-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2017; 6(1): 1-3
doi:10.5923/j.ijpt.20170601.01

Acute Stroke Secondary to Tuberculous Meningitis: A Case Report and Review of Literature
Saeed Razmeh , Amir Hasan Habibi , Zahra Ghorchian , Monireh Eslami , Ghazal Haeri
Neurology Department, Rasoul Akram Hospital, Iran University of Medical Science, Iran
Correspondence to: Saeed Razmeh , Neurology Department, Rasoul Akram Hospital, Iran University of Medical Science, Iran.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Ischemic stroke is a sudden onset of a focal neurologic deficit that can cause morbidity and mortality in the countries. The etiology of ischemic stroke is so numerous. Cerebral vasculitis secondary to tuberculous meningitis is a rare cause of it. We report a 27-year old male man who developed multiple cerebral infarctions as the first manifestation of tuberculous meningitis and discusses that full work up for every patient with atypical and young stroke should be done.
Keywords: Tuberculous meningitis, Acute stroke, Cerebral vasculitis
Cite this paper: Saeed Razmeh , Amir Hasan Habibi , Zahra Ghorchian , Monireh Eslami , Ghazal Haeri , Acute Stroke Secondary to Tuberculous Meningitis: A Case Report and Review of Literature, International Journal of Prevention and Treatment, Vol. 6 No. 1, 2017, pp. 1-3. doi: 10.5923/j.ijpt.20170601.01.
1. Introduction
- Tuberculous meningitis is the most dangerous form of tuberculosis. It accounts for 9.1% of extrapulmonary TB cases. The early manifestations are low-grade fever, malaise, headache, confusion and stiff neck that may evolve during the weeks and months to stupor, coma and death so it is essential to diagnose and treatment TB meningitis early in the course of the disease [1, 2]. Ischemic stroke is a sudden onset of focal neurologic deficit due to occlusion of cerebral blood vessels. It is the important cause of morbidity and disability in the countries. The etiology of ischemic stroke is so numerous but cerebral vasculitis secondary to tuberculous meningitis is very unusual [2, 3]. This case report presents a case of acute Ischemic stroke as the first manifestation of TB meningitis.
2. Case Report
- A 27 years-old man was referred to our hospital with chief complaint of acute onset of left hemiparesis, confusion and agitation. He also had a history of headaches, lethargy and mild fever since 2 weeks ago. His family reported no history of blurred vision, double vision, seizure, cough and dyspnea. In family history his mother suffered from tuberculosis than two years ago. In physical examination, she was confused without orientation to time, place and person. He had no neck vein engorgement, no carotid bruit. Chest examination was normal. Cardiac rhythm and rate were normal with no murmurs. Abdomen was flat, soft and non-tender with normal liver and spleen. Extremities had normal findings. Muscle strength was 2/5 over both left upper and lower extremities and all deep tendon reflexes were normal and plantar response was bilateral extensor. A computed tomography (CT) of the brain revealed severe brain swelling and diffuse hydrocephalus. Cerebrospinal fluid (CSF) from a lumbar puncture revealed a white cell count (WBC) of 120/µL, a lymphocyte count of 80%, a protein level of 246 mg/dL, a glucose level of 23 mg/dL, negative results on India ink staining and a closing pressure of 25 cm H2O. Initial laboratory data showed a WBC count of 22000/μL, a serum glucose level of 130 mg/ dL, and normal liver and renal function test results. The initial chest film showed no definite active lung lesion. DWI and apparent diffusion (ADC) reveal acute infarctions in the pons, midbrain, temporal and internal capsule (Figure 1). Serology tests for human immunodeficiency virus and HCV and HBV were negative. He was started on dexamethasone and combination of ceftriaxone, vancomycin, and acyclovir and anti-TB and transferred to the neurosurgical unit for ventriculoperitoneal shunting. The second CSF study showed persistent pleocytosis and analysis of CSF was negative for bacterial culture, herpes simplex polymerase chain reaction result, but polymerase chain reaction for Mycobacterium tuberculosis (TB PCR) was positive. Ventriculoperitoneal shunting resulted in no neurological improvement. He succumbed to tuberculosis 4 days after the operation.
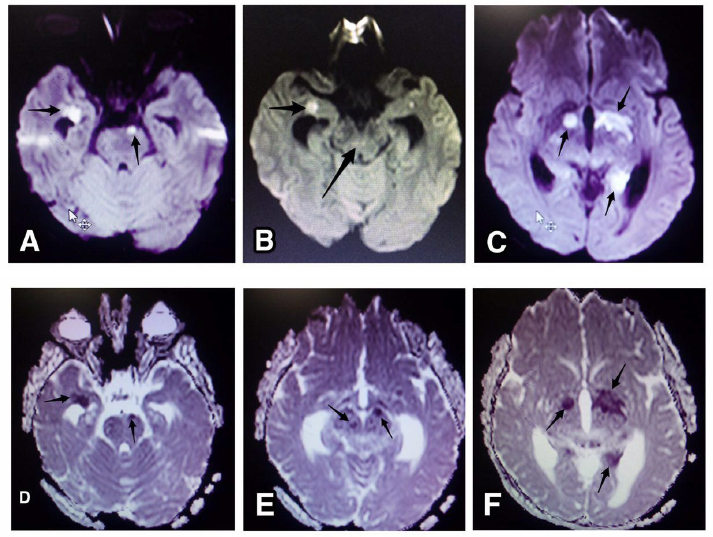 | Figure 1. Axial diffusion-weighted image (A,B,C) and apparent diffusion coefficient (D,E,F) reveals acute infarctions in the pons, midbrain, temporal and internal capsule |
3. Discussion
- TBM is a severe form of TB that cause high mortality and morbidity rates especially in individuals with immunosuppression [4]. The disease is difficult to diagnose because it develops slowly with different signs and symptoms and can be misdiagnosed with other diseases. The cardinal features of TBM include fever, headache, malaise, confusion, meningeal signs and focal neurological deficits [5]. The risk for TB meningitis includes immunodeficiency, malignancy, HIV infection, malnutrition, Diabetes mellitus, alcohol abuse, chronic kidney disease and silicosis’s [6, 7]. Cerebral vasculitis is a rare disorder that causes inflammation of cerebral blood vessel walls. It has many different etiology. Cerebral vasculitis due to tuberculous (TCV) is a catastrophic complication of TBM that accounts for secondary cerebral vasculitis. Appenzeller S and colleagues reviewed the MRI findings in clinically suspected cases of vascular involvement with systemic diseases. Underlying causes for CNS vasculitis were identified in all patients that three of these 29 patients had tuberculosis [8] TCV has different symptoms, including paresis, dysarthria, impaired consciousness, ataxia and ophthalmoparesis. So always should be considered TCV in the differential diagnosis of tuberculosis patients with the focal neurological deficit [9]. But in our case, there is no history of tuberculosis before the onset of symptoms that it is usually uncommon. Brain CT and MRI can contribute to diagnosing TBM and TCV but the role of CT is limited for detecting acute hydrocephalus for surgical management. MRI with high accuracy and sensitivity than CT can diagnose TBM by detecting basal enhancement in more patients and small infarctions in different part of brain, in this condition CT may even be normal [9-11]. In our patient BRAIN MRI show acute hydrocephalus with periventricular edema and in BRAIN DWI MRI, show multiple bilateral acute infarctions in midbrain, internal capsule and temporal. Prognostic factors of tuberculous meningitis include old age, Comorbidities especially concomitant pulmonary tuberculosis, impaired consciousness with the focal neurological deficit on admission, hydrocephalus and increasing time-to-treatment initiation. Treatment for TB meningitis and vasculitis include antituberculous regimens in combination with Corticosteroids [12, 13]. This treatment, lowers the risk of death and neurological sequelae. Corticosteroid has an important role in this regime because some believed that cerebral vasculitis can be caused by the immunological mechanism in addition to by direct invasion of the vessel wall [14]. And in the randomized controlled trial, Thwaites GE and colleagues show treatment with dexamethasone reduced the risk of death or severe disability in patients with tuberculous meningitis, with or without HIV infection [15]. In Conclusion In any patient with focal neurological deficits especially young patient with a history of fever, confusion and meningeal signs, other rare causes like infectious vasculitis should be considered. It is unusual clinical presentations of infectious disease such as tuberculosis but delay in diagnosis can cause catastrophic complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML