Neha Khambete1, Rahul Kumar2
1DentoScan.3D CBCT, Shop No.6, Queensgate CHS, Hiranandani Estate, Thane (W), India
2Department of Conservative Dentistry & Endodontics. MGM Dental College & Hospital, Navi Mumbai
Correspondence to: Neha Khambete, DentoScan.3D CBCT, Shop No.6, Queensgate CHS, Hiranandani Estate, Thane (W), India.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Abstract
Cone-beam computed tomography (CBCT) is being increasingly used for head, neck and dentomaxillofacial imaging. There is growing interest in CBCT from all fields of dentistry because it has created a revolution in maxillofacial imaging. It has caused transition of dental imaging from 2D to 3D images and has expanded the role of imaging from just diagnosis to image guidance of operative and surgical procedures. The present article is to provide an overview of this CBCT technology and review its capabilities with specific applications in clinical dental practice.
Keywords:
CBCT, Dental, Cone Beam Computed Tomography, Dental Implants
Cite this paper: Neha Khambete, Rahul Kumar, Cone Beam Computed Tomography: A Third Eye for Dental Practitioners, International Journal of Stomatological Research, Vol. 4 No. 1, 2015, pp. 1-7. doi: 10.5923/j.ijsr.20150401.01.
1. Introduction
Conventional two-dimensional (2D) imaging modalities have been used in dentistry since the first intraoral radiograph was obtained in 1896. Since then, dental imaging techniques have advanced strength by strength with the introduction of tomography and panoramic imaging. More recent advances in digital diagnostic imaging have resulted in lower radiation doses and faster processing times without hampering the diagnostic quality of the intraoral or panoramic images. However, 2D images possess inherent limitations which include magnification, distortion, and superimposition that can make it possible to misinterpret structures. [1] Cone beam CT (CBCT) was first developed for use in angiography. In 1998, Mozzo et al reported the first CBCT unit developed specifically for dental use, the NewTom 9000 (Quantitative Radiology, Verona, Italy). [2] CBCT is well suited for imaging the craniofacial area. It provides clear images of highly contrasted structures and is extremely useful for evaluating hard tissues of maxillofacial region. CBCT allows the creation in “real time” of images not only in the axial plane but also 2-dimensional (2D) images in the coronal, sagittal and even oblique or curved image planes - a process referred to as multiplanar reformation (MPR). In addition, CBCT data are amenable to reformation in a volume, rather than a slice, providing 3-dimensional (3D) information. [2, 3]
2. Principle of Action
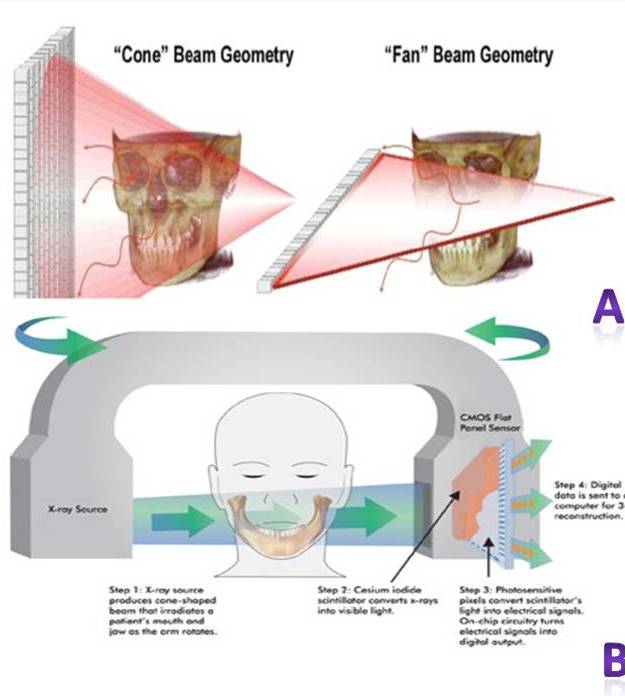
The principle of CBCT is based on a fixed x-ray source and detector with a rotating gantry. The x-ray source emits a cone-shaped beam of ionizing radiation that passes through the centre of the scan region of interest (ROI) in the patient’s head to the x-ray detector on the other side. The gantry bearing the x-ray source and detector rotates around the patient’s head in 360 degree arcs. (Figure 1A & B) 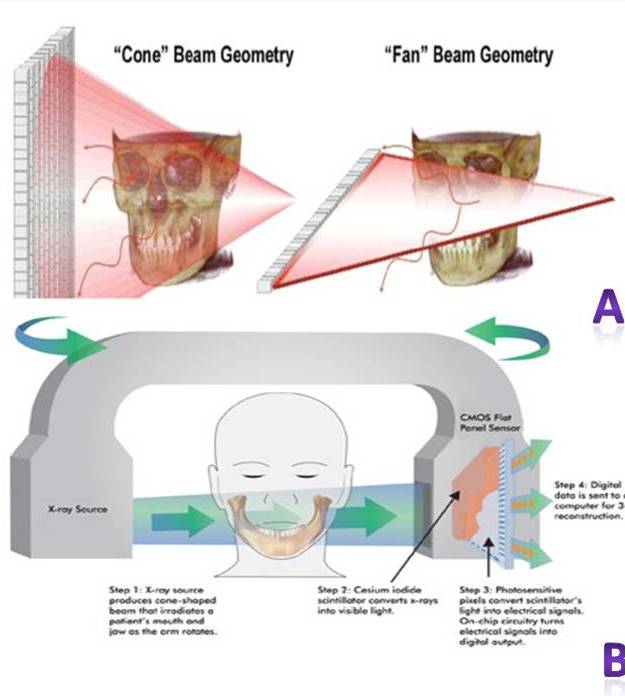 | Figure 1. A: Difference between Cone –Beam and Fan-Beam Geometry B: Procedure of Image acquisition in CBCT |
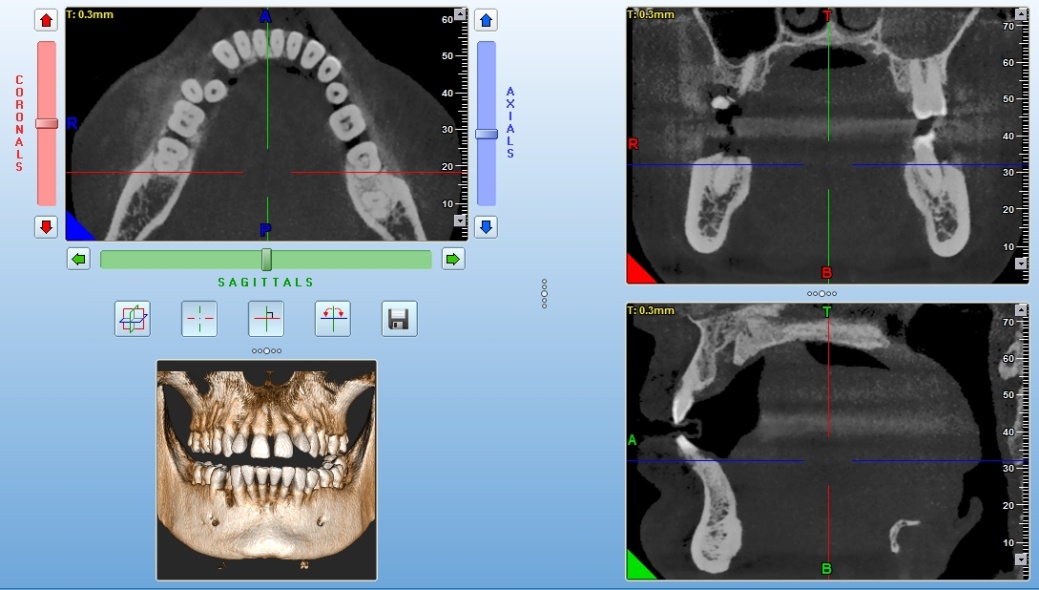
While rotating, the x-ray source emits radiation in a continuous or pulsed mode allowing projection radiographs or “basis images”. [2] These are similar to lateral cephalometric radiographic images, each slightly offset from one another. This series of basis projection images is referred to as the projection data. Software programs incorporating sophisticated algorithms including back-filtered projection are applied to these image data to generate a 3D volumetric data set, which can be used to provide primary reconstruction images in 3 orthogonal planes (axial, sagittal and coronal). [4] (Figure 2)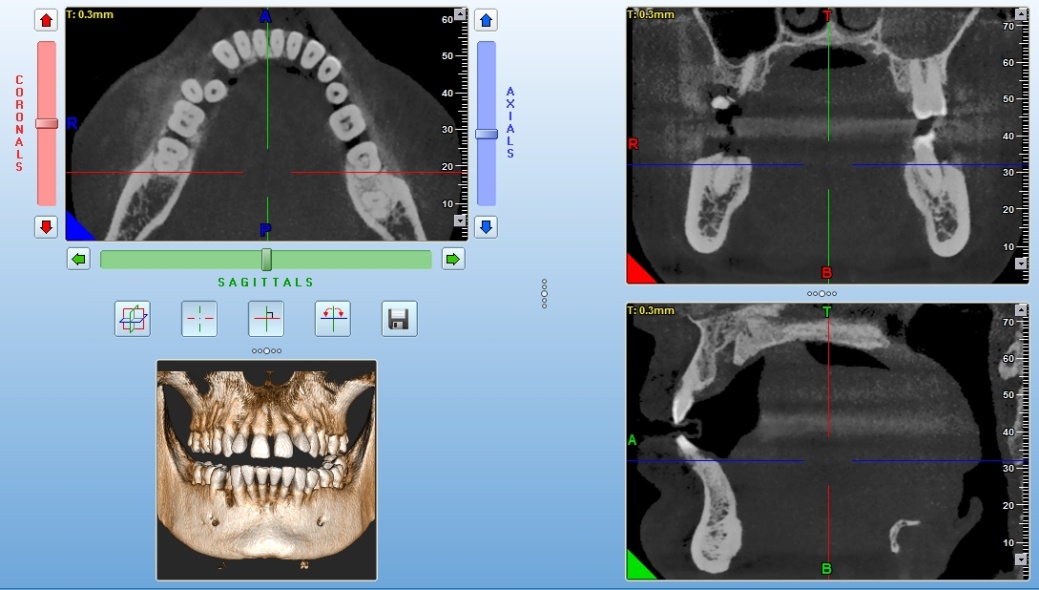 | Figure 2. A multiplanar display panel of CBCT showing axial, coronal, sagittal and 3D –reconstructed images |
3. Applications in Dentistry
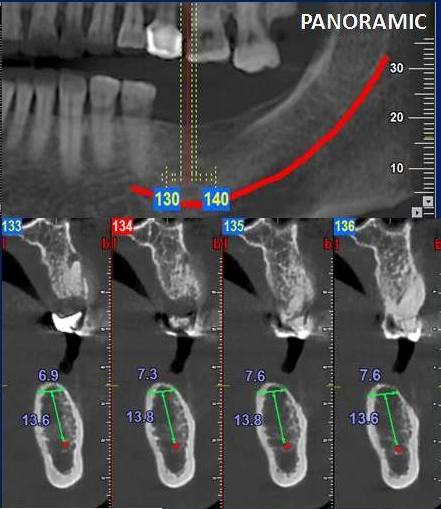
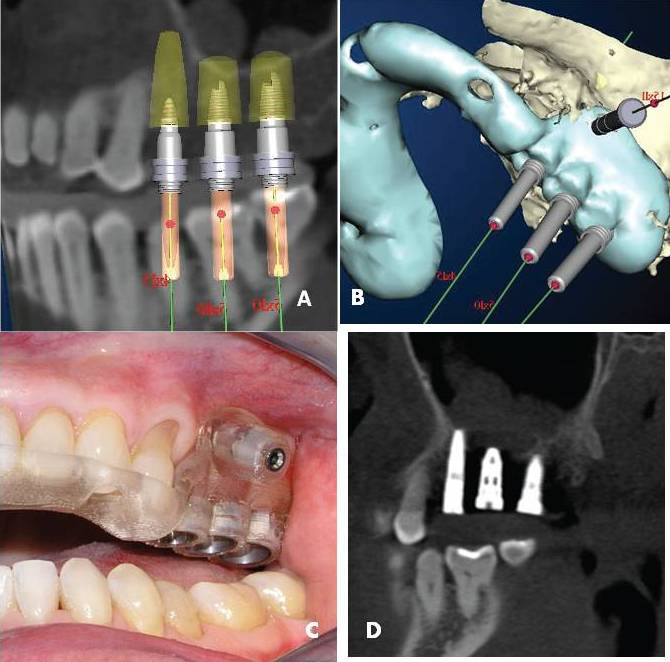
1. Implantology: The increasing need for dental implants to replace missing teeth requires a technique capable of obtaining highly accurate alveolar and implant site measurements to assist with treatment planning and avoid damage to adjacent vital structures during surgery. [5] Cross-sectional imaging techniques can be an invaluable tool during preoperative planning for dental implant procedures. [6] 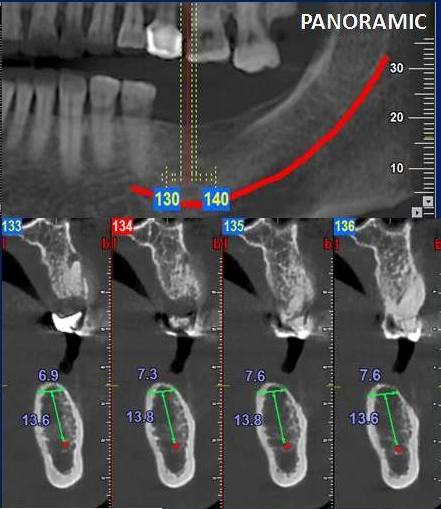 | Figure 3. Implant planning using cross-sectional imaging. |
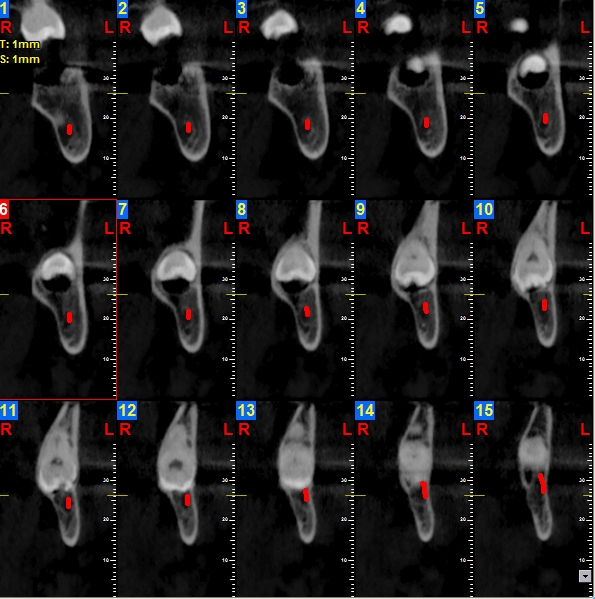
CBCT has reduced implant failures by providing information about bone density, the shape of the alveolus, and the height and width of the proposed implant site for each patient. [7] CBCT is commonly utilized in postsurgical evaluations to assess bone grafts and the implant’s position in the alveolus. [8, 9]2. Oral Surgery: a) Maxillofacial Trauma: Imaging of complex high-contrast bony structural pathology such as craniofacial fractures is a logical application for CBCT. The low-dose high-resolution properties of CBCT imaging are used in preoperative characterization of mandibular and orbital floor fractures. The intra-operative use has demonstrated the feasibility of CBCT use in surgical navigation, localization of bony fragments, and evaluation of screw anchorage and plate fittings with low levels of metal artifacts as compared to CT. [10]b) Oral & Maxillofacial Pathologies: Three dimensional imaging of cysts and tumors of the maxillofacial region can give the surgeon the vital information necessary for planning surgery; with volumetric analysis, this can help anticipate the need for and volume of a potential graft for reconstruction. [11]c) Craniofacial Surgery: Treatment planning for patients with cleft lip and palate entails many unique considerations. Due to the young age of the patients and concerns about radiation exposure, conventional CT is not always used. CBCT should allow better evaluation of dental age, arch segment positioning, and cleft size compared. Volumetric analysis promises to offer better prediction in terms of the morphology of the defect, as well as the volume of graft material necessary for repair. [11]d) Impacted Teeth: The identification, treatment planning, and evaluation of potential complications of impacted teeth are greatly improved by adding the third dimension through CBCT. The site evaluation becomes not only less invasive and less time-consuming, but also more complete. The relationship of impacted third molars to the mandibular canal, adjacent teeth, sinus walls, and cortical borders is important diagnostic information that can directly impact the outcome of surgery. [11]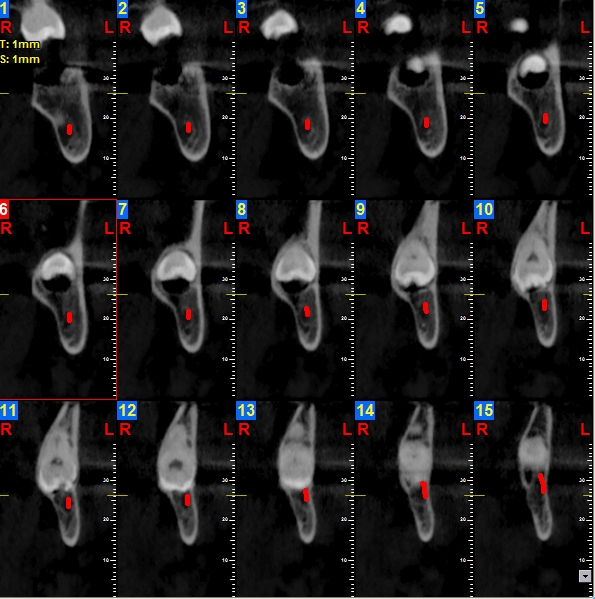 | Figure 4A. Assessing the position of impacted third molar and its relationship with inferior alveolar canal |
 | Figure 4B. MIP 3D reconstruction showing impacted 38 |
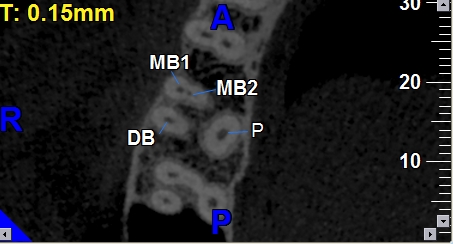
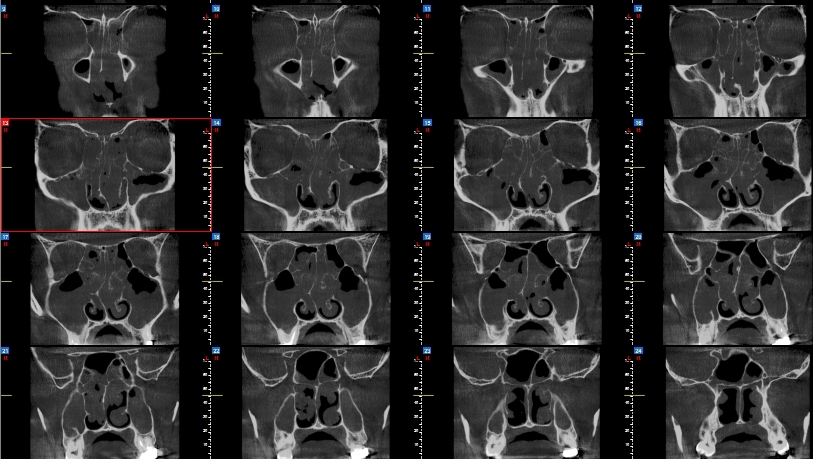
3. Endodontics: Endodontic applications of CBCT include the diagnosis of periapical lesions due to pulpal inflammation, visualization of root canals, elucidation of internal and external resorption, visualization of extra roots and detection of root fractures. CBCT has been explored for applications in endodontics, including periradicular surgical planning, assessment of periapical pathology, and dentoalveolar trauma evaluation. There may also eventually be a role for CBCT in early detection of periapical disease, which could lead to better endodontic treatment outcomes. Promising results have been demonstrated in studies characterizing CBCT images for endodontic surgical planning purposes as well. [12, 13]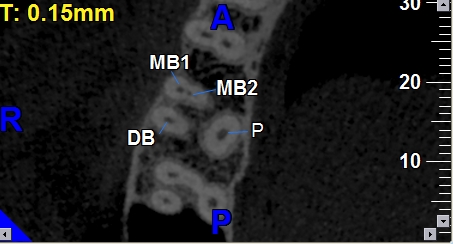 | Figure 5. CBCT of Maxillary first molar showing presence of MB2 Canal |
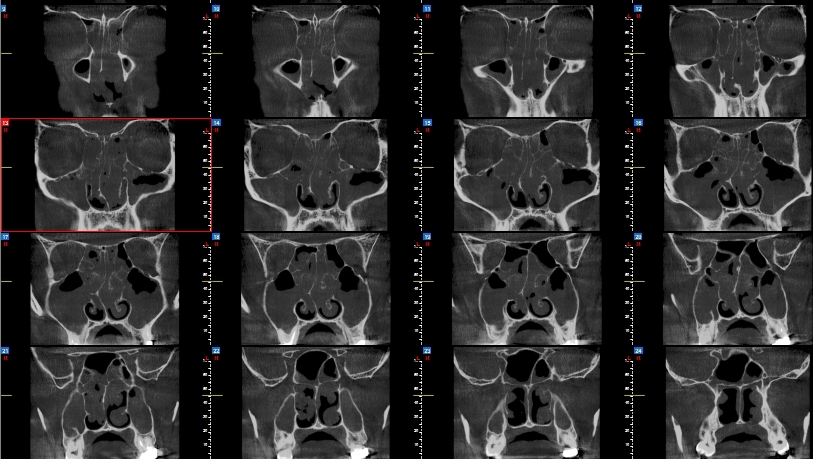
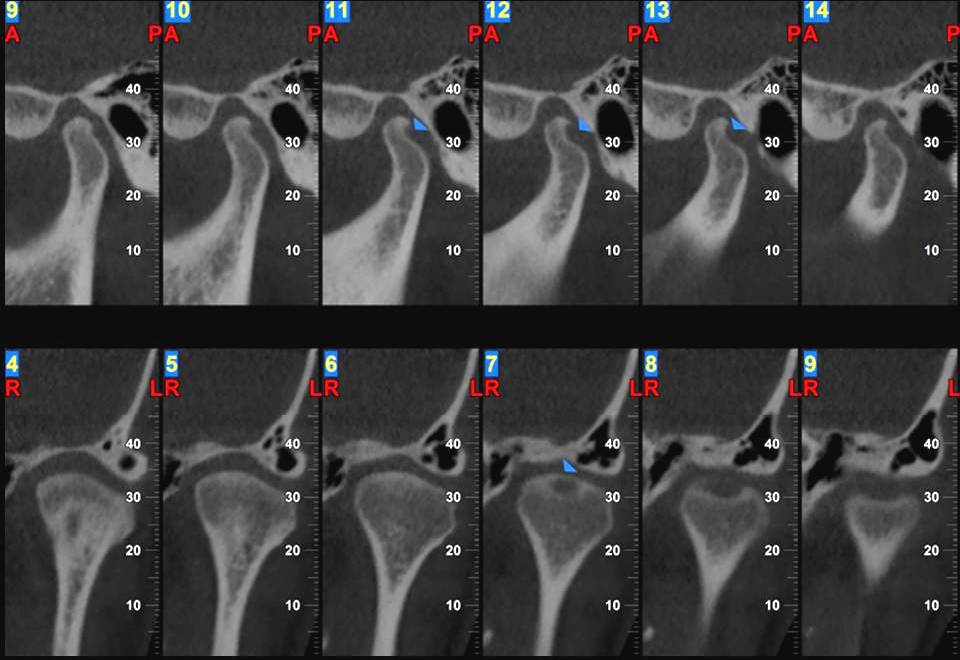
4. Periodontics: Limitations of 2D radiography could cause dentists to underestimate the amount of bone loss or available bone due to projection errors and has led to errors in identifying reliable anatomical reference points. CBCT provides accurate measurement of intrabony defects and allows clincians to assess dehiscence, fenestration defects, and periodontal cysts. CBCT can visualize buccal and lingual defects. CBCT can also be used to assess furcation involvement of periodontal defects and allow clinicians to evaluate postsurgical results of regenerative periodontal therapy. Studies are being conducted on use of Digital Subtraction Radiography along with CBCT images to assess the post-operative treatment outcomes [12]5. Orthodontics: The introduction of new software in orthodontic assessment, such as Dolphin (Dolphin Imaging & Management Solutions) and In Vivo Dental (Anatomage), have allowed dentists to use CBCT images for cephalometric analysis, making it the tool of choice for assessing facial growth, age, airway function, and disturbances in tooth eruption. CBCT is a reliable tool for assessing the proximity of impacted teeth to vital structures that could interfere with its orthodontic movement. CBCT can also be used for pre-and post- operative evaluations in orthognathic surgeries. When mini-implants are required as temporary anchors, CBCT offers visual guides for safe insertion, thus avoiding accidental and irreparable damage to the existing roots. [14]6. Temperomandibular Joint Disorders: Diagnostic imaging of the TMJ is crucial for proper diagnosis of diseases and dysfunctions associated with joint conditions. CBCT’s accuracy and lack of superimposition makes it possible to measure the roof of the glenoid fossa and visualize the location of the soft tissue around the TMJ, which can offer a workable diagnosis. These advantages outlined above have made CBCT the best imaging device for cases involving trauma, fibro-osseous ankylosis, pain, dysfunction, and condylar cortical erosion and cysts. [15]7. Airway assessment: 3D imaging is a very efficient method to inspect and identify diffuse narrowing (narrowing disturbed over a large distance) or focal narrowing (encroachments) of the airway. Imaging can identify patients with airways who are at risk for obstruction and other anatomic characteristics that may contribute to Obstructive sleep apnea. The airway extending from the tip of the nose to the superior end of the trachea can be visualized on cone beam CT (CBCT) scans. Because these scans also include the jaws, teeth, cranial base, spine, and facial soft tissues, there is an opportunity to evaluate the functional and developmental relationships between these structures. [16]8. Paranasal sinus evaluation: Preliminary evidence suggests that CBCT may be suited for specific imaging tasks in the context of intra-operative and perioperative bony structural evaluations, enabling low-dose assessment of individualized paranasal sinus anatomy, surgical outcomes, and stent placements. [17]9. Ear examinations: CBCT might be useful for certain imaging tasks in temporal bone imaging, including evaluation of inner and middle ear implant positioning, as well as definition of high-contrast postsurgical change and structural anatomy within the lateral skull base. Possible applications in evaluation of bony pathologies such as ossicular chain erosions, is also emerging. Currently, further research is required to characterize the ability of CBCT to define temporal bone structures and bony pathology reliably. [17]10. Forensic Dentistry: Age estimation is an important aspect of forensic dentistry. It is imperative that clinicians are able to estimate the age of the individuals placed in the legal system (and those who are deceased) as accurately as possible. Typically, extraction and sectioning are required to quantify these morphological changes, which is not always a viable option. CBCT, however, provides a non-invasive alternative. [18]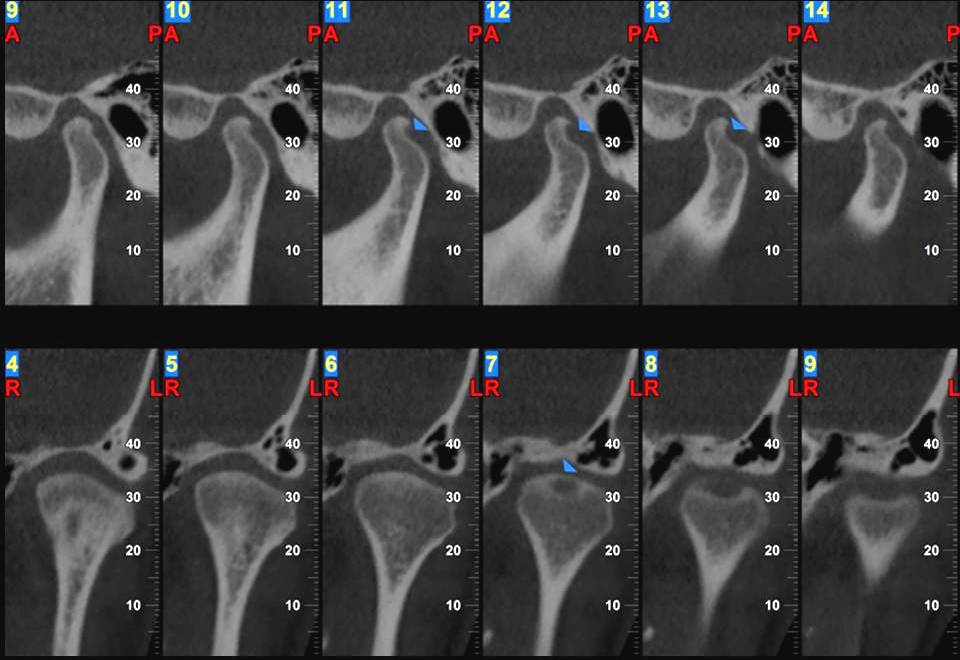 | Figure 6. Oblique Sagittal & coronal sections TMJ showing developmental anamoly (Note the lack of superimposition gives superior visualization of articular surfaces) |
 | Figure 7. Coronal Sections showing radiopacity in the right and left maxillary sinus probably suggestive of maxillary sinusitis |
4. Discussion
CBCT is well suited for imaging the craniofacial area. It provides clear images of highly contrasted structures and is extremely useful for evaluating bone. Although limitations currently exist in the use of this technology for soft-tissue imaging, efforts are being directed toward the development of techniques and software algorithms to improve signal-to-noise ratio and increase contrast. The use of CBCT technology in clinical practice provides a number of potential advantages for maxillofacial imaging compared with conventional CT.: 1) X-ray beam limitation providing multiple Fields of vision (FOV), 2) Isotropic voxels with sub-milimeter resolution providing more accurate images, 3) Rapid scan time, 4) Reduced radiation doses, 5) Unique display modes for maxillofacial imaging and 6) reduced image artefacts.With the continued decreasing cost of CBCT technology, it is only a matter of time until CBCT finds its way into the average oral and maxillofacial radiology practice. The increased diagnostic capability combined with the lower radiation dose also will help bring this technology into the mainstream. The applications described herein are merely the beginning. We are now capable of obtaining significantly more data to characterize a patient’s condition. The next step is to establish how best to use these additional data in the most effective manner. [2]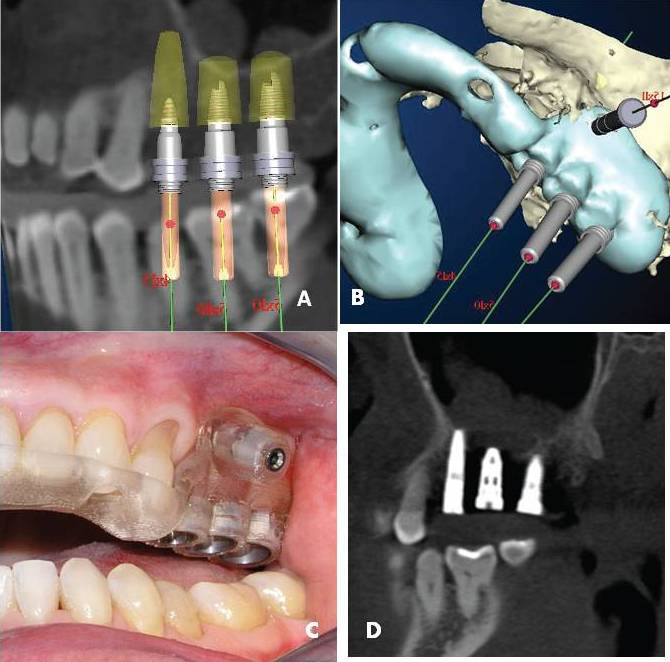 | Figure 8. CBCT Guided implant surgery, A: Diagnostic work up B: CAD-CAM Fabrication of surgical guide C: Fabricated guide D: Post Operative CBCT |
FUTURE APPLICATIONS: The accuracy of CBCT data can be used to fabricate surgical guides using CAD-CAM systems. A surgical guide can be designed and constructed on the basis of computer analysis of the available bone, the proximity of teeth to the proposed implant site and structures to be avoided in implant placement. This information can help clinicians comprehend better the optimal location of implant placement and ultimately lead to better potential for a successful outcome. [9] Autotransplantation of teeth is a viable option for tooth replacement in carefully selected patients. The CBCT based preoperative planning and use of stereolithographic tooth replica and surgical guide allowed reduced surgical time, with a decrease in extra-alveolar time and less manipulation of the donor tooth, which may reduce the periodontal ligament injury during the trial and error of the donor tooth. [19]
5. Conclusions
CBCT is here to stay and play an integral role in diagnosis and treatment planning for many dental disciplines. Additionally, at this point, we conclude that if used judicially, its benefits would outweigh the inherent risks. We should advocate more professional education and training on this emerging technology. Meanwhile, nothing should keep clinicians from continuing sound practices with appropriate aid of this extraordinary imaging technology.
References
| [1] | Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am 2008;52(4):707-730. |
| [2] | Scarfe WC, Farman AG, Sukovik P. Clinical Applications of Cone-Beam Computed Tomography in Dental Practice. J Can Dent Assoc 2006; 72(1):75–80. |
| [3] | Ziegler CM, Woertche R, Brief J, Hassfeld S. Clinical indications for digital volume tomography in oral and maxillofacial surgery. Dentomaxillofac Radiol 2002; 31(2):126–30. |
| [4] | Kawamata A, Ariji Y, Langlias R Three dimensional computed tomography in dentistry Dent Clin North Am 2000,44:2:395-410. |
| [5] | Macleod I, Heath N. Cone-beam computed tomography (CBCT) in dental practice. Dent Update 2008;35(9):590-598. |
| [6] | Tyndall DA, Brooks SL. Selection criteria for dental implant site imaging: a position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:630–37. |
| [7] | Howerton WB Jr, Mora MA. Advancements in digital imaging: What is new and on the horizon? J Am Dent Assoc 2008;139 Suppl:20S-24S. |
| [8] | Tischler M. In-office cone beam computerized tomography: Technology review and clinical examples. Dent Today 2008;27(6):102-106. |
| [9] | Worthington P, Rubenstein J, Hatcher D. The role of cone-beam computed tomography in the planning and placement of implants. JADA 2010;141(10 suppl):19S-24S. |
| [10] | Pohlenz P, Blessmann M, Blake F, et al. Clinical indications and perspectives for intraoperative cone-beam computed tomography in oral and maxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:412–17. Epub 2006 Sep 26. |
| [11] | Quereshy FA, Savell TA, Palomo JM Applications of Cone Beam Computed Tomography in the Practice of Oral and Maxillofacial Surgery J Oral Maxillofac Surg,2008;66:791-6. |
| [12] | Tyndall DA, Rathore S. Cone-beam CT diagnostic applications: Caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am 2008;52(4): 825-841. |
| [13] | Patel S, Dawood A, Ford TP, et al. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J 2007;40:818–30. Epub 2007 Aug 14. |
| [14] | Farman AG, Scarfe WC. Development of imaging selection criteria and procedures should precede cephalometric assessment with cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2006;130(2):257-265. |
| [15] | Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol 2004;33(3): 196-201. |
| [16] | Hatcher D,Cone Beam Computed Tomography: Craniofacial and Airway Analysis. Sleep Med Clin 5 (2010) 59–70. |
| [17] | Miracle AC, Mukherjee SK Conebeam CT of the Head and Neck, Part 2: Clinical Applications Am J Neuroradiol, 2009; 30:1285–92. |
| [18] | Yang F, Jacobs R, Willems G. Dental age estimation through volume matching of teeth imaged by cone-beam CT. Forensic Sci Int 2006;159Suppl 1:S78-S83. |
| [19] | Shahbazian M, Jacobs R, Wyatt J, Denys D, Lambrichts I, Vinckier F et al Validation of the cone beam computed tomographyebased stereolithographic surgical guide aiding autotransplantation of teeth: clinical case-control study Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:667-675. |

 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML