-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Stomatological Research
2012; 1(3): 31-34
doi: 10.5923/j.ijsr.20120103.03
Clinical Evaluation of Periodontal Parameters in Correct Marginal Dental Restorations
Seyyed Ali Banihashemrad 1, Mohammad Javad Mogaddas 2, Majid Reza Mokhtari 2, Fateme Farazi 3, Assadollah Garajian 1, Reza Mehrara 1
1Dept of Periodontology,School of Dentistry,Mashhad University of Medical Sciences,Mashhad, 91889, Iran
2Dept of Operative Dentistry,School of Dentistry,Mashhad University of Medical Sciences,Mashhad, 91889, Iran
3Dept of Oral Medicine,School of Dentistry,Bojnourd University of Medical Sciences,Bojnourd, 49815, Iran
Correspondence to: Majid Reza Mokhtari , Dept of Operative Dentistry,School of Dentistry,Mashhad University of Medical Sciences,Mashhad, 91889, Iran.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Marginal restorations are appropriate places for plaque accumulation and bacteria reproduction causing periodontal disease . The present study was conducted to compare the periodontal status in patients with correct marginal restorations and their controls referred to department of Oral Medicine and Operative Dentistry of Mashhad Dental School in 2009. Fifty patients with one or more marginal restorations as well as their controls were studied in a cross-sectional method. Gingival bleeding and plaque indices were evaluated in both groups for the purpose. Periodontal probes were used for measuring plaque, bleeding index and probing depth and gingival index was examined by observation. 50 percent of cases had plaque index of 0 as the rate was 60 percent in control samples. Considering gingival index, the percentage of patients with 0 gingival index was 58 and 74 in case and control groups respectively. Bleeding index of 0 was reported to be 38 and 72 per cent in case and control groups. Probing depth in case group was more than control. Statistical analysis showed significant difference between the two groups considering four measured ariables (P < 0.05). According to the results of this study, even the correct marginal restoration may have effect on periodontal status.
Keywords: Correct Restorations, Plaque Index, Bleeding Index, Gingival Index
Cite this paper: Seyyed Ali Banihashemrad , Mohammad Javad Mogaddas , Majid Reza Mokhtari , Fateme Farazi , Assadollah Garajian , Reza Mehrara , "Clinical Evaluation of Periodontal Parameters in Correct Marginal Dental Restorations", International Journal of Stomatological Research, Vol. 1 No. 3, 2012, pp. 31-34. doi: 10.5923/j.ijsr.20120103.03.
1. Introduction
- Different studies showed that restoration edges have always been suitable places for plaque accumulation and bacteria reproduction resulting gingivitis and even tooth loss in some cases. Restorative materials and cements can affect periodentium tissues in different ways and result in gingivitis and gingival damage.These impressions mostly occur in restorations with sub -gingival margins and can be due to physical or chemical compositions of the materials. In most cases these destructive responds are due to superficial roughness formed by dental materials than to their composition(1,2).In this case a rougher surface results in gingivitis by accumulating more plaque. The most significant mechanism through which dental materials can affect marginal gingival health is through increase in plaque accumulation.Typically sub-gingival margins have a 20-40µ gap between restoration margin and unprepared tooth which after some time and being washed , the gap's cement is colonized with bacterial plaque and destructive effects of the plaque are exerted (3).Restorative materials are not damaging to periodontal tissues, in themselves (4,5).Of course self-cure acrylics can be an exception in this regard. The studies have also showed that although the different dental materials surface texture differ in plaque retention capacity (6), all can be sufficiently cleaned if polished and have access to dental care.(8,9)However as it was said before, dental materials can physically or chemically damage oral mucosa. It is believed that materials released from restorative materials can directly or indirectly help aggregate existing gingivitis and have a synergic effect with plaque in intensifying inflammatory reactions.Moreover the responses to increase in immunitysensitivity to materials usually delays the healing process ,which if continued, and reaches bone's crest , will lead to periodontitis.This study was made with the aim of comparingperiodontal condition of correct gingival-adjacent restorations with control group in patients referring to restoration ward of Mashhad School of Dentistry in 2009.
2. Materials and Methods
- This clinical study was conducted in 50 patients referred to department of Oral Medicine and Operative Dentistry of Mashhad Dental School in 2009 as well as their controls in a cross-sectional method .The patients had the required correct restoration (The patient had to have correct gingival-adjacent restorations, no systemic disease and at least one year passed from the restoration.)lacking the conditions for exit(No correct gingival-adjacent restorations, overhang, unsuitable contour ,lack of restoration margin fit, having a systemic disease ,taking antibiotics within the past three months , be under gingival and periodontal treatments). Sampling is made in easy access using observation methods and clinical examination by explorer to check correct and fit margin and restoration surface roughness. Periodontal probe was used to determine rate of restoration-adjacent sulcus bleeding .Two teeth of the patient were studied in this research ,one the restored tooth as the case and a healthy one as the control.GI (Gingival Index) ، (Plaque Index)PI ، (Bleeding points Index)BPIوPPD (Probing Pocket Depth) in four surfaces of buccal, lingual, mesial and distal . Based on the index intensity , a low, average and high rank is assigned to it. In gingival index , the change in color ,inflammation and consistency and in plaque index: Rate of plaque accumulation, and bleeding index: Rate of bleeding, will determine the index's rank. The depth of probing is measured and recorded by dial explorer. The normality of data distribution weas studied using K-S test in SPSS software and showed no normal distribution except in data related to probing depth in restored teeth. Therefore Wilcoxon test was used in data analysis.
3. Results
- The Gingival Index(GI)average in restored tooth is at least twice of the tooth without restoration. This is a statistically significant difference.(P=0.002)The maximum of GI in restored tooth is 1 and 0.75 in non-restored tooth. The SD compared to the mean in non-restored tooth is higher than restored tooth .
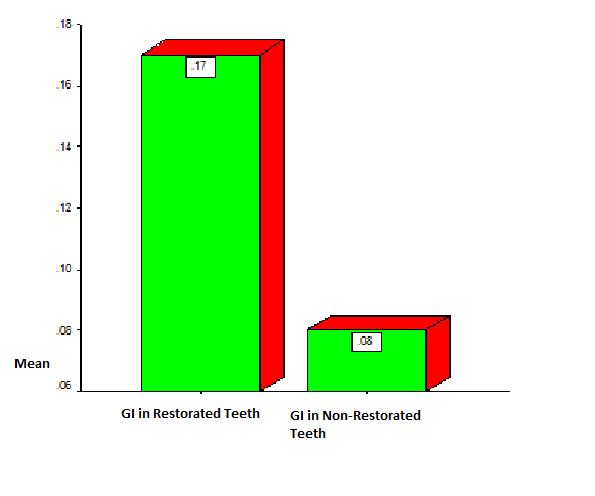 | Diagram 1. GI Index in Restored Teeth and Teeth without Restoration |
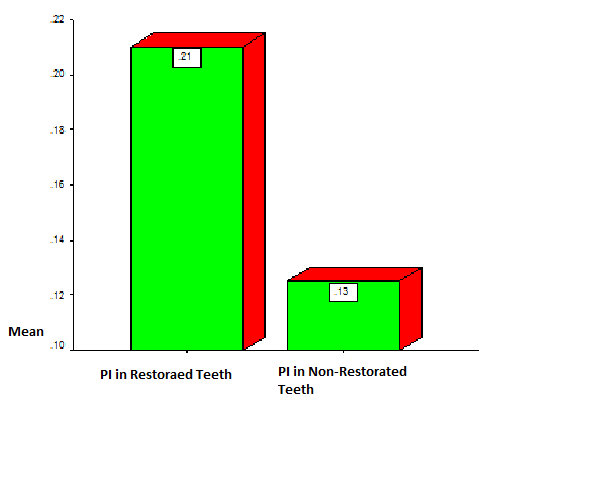 | Diagram 2. PI index in restored teeth and teeth without restoration |
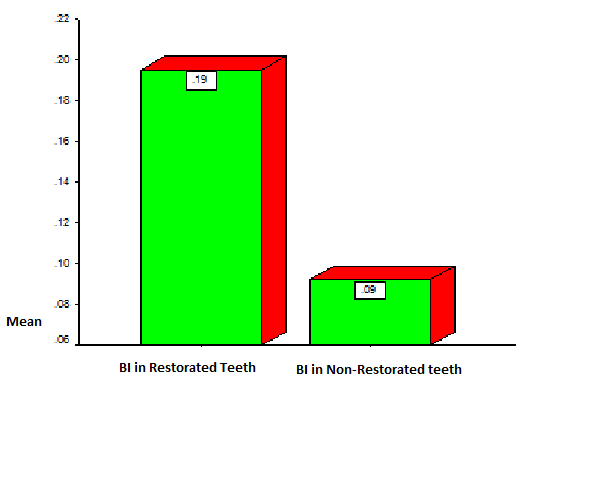 | Diagram 3. BOP Index in restored and non-restored teeth |
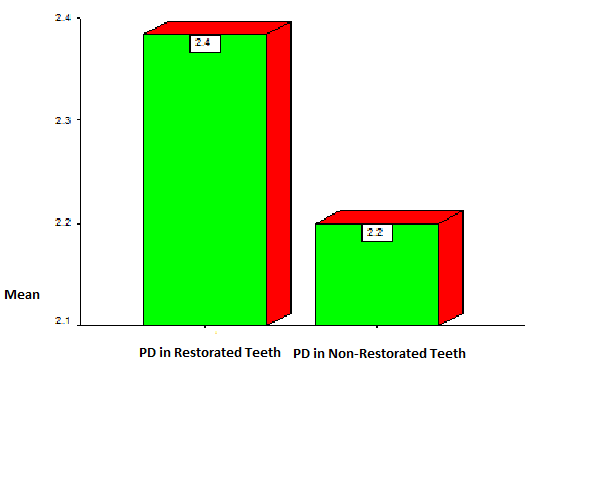 | Diagram 4. PD Index in Restored and Non-restored Teeth |
4. Discussion
- In a general comparison it can be seen that whether in restored tooth or in control tooth the most percentage of abundance except in PD was related to zero except in BOP index in restored teeth. Zero grade in control group is of greater abundance compared to restored tooth group. But in next grades restored tooth has a greater abundance compared to control group teeth .All these mean a rather bad condition of periodontal in restored tooth group compared to control group. In other words ,restored teeth surfaces show indices with a greater abundance and intensity as compared to the healthy tooth.In a research in which Dunkin et al.,(1983) studied the gingival reaction toward Class V composite resin restorations, no significant difference was seen between studied indices in the two groups.In a research made by Luthardt and Mandy Stobel in 2000 ,plaque retention in crowns and temporary bridges significantly increased which approves the present results.(10).The research made by Van Dijken,Claesson and Konradsson in 2007(11) showed that there is no difference in plaque and gingival indices and IL1α, IL1β and antagonist receptor between ceramic, composite and enamel in their adjacent gingival tissues within a 10-day experimental gingivitis and temporary study. More Gingival Cervicular Fluid was found next to composite restorations. In time-limited study it is not referred to the amount of time passed from the restoration.In the study made by Van Dijkan and Sjostrom in 1998(12)no difference was found in the rates of plaque and gingival index adjacent to restorations among different materials within an experimental 7-day gingivitis. in the seventh day less GCF (Gingival Cervicular Fluid)was sampled in enamel surfaces which is an indicator of greater gingival vulnerability adjacent to different restorations to lack of hygiene and therefore approves the results of the current study. Another study made by Kent et.al, in 2002(13) showed that (1)crowns and FPDs (Fixed Partial denture) increase the advanced gingivitis adjacent to restoration .(2)specially if they are gingival intra-sulcus edge, poor adaptation and rough surface .The result (1) conforms the current study. However in correct restorations the result number (2) does not conform the present study. This study showed that poor or incomplete restorations are related to gingivitis ,but it did not show the increase in gingival links adjacent to crowns or FPDs.Further studies in this regard can be made by measuring indices at the beginning of the study and before performing correct gingival-adjacent restorations and comparing them after restorations .In this case lots of intervening and confounding factors will be omitted. Although a number of studies have been made to compare different types of restorations, a study like the present one focusing on the effect of different dental materials in gingival tissues applied in correct gingival-adjacent restorations seems required.
5. Conclusions
- The results of the current study showed that the teeth with one or more correct restored surfaces show more GI compared to control tooth with healthy non-restored enamel. Even correct-restored teeth have a role in periodontal diseases and demand more health care .It can explain the role of decay preventive principles in preventing periodontal diseases even more.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML