-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2017; 6(1): 12-18
doi:10.5923/j.ijpt.20170601.03

Enabling Engagement in Provider-Recommended Physical Activity
Anthony U. Emekalam1, Latasha Wade2, Shirley Brown1
1Dr. Herman G. Cooke Department of Natural Sciences, Pharmacy and Health Professions, the Elizabeth City State University, USA
2Department of Pharmacy Practice and Administration, School of Pharmacy and Health Professions University of Maryland Eastern Shore, Princess Anne, USA
Correspondence to: Anthony U. Emekalam, Dr. Herman G. Cooke Department of Natural Sciences, Pharmacy and Health Professions, the Elizabeth City State University, USA.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: Successfulengagement in regular physical activity usually requires motivation. This study investigated impacts of a provider-facilitator motivational support partnership on adherence to provider-recommended physical activity. Methods: 75 study participants from 5 doctor’s offices in Elizabeth City and a neighboring town both in northeastern North Carolina were referred to the Elizabeth City State University Community Health Ambassadors Program (ECSUCHAP) on a rolling basis. Each participant received personal telephone-based motivational support from trained Community Health Ambassadors (students from professional pharmacy and allied health programs) for 52 weeks. Adherence to the physical activity regimen recommended by providers for each participant at the time of referral was tracked, documented and measured. Results: 100% adherence was achieved by all participants during the first 10 weeks of referral. Percentage adherence declined to 80% after 26 weeks and to 57% at the end of the mentoring cycle. Adherence was significantly more in older program participants (> 60 Y/O) (85%) in comparison to younger participants (< 60 Y/O) (33%). Conclusion: Collaborative arrangements between a facilitator of simple cost effective motivational supports and primary health care providers is effective in fostering adherence to prescriber-recommended physical activity by patients in primary care settings. Modified perceptions of importance of clinical benefits of physical activity that was achieved by written recommendations of activity regimens and referrals to a motivational support program by providers augmented response to motivational supports.
Keywords: Physical activity, Motivational support, Collaboration, Cost effective, Chronic disease prevention, Chronic disease management
Cite this paper: Anthony U. Emekalam, Latasha Wade, Shirley Brown, Enabling Engagement in Provider-Recommended Physical Activity, International Journal of Prevention and Treatment, Vol. 6 No. 1, 2017, pp. 12-18. doi: 10.5923/j.ijpt.20170601.03.
Article Outline
1. Introduction
- Regular physical activity (PA) can both prevent and delay onset (primary prevention) and progression (secondary prevention) of many preventable chronic health conditions such as coronary heart disease, stroke, arthritis and type-2 diabetes mellitus [1-4]. Research findings show that engaging in regular PA of any type (aerobic or resistance) is associated with reduced risks for many chronic health problems and contributes to improvements in overall health status of individuals that are previously inactive [3, 4]. Also, there is evidence from multiple studies of a graded reduction in risk of dying from all causes among individuals that participate routinely in various forms of physical activity [3, 5-7]. One of such studies indicated that sedentary middle-aged women (defined in the study as those engaging in less than one hour of PA per week) were 52% more likely to die from all causes, 2 times as likely from cardiovascular-related events and 29% more likely from cancer-related events when compared to women of a similar age group that were more active [8]. Furthermore, regular PA reduces relative risks of death from all causes in both men and women by 20-30% and more intensive activity has been known to reduce risks of developing breast cancer, colon cancer and stroke by approximately 20-40%, 30% and 25-30% respectively [9-11]. PA prevents stroke and cardiovascular disease by directly reducing relative risks of high blood pressures in normotensive individuals, decreasing low density lipoprotein (LDL) cholesterol and total cholesterol, increasing cardio-protective high density lipoprotein (HDL) cholesterol and reducing body weights [11, 12, 13-15, 17-19]. It has been reported that health interventions that combined various lifestyle and behavioral modifications with PA reduced incidence of type-2 diabetes by 40-60% over a period of 3-4 years in a study population of individuals with very high relative risks for type 2 diabetes such as excessive body weights [20-22]. A study demonstrated that behavioral modifications that included two and half hours of PA per week was more effective than Metformin alone in reducing incidence of type 2 diabetes among individuals at risk [23]. PA is equally effective in treatment and management of type 2 diabetes, cardiovascular disease, mental disorders and stroke. Its health benefits apply both to individuals currently suffering from these chronic conditions and to those recovering from them [24-27]. A prospective cohort study demonstrated that at least 2 hours per week of engagement in a simple aerobic PA such as walking is associated with a 39 – 54% reduction in premature death from all causes and 34 – 53% reduction in cardiovascular-related premature death among patients with diabetes [28]. In comparison, physically inactive men with type 2 diabetes are 1.7 times more likely to die of premature death than type 2 diabetics who are active [29]. Better glycemic control, avoidance of metabolic syndrome and reduction in Hemoglobin AIC to levels that significantly reduce risk of diabetes-related complications have all been documented with diabetes treatment regimens that included engagement in routine aerobic and resistance PA [30-32]. Engagement in regular PA can hinder progression while promoting reversal of the cardiovascular disease process. Several studies have confirmed the existence of an inverse relationship between routine PA and risks of premature deaths secondary to cardiovascular disease. For instance, a weekly energy expenditure of about 1600 and 2200 kcal was shown to be effective in reducing progression of coronary artery disease and plaque respectively in individuals diagnosed with heart disease [33, 34]. Also, combining regular moderately intense aerobic PA with antihypertensive pharmacotherapy lowered diastolic and systolic blood pressures significantly and reversed left ventricular hypertrophy in African American men diagnosed with severe hypertension [35]. Some research evidence suggests that PA could be beneficial in slowing down some disease processes of Alzheimer’s disorder through a mechanism that includes promotion of vascular health, lowering of blood pressure and reducing several risk factors of the disease. Up to 32% reduction in Alzheimer’s risk has been documented among individuals who participate in PA 3 times a week in comparison to individuals with less frequent participation [36, 37]. Through improvement of overall symptoms of diseases, PA has proven to have positive impacts on depression and anxiety disorders [38, 39]. Several physical and psychosocial health factors of stroke survivors including improvements in gait, cardiovascular health, and muscle strength of upper body extremities are also impacted positively by PA [40-42]. Additional benefits include improvements in executive functioning, memory, and post-stroke tiredness [43-45]. Despite these well documented health benefits of PA, physical inactivity is still a problem with serious global health implications. According to the World health organization, health conditions attributable to physical inactivity are the 4th leading cause of death globally [46]. For instance, 27% of all type 2 diabetes and 30% of Ischemic heart diseases are direct outcomes of physical inactivity [47]. The Centers for Disease Control and Prevention (CDC) reports that only 21% (1 in 5) of adult Americans are physically active at levels recommended in the 2008 PA guidelines for Americans [48, 49] and experts argue that current obesity and type 2 diabetes trends in America have direct links to physical inactivity [50, 51]. It is therefore imperative to identify effective methods for promoting PA among adult Americans if the goals of healthy people 2020 are to be met. Studies indicate that strategies that include primary care providers (PCP) are promising in enhancing adoption and maintenance of regular PA among those receiving treatments for chronic health conditions in primary care [52-55]. This study therefore investigates impacts of motivational supports collaboration for promoting PA between PCP and an engagement facilitator on adherence to prescriber-recommended PA in patients receiving care at doctors’ offices in rural northeastern North Carolina.
2. Methods
2.1. Elizabeth City State University Community Health Ambassadors Project (ECSUCHAP)
2.1.1. Description
- ECSUCHAP was a community health promotion program funded by the Blue Cross and Blue Shield Foundation of North Carolina and approved by the Elizabeth City State University (ECSU) Institutional Review Board with a primary goal of supporting engagement in PA among rural community residents in northeastern North Carolina. The program was implemented as a collaborative effort between local health care providers and allied health students of ECSU referred to as Community Health Ambassadors (CHAs). According to the collaborative understanding, participating health care providers recommended PA to patients with chronic health conditions such as diabetes and high blood pressure that are likely to be impacted favorably by it and further inquired if they are interested in receiving low intensity motivational supports to assist with engagement and participation. Providers thereafter introduced, carefully explained, obtain informed consent and referred interested patients to the program. Upon receiving referral documents (faxed exercise regimens that included patient names, addresses, contact information, PA types, intensities, durations, frequencies and copies of signed informed consents), the Principal Investigator (PI) immediately contacted patients to set up initial engagement meetings. During these meetings, the PI went over information on referral documents with patients and helped them in determining convenient PA plans in accordance to provider recommendations. For instance, if a provider recommended 30 minutes of mild intensity PA 3 times a week, the PI assisted in translating recommendation into a plan such as walking on a Treadmill on Mondays, Wednesdays and Fridays from 4 – 4.30 pm. The PI also helped with identifying and facilitating access to PA-support resources including exercise equipment. The ECSUCHAP program operated out of ECSU Health Resource Center which provided free unlimited access to exercise equipment to members of the community which helped to an extent in meeting such needs. Additionally, the program facilitated access to ECSU Wellness center to those who preferred the facility and made arrangements with organizations in the area such as Young Men Christian Association (YMCA) for discounted membership rates which was covered by the program for participants who are unable to use campus-based facilities due to distance. Once PA plans and convenient locations were determined, patients (program participants) were assigned to CHAs to provide motivational supports and track participation and engagements. Providers received monthly progress reports on each referred patient which were included in charts and used as counseling points during post referral visits.
2.1.2. Motivational Supports
- Motivational supports have 2 main components with a common goal of fostering adherence to provider-recommended physical activity (PRPA). The first component (level 1) was bipartite and was facilitated primarily by the PI. The first part focused on helping program participants establish convenient PA plans from provider recommendations and the second part was to secure unhindered access to a physical PA at ECSU Health Resource center, the ECSU Wellness Center or other locally-based organizations. The second component (level 2) was provided by CHAs whereby telephone-based (phone calls and text messages) communication methods were used to periodically remind and encourage participants to adhere to individual PA plans. Although there were no limits to number of reasonable support contacts with participants, CHAs were required to contact participants at least a day and 1 hour before every scheduled PA in their plans.
2.1.3. Community Health Ambassadors (CHAs)
- CHAs were full-time ECSU–based pharmacy students in the University of North Carolina in Chapel Hill Eshelman School of Pharmacy/ECSU Doctor of Pharmacy partnership program and students from Allied Health programs at ECSU. Announcements and solicitations for CHA positions were broadcasted through mass emails to students with details of application process and eligibility requirements included in email contents. At the close of the application window, every application was reviewed and those that met eligibility requirements (ECSU student with full time enrolment status in applicable program or discipline, sophomore or rising junior at the time of application and Cumulative Grade Point Average of at least 3.0) were invited for oral interviews. The purpose of oral interviews was to make objective assessments of students’ perceptions of motivational assistance by asking them to describe specific scenarios when they intentionally assisted someone to overcome specific health challenges or obstacles. Those that met eligibility criteria and interviewed well (described very clear scenarios) were recruited as CHAs. Recruitment continued until a predetermined number of CHA positions were fulfilled. Interviews were conducted according to the order by which applications were received. Recruited students thereafter completed a 3-hour CHA orientation and training, The Health Insurance Portability and Accountability Act (HIPAA) training, and the National Institutes of Health (NIH) Human Subject Protection Certification [56]. Each CHA was responsible for supporting up to 5 program participants a year and since supports were mainly telephone-mediated interactions, supports were not interrupted by summer or other University holidays. CHAs received financial incentives for their roles in the program.
2.2. Engaging Local Providers
- ECSUCHAP was introduced in person to healthcare providers at several doctors’ offices and clinics in Elizabeth City and surrounding towns by the PI. During these encounters the PI explained the purpose, goals and design of the program to providers in addition to providing them with written narratives of the program. The PI also answered questions, provided additional clarifications when needed and formally solicited participation of providers. Those that were interested in participating received patient referral documents and were encouraged to start referring patients to the program as soon as possible.
3. Results
3.1. Community Health Ambassadors
- 25 students out 40 applications [10 Doctor of Pharmacy students (40%) and 15 Allied health students (60%), 13 females (52%) and 12 males (48%)] were recruited to serve as CHAs from beginning of fall 2011 semester through end of spring 2012 semester.
3.2. Local Health Care providers and Program Participants
- Overall, 5 primary care providers (3 physicians, 1 Physician Assistant, and 1 Nurse Practitioner) out of 7 that were contacted expressed interest in participation. 3 (60%) of the providers were males and 2 (40%) were females. 4 (80%) were affiliated with practices in Elizabeth City and 1 (20%) with a practice that is located in a smaller more rural town about 20 miles south of Elizabeth City. Collectively they referred 75 program participants aged 31 – 70 years with a baseline average age of 52 years between April and June 2011 to the program. Providers did not receive any personal financial incentives for participation.
3.3. Adherence to Provider-recommended Physical Activity
- Adherence to PRPA for each participant was tracked and documented by CHAs for 52 weeks starting from the day that their PA plans were initially described. Average percentage adherence to PRPA started to decline progressively after initial 2 and ½ months of program participation dropping to 80% by the 25th week and 57% at the end of 52 weeks (figure 1). During the initial 2 and ½ months of program implementation, participants who missed scheduled PA were very prompt and diligent in making them up resulting in perfect adherence. However as implementation progressed over time many participants showed reluctance in making up missed activities irrespective of efforts by CHAs to steer them back on course. Additionally, adherence was significantly higher among participants 60 years and older (n=32) in comparison to those younger than 60 years (n= 43) both at 24 weeks 84.6% versus 70.4 %( p = 0.0069; Table 1) and at 52 weeks 85.1% versus 37% (P < 0.0001; Table 2)
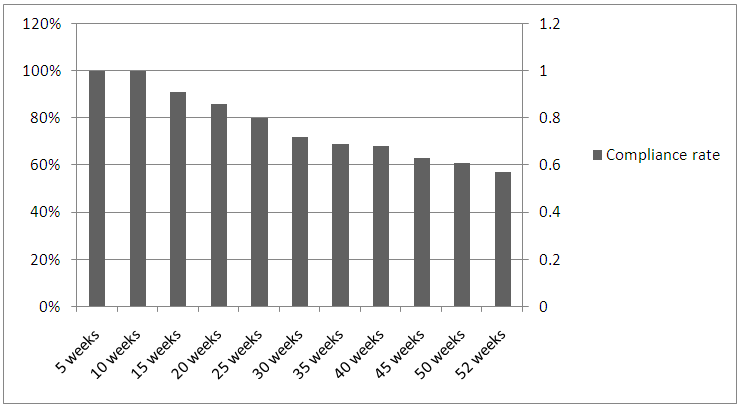 | Figure 1 |
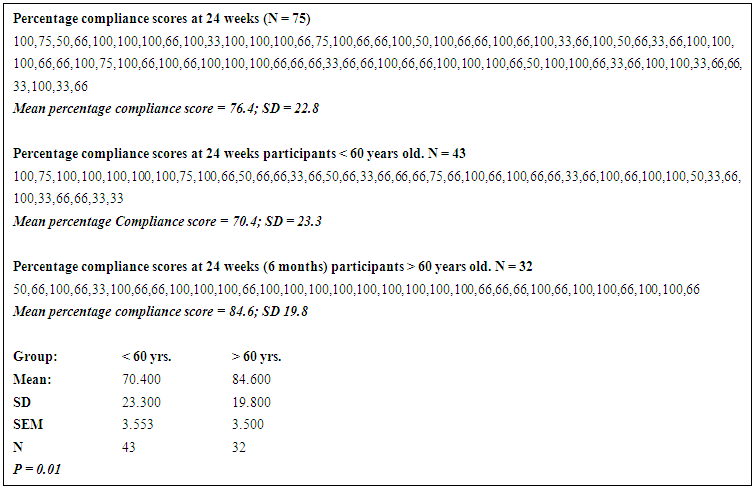 | Table 1 |
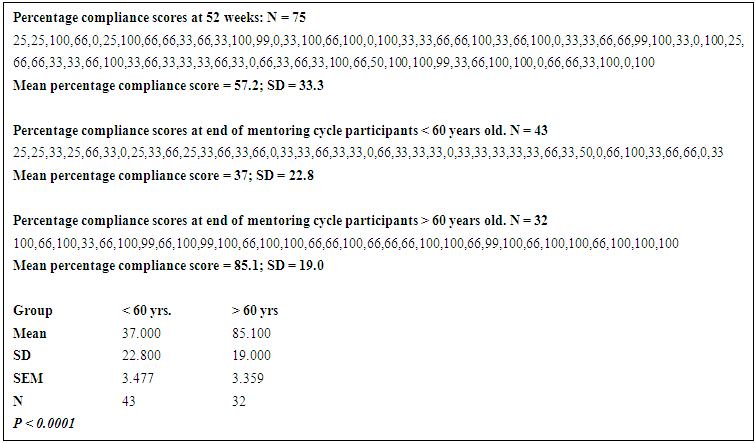 | Table 2 |
4. Discussion
- A key aim of this study was to investigate efficacy and feasibility of a strategy for promoting engagement in routine PA by using multilevel motivational supports that included collaborations with primary care providers. The main consideration for engaging providers in this process is to strengthen emphasis on clinical benefits of PA through written recommendations and referrals for motivational and engagement supports. This direct, cost-effective and simple approach (use of telephone-based communication techniques as media for extending motivational supports for PA) was effective in fostering engagement in PA among sedentary elderly individuals receiving chronic disease treatments in primary care settings. Our findings agreed with findings of Lilienthal KR et al [57] showing that telephone-based motivational support is effective in increasing short term engagements in PA among older adults as our results showed that all program participants achieved 100% adherence to provider-recommended PA during the first 10 weeks of program participation and that adherence was significantly higher among participants 60 years and older in comparison to individuals younger than 60 years (figure 1 and table 1). Furthermore, we argue that increased engagement in PA also resulted from modified (increased) perception of clinical importance of PA secondary to provider-prescribed activity regimens and subsequent referrals to formal motivational support program. This conclusion is supported by findings of Grandes et al [58] and study conclusions of Petrella et al [59] suggesting that prescribing PA in writing other than verbal counselling alone are important methods for strengthening physician counselling for PA.
5. Study Limitations
- Results and findings of this study did not include assessments of factors capable of confounding individual adherence scores. The study design did not include strategies for controlling impacts of self-motivation, family supports and other psychosocial factors that may have impacted outcomes and findings. Study results were also not modified to account for these possible interferences and confounders. Therefore, result-based conclusions and other inferences pertaining to this interventional strategy may have also been somewhat exaggerated.
6. Conclusions
- This very brief study showed that a strategy that combines prescriber recommendations for PA and arrangements to provide motivational supports for engagement and participation is effective in promoting PA among individuals 60 years and older receiving routine care from primary care facilities. Modified perceptions of importance of clinical benefits of physical activity that was achieved by written recommendations of activity regimens and referrals to a motivational support program by providers augmented response to motivational supports. However, further studies will be required to measure overall health impacts of this strategy.
ACKNOWLEDGEMENTS
- The authors will like to thank Blue Cross and Blue Shield Foundation of North Carolina, all participants, practitioners, students, facilities and organizations that were involved in this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML