-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2016; 5(2): 22-24
doi:10.5923/j.ijpt.20160502.02

Schistosoma mansoni Infestation Rate Evaluation by Kato Katz’s Method in Haute Matsiatra Region (Madagascar) School Environment
Rakotozafy J. C. R.1, Tanamasoandro R.1, Rakotoarimanana R.2, Raherimandimby H.2, Randriamamonjy F.2, Rasoloherimampiononiaina M. R.3, Rabarijaona M.3
1Laboratory of Molecular Biology, Faculty of Sciences – University of Fianarantsoa, Madagascar
2Laboratory of Biomedical Analysis, Center Hospital University of Fianarantsoa, Madagascar
3Center Hospital University of Fianarantsoa, Madagascar
Correspondence to: Rakotozafy J. C. R., Laboratory of Molecular Biology, Faculty of Sciences – University of Fianarantsoa, Madagascar.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

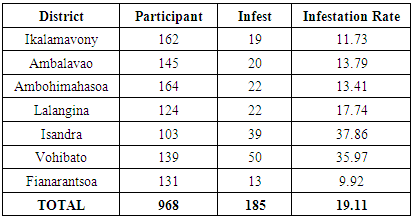
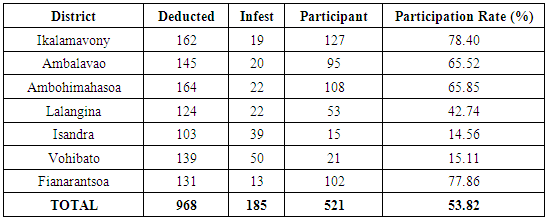
Schistosomiasis infestation rate evaluation achieved to Public Primary School by the Kato-Katz's method in Haute Matsiatra Region (Madagascar) showed that on 968 examined, 185 are carriers of Schistosoma mansoni eggs. Isandra and Vohibato districts are the more touched with an infestation rate to 37.86% and 35.97%. The weak infestation rate is in Fianarantsoa district (9.92%). This intestinal parasite scattering of the aforesaid region is in extension. It is therefore important to recommend the means to reduce this expansion. This survey gives bases on the future geoschistosomiasis of Schistosoma mansoni in Haute Matsiatra region.
Keywords: Haute Matsiatra, Kato-Katz’s, Madagascar, Schistosoma mansoni
Cite this paper: Rakotozafy J. C. R., Tanamasoandro R., Rakotoarimanana R., Raherimandimby H., Randriamamonjy F., Rasoloherimampiononiaina M. R., Rabarijaona M., Schistosoma mansoni Infestation Rate Evaluation by Kato Katz’s Method in Haute Matsiatra Region (Madagascar) School Environment, International Journal of Prevention and Treatment, Vol. 5 No. 2, 2016, pp. 22-24. doi: 10.5923/j.ijpt.20160502.02.
Article Outline
1. Introduction
- The schistosomiases is a chronic illness provoked by parasitic worm. The victims are infected in the setting of current agricultural activity, domestic, professional or recreative, including exposition to a contaminated water. Lack of hygiene and some habits of children school-age game, as swimming or fishing in infested waters make children vulnerable to the infection. The struggle against the schistosomiases focuses on patients’ number reduction of population periodic treatments by Praziquantel; as well as struggle against gastropods should also make regress the transmission [1]. In 2014, at least 258 million people in the world needed a preventive treatment against schistosomiases. More of 61.6 million have been treated. Mortality due to schistosomiases varies between 20 000 and 200 000 deaths per year [2].Schistosomiases prevalence area is located in tropical and subtropical regions, at resourceless communities. Less than 90% of people need treatment live in Africa. Schistosomiases touches particularly agriculturists and fishers poor populations. Women doing their domestic tasks in the infested water are also exposed to the risk [3]. In Madagascar, according to the statistics held by Ministry Health and CHU/F statistical service in Fianarantsoa, the topics parasitized by Schistosoma mansoni number is estimated to 2 million of which fourth (25%) at Haute Matsiatra region [4].The intestinal schistosomiasis is much spilled in tropical zones, it explains by fecal hygiene lack of population especially the children. Consequently, the survey has been fixed to children at Public Primary school. The objective is to evaluate Schistosoma mansoni infestation rate in school environment, in order to put an efficient and perennial local strategy to fight against this parasite.
2. Materials and Methods
2.1. Study Population
- Children from seven districts (Ikalamavony, Ambalavao, Vohibato, Isandra, Lalangina, Ambohimahasoa, Fianarantsoa I) constituted the cohort of study. The first step method consisted of an information session about schistosomiases offered to pupil’s parent in each Public Primary School. The parents were asked to participate voluntarily in the study by filling out a questionnaire of requesting age and the different factors and cofactors that can contract the schistosomiases of their children.The consent form, the questionnaire and the information pamphlet were written in Malagasy language to facilitate the communication. Sterile plastic bags (10 x15 cm) were used for fecal withdrawal. All specimens and corresponding questionnaires were carried out to laboratory for analysis.Schistosomiases eggs research at the fecal is done according to the Kato - Katz's method (Kato Katz’s Kit from Department of Helminthology, Faculty of Tropical Medicine, Mahidol University Thailand) (figure 1). Briefly, a small amount of fecal material was placed on absorbable paper and a piece of nylon screen was pressed on top so that some of the feces sieved through the screen and accumulated on top. A flat-sided spatula was scraped across the upper surface of the screen to collect the sieved feces. A template was placed on the slide and the sieved feces were added with the spatula so that the hole in the template was completely filled. The spatula was passed over the filled template to remove excess feces from the edge of the hole. The template was removed carefully so that a cylinder of feces was left on the slide. The fecal material was covered with a pre-soaked cellophane strip.
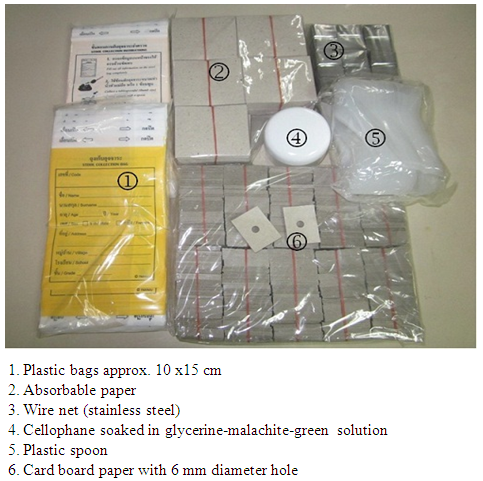 | Figure 1. Kato Katz’s kit |
2.2. Statistical Analysis
- Comparison Schistosoma mansoni rate infestation and Praziquantel treatment rate involvement of 7 districts (n=7) has been studied. The statistical analysis of the qualitative and quantitative variables was either of monovaried type, or of multivariate type using a software Epinfo version 6. The Student test was used for the comparison of the averages and the variances and the test of Chi-2 for the comparison between the rates and a significant value if p<0. 05.
3. Results and Discussions
- During the study, 968 pupils have been appropriated that 162 Ikalamavony, 145 Ambalavao, 164 Ambohimahasoa, 124 Lalangina, 103 Isandra, 139 Vohibato and 131 Fianarantsoa. Among the 968 pupils, 185 are carriers of Schistosoma mansoni eggs (Table 1).
|
|
4. Conclusions
- This survey confirms that Schistosomiases infection exists in Haute Matsiatra region. Even that the study is centered only on Public Primary School pupils, the results permit to say that this parasite disperses itself in rural area. The survey also shows that schistosomiases infection depends on population daily activity and socioeconomic statute. Questionnaire analysis of Praziquantel treatment and local population behavior was not conclusive to the effect on schistosomiases infection. From this survey, tracking program feasibility for all population using Kato Katz’s technique is an essential question. In perspective, different probable sources and schistosomiases high risk infection analysis will be important in order to determine efficient preventive struggle in this region.
ACKNOWLEDGMENTS
- This work was made possible with the “Fondation Mérieux – Lyon (France) and Center Hospital University of Fianarantsoa (Madagascar).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML