-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2016; 5(1): 7-11
doi:10.5923/j.ijpt.20160501.02

Saudi Nurses' Level of Knowledge Regarding to Pressure Ulcer Preventive Measures
Magda M. Bayoumi1, Enas Bassuni2, 3
1Medical Surgical Nursing Department, Faculty of Nursing, Buni-Suef University, Egypt
2Lecturer of Nursing Administration Department, Faculty of Nursing, King Khalid University, KSA
3Faculty of Nursing, Cairo University, Egypt
Correspondence to: Magda M. Bayoumi, Medical Surgical Nursing Department, Faculty of Nursing, Buni-Suef University, Egypt.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: A pressure ulcer is an injury to the skin that occurs when a patient lies or sits too long in the same position. All nurses are at the forefront of predicting patients at risk for PU. Of course the prevention of PU has generally is considering the responsibility of nursing staff. Healthcare professionals need to be able to benchmark the care they deliver against standards that ensure the patient receives the best possible care. Aim: to evaluate the nurses' knowledge regarding bedsores’ preventive measures at Saudi Arabia. Methods: Descriptive (cross- sectional study). This study was conducted at General Mohyeil Hospital and Rijal Alma Hospital, from October 2012 to February 2012. The study sample consisted of 38 staff nurses from different departments or units. Results: In the study sample the characteristics of staff nurses were both sex, ranged from 24 years (50%) to 43 years (15.8%), are working in different areas medical (42.11%), surgical (13.2%), ER (13.2), ICU (21%), and 10.5 in artificial kidney unit, the majority of the nurses (76.3%) pay attention to give the patient and family health education about how to prevent bed sores. In addition there are significant correlation (0.026) between years of experiences and don’t elevate the high risk patient above 20 degree. Conclusions: The study concluded that prevalence of pressure sores are developing at factors, also nurses knowledge were good in comprehensive skin assessment within 24 hours of admission. As well as most of nurses were not conscious regarding the degree of bed elevation for high risk patient.
Keywords: Nurses, Knowledge, Bed sores
Cite this paper: Magda M. Bayoumi, Enas Bassuni, Saudi Nurses' Level of Knowledge Regarding to Pressure Ulcer Preventive Measures, International Journal of Prevention and Treatment, Vol. 5 No. 1, 2016, pp. 7-11. doi: 10.5923/j.ijpt.20160501.02.
Article Outline
1. Introduction
- Refers to a reduction in the amount and control of movement a person has. Normally people move when they experience discomfort due to pressure on an area of the body. Healthy people rarely exceed their tolerance to pressure. However; Paralysis, extreme weakness, pain, or any cause of decreased activity can hinder person's ability to change positions independently and relative the pressure, even if the person can perceive the pressure [1].Pressure ulcer (PU) Pressure ulcers, commonly called pressure sores or bedsores, are localized areas of cellular necrosis that occur most often in the skin and subcutaneous tissue over bony prominences. These ulcers may be superficial, caused by local skin irritation with subsequent surface maceration, or deep, originating in underlying tissue. Deep lesions often go undetected until they penetrate the skin, but by then, they've usually caused subcutaneous damage. Most pressure ulcers develop over five body locations: sacral area, greater trochanter, ischial tuberosity, heel, and lateral malleolus. Collectively, these areas account for 95% of all pressure ulcer sites. Patients who have contractures are at an increased risk for developing pressure ulcers due to the added pressure on the tissue and the alignment of the bones [2].Recent researches reported that pressure ulcer is remains a major health problem among high risk hospitalized patient particularly critically ill patients. Unfortunately pressure ulcers have been reported in all health care setting at many countries as a major health problems [3]. Because all nurses are at the forefront of predicting patients at risk for PU [4]. Moreover the prevention of PU has generally is considering the responsibility of nursing staff [5]. Although many previous studies shown nurses knowledge of PU management have had conflicting result; knowledge are good in some studies and poor in others [6]. Furthermore successfully prevention of bed sores requires that nurses have adequate knowledge of this complication [7]. Whereas prediction and prevention of PU involve health care personnel in many disciplines, nurses are patients’ primary caregivers plus they have the most responsibility for preventing and managing this complication [8]. In Saudi Arabia, At King Abdul-Aziz University Hospital (KAUH) is one of the larger sized governmental hospitals in Jeddah, with a total bed capacity of 878. And the study reported the rate of pressure ulcers development was decreased per 1000 admissions [9]. Despite the increased expenditure on PU prevention strategies, incidence and prevalence is increasing [10]. However it becomes to be a major societal health problem, greatly affecting patients and their caretakers. As well as still as a major cause of admission to hospitals for patients with impaired mobility and sensory function and for elderly patients [11].Therefore in Saudi Arabia no research done to answering what is the staff nurses' knowledge regarding preventive measures that taken to minimize the occurrence of PU at Saudi Arabia hospitals.Aim of the study: to evaluate the nurses' knowledge regarding bedsores’ preventive measures at Saudi Arabia.
2. Subjects and Methods
- Research designA cross-sectional descriptive study design was carried out in the present study. Setting:This study was carried out at Regal-Alma hospital and General Mohail Hospital in the following units (Medical, Surgical, ICU, Dialysis Unit & Emergency).SubjectsThe subject of this study comprised of selected number of staff nurses who met the following criteria: Both gender, one year of experience or more, working at high risk unit for PU. Determination of the sample size (38) who were chosen from above mentioned units at Mohail general hospital and Regal Almaa general hospital. The sample size was estimated as convenience sample. The study was conducted between October 2012 and December 2012.Ethical Consideration:The study was approved by the appropriate ethics committee. Staff nurses were informed about the purpose of the study and about their rights to refuse or withdrawal at any time.Instrument:The questionnaire was consisted of two parts first parts:Part I: socio-demographic data (age-sex-unit-graduation year-total years of experiences, and years of experience in current unit. Part II: the observational checklist for the role of nurses in process of care for high risk patients, each question is scored in a likert-type scale of 1-3 (based on the nurse’s replies (done, Not done, Not applicable). To calculate as a positive score for a given factor, the survey respondent must answer yes to all related items. Statistical Designs:Collected data was arranged, tabulated and analyzed according to the type of each data.Scoring system:Scoring system was ranged from 1 to 3scores 1 = for yes, 2 = NO and 3 for Not Applicable.Statistical analysis:Data analysis:Data was collected and entered into a database file. Statistical analysis was performed by using the SPSS 16 computer software statistical package. Data was described by summary tables. Statistical significance was considered at P-value <0.05 and highly significance at P-value <0.00.
3. Results
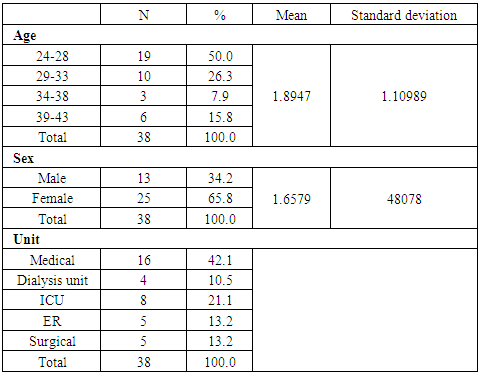
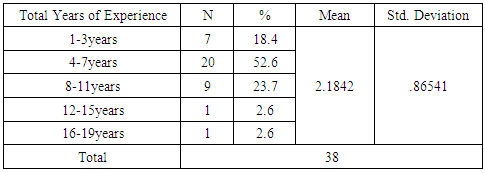
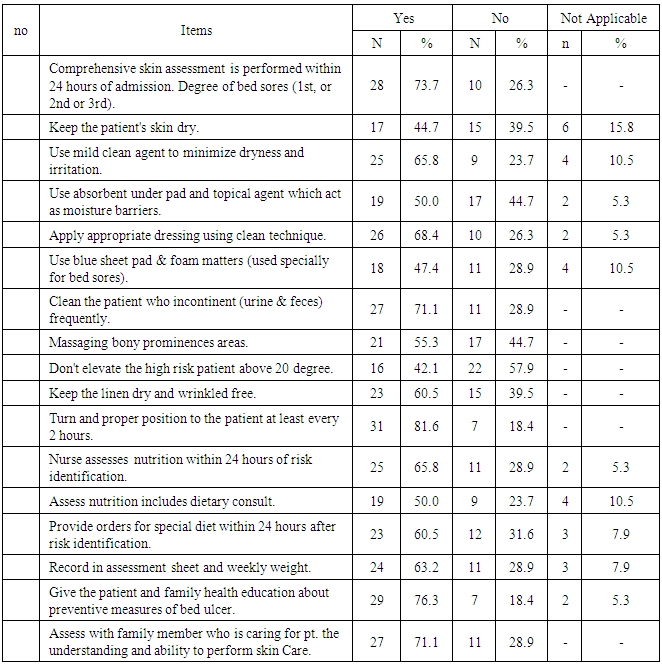
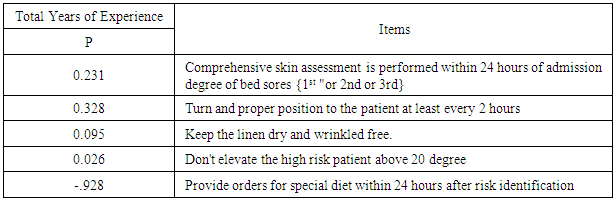
- Table 1 shows that the age of participant was ranged between 24 (50%) to 43(6) years, with mean score 1.895±1.1098, from both sex 65.8% were females and 34.2% were men. In addition they distributed in different units in hospitals medical 42.1%, surgical 13.2% and ER 13.2%, while the graduation years was ranged between 20 years (7.9%) to one year (5.3%), however the majority of the nurses graduation year was ranged between 4 year to eight year (60.5%). Table (2) presents that more than half 52.6% of staff nurses' total years of experiences ranged between 4:7 years, while 18.4% ranged between 1:3 years of experiences with mean and stander deviation 2.1842±.86541.The finding revealed that nearly three quarter of the nurses 73.7% done of those items during providing care for high risk patients as comprehensive skin assessment is performed within 24 hours of admission; keep the patient's skin dry; use mild clean agent to minimize dryness and irritation if used what it is; use absorbent under pad and topical agent which act as moisture barriers; don't elevate the high risk patient above 20 degree; turn and proper position to the patient at least every 2 hours; Nurse assess nutrition within 24 hours of risk identification; and Assess nutrition includes dietary consult. Furthermore the majority of all participating nurses rated 81.6% nurses done in relation to turn and proper position to the patient at least every 2 hours. While 42.1% nurses rated done for “Don’t elevate the high risk patient above 20 degree". As well as 10.5% nurses were not applicable in relation to Use mild clean agent to minimize dryness and irritation as documented is shown in Table (3). Table 4 shows that the significant relationship between staff nurses' years of experiences and their knowledge regarding keep the linen dray (p=.095), while nurses knowledge regarding Provide orders for special diet within 24 hours after risk identification (-.928) correlate negatively with the nurses years of experiences.
|
|
|
|
4. Discussion
- PU is one indicator of quality of nursing care and causes anxiety and stress for all nursing staff, however the PU prevention and management is a vital part of nursing practice [12].In this study we recruited a sample which represented different sex, age, departments, units and different year of experience. Although nurses years of experiences was ranged between 1 year to 19 years, the most of the sample (above half) were had 4-7 years of experience; this high level of experience may be considerable as positive correlation with don't elevate of high risk patients above to 20 degree and Keep the linen dry and wrinkled free. These findings supported by Tweed; 2008 who mentioned while the nurses' years of experience was high that lead to high level of knowledge of pressure ulcer prevention and management [13]. This result congruent with the Pieper & Mattern 1997 study reported that no difference in different level of experiences and level of performance regarding PU prevention [14, 15]. However, nurses who had been in their current position for more than 5 years were less knowledge than staff nurses whose appointments were more recent.As regards nurses who provide care; our study finding revealed that the above two third of the sample providing care for high risk patients as comprehensive skin assessment within 24 hours of admission, turn and proper position to the patient at least every 2 hour. Other results in the same line for Black et al 2011 who mentioned that most PUs are avoidable, while our finding congruent with Banjar 2012 who stated that no one of the nurses provided care for high risk patients in 24 hours of admission [3, 16].Whereas there are highly significant correlation between balanced diet; when increase protein, calories intake and A, C, or E vitamin supplements risk of PU will be decreased [17, 18].We found only fifty percent of the studied sample assess nutrition include dietary consultant this may be due to defect of nurses knowledge regarding importance of balanced meals and attention to specific food components especially in susceptible patients to PU. Regarding to the use of specific bed matters (foam mattress) the result of this study revealed that less than half of the study sample was use specific matters, this may be due to less hospital facilities. This result agreed with McGough (2009) & Hampton (2007) who reported that, using of redistributing device should be based on an overall patient assessment and using specialized support surface such as mattresses can reduce or relieve PU [19, 20].
5. Conclusions
- The study concluded that nurses knowledge were good in comprehensive skin assessment within 24 hours of admission. As well as most of nurses were not conscious regarding the degree of bed elevation for high risk patient.
6. Recommendations
- √ Repositioning by the caregiver every 2 hours or more often if indicated, with support of pillows for immobile patients; a pillow and encouragement to change position for those able to move √ Foam, gel, or air mattress to aid in healing by reducing pressure on the ulcer site and reducing the risk for more ulcers √ Foam, gel, or air mattress on chairs and wheelchairs as indicated √ Nutritional assessment and dietary consult as indicated; nutritional supplements, such as vitamin C and zinc, for the malnourished patient; monitoring serum albumin and protein markers and body weight √ Adequate fluid intake (I.V. if indicated) and increased fluids for a dehydrated patient √ Good skin care and hygiene practices (for example, meticulous hygiene and skin care for the incontinent patient to prevent breakdown of the affected tissue and skin) √ Stage II, cover ulcer with transparent film, polyurethane foam, or hydrocolloid dressing √ Stage II or IV, loosely fill wound with saline- or gel-moistened gauze, manage exudate with absorbent dressing (moist gauze or foam) and cover with secondary dressing √ Clean, bulky dressing for certain types of ulcers, such as decubiti √ Surgical debridement for deeper wounds stage III or IV as indicated [21]
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML