapy for good-to-poor–risk NSGCT - Bleomycin, etoposide, cisplatin (BEP) for 4 cycle and additional agents include vinblastine, ifosfamide [11, 12]. Although chemotherapy may result in disappearance of the testicular mass, orchiectomy is always indicated for accurate diagnosis. There are few case reports reported in literature, where patients with pure choriocarcinoma with metastasis were treated with radiation therapy.[8] Our patient described above was managed with radical orchiectomy followed by radiation to orbit and brain initially and eventually had chemotherapy with significant improvement in his visual acuity.
4. Conclusions
- Choriocarcinoma should be considered as one of the differentials in otherwise healthy young males who present with visual abnormalities and constitutional symptoms. We propose that one should manage patients with pure choriocarcinoma with scleral metastasis aggressively with radiation therapy and chemotherapy, with toxicity a secondary concern as there is only 35 to 50% cure with chemotherapy [10]. Finally, we conclude that it would be prudent to consider genetic study as a future project for better understanding of this rare tumor.
ACKNOWLEDGEMENTS
- We would like to acknowledge Gabriela Oprea, MD; Micheal Flood, MD; and Joshua Oliver, MD for their valuable contributions.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML