-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2015; 4(2): 23-28
doi:10.5923/j.ijpt.20150402.01
Comparison of the Use of Kinesio Tape and Shorts Stretch Bandage to Changes in Volume of the Peripheral Blood Flow
Asuman Saltan1, Yeşim Bakar2, Handan Ankarali3
1Yalova University Termal Vocational School Yalova, Turkey
2University of Abant İzzet Baysal, KD School of Physical Therapy and Rehabilitation, Bolu, Turkey
3University of Düzce, Faculty of Medicine, Department of Biyostatistic. Düzce, Turkey
Correspondence to: Asuman Saltan, Yalova University Termal Vocational School Yalova, Turkey.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Backround: The present literature and clinical practice provide support for the use of bandaging in reducing edema. However, the taping for edema still remains relatively poorly understood. Moreover, recent studies suggest that there is a need for evidence regarding the bandaging and taping techniques.Objectives: The purpose of study is to compare the treatment effect between tapes and bandages on acute edema.Experimental, randomized study.Methods: The edema was created by the tourniquet application for 20 minutes on the lower right leg of rabbits. A total of 21 male New Zealand white rabbits were randomly placed into a kinesiotape group (n = 7), a bandage group (n=7), and a control group (n=7). After the edema, the low stretch multilayered compressive bandage (n=7) and kinesiotape (n=7) were used for 20 minutes. The circumferancial measure, the blood flow rate, and the heart rate were calculated before and after the turnique and after each implementation. Results: The excess limb size (circumference) was reduced significantly after the applications so as to compare it after the tourniquement (p=0.002). No significantly interactions between groups and evaliation times regarding the circumference, heart rate, and blood flow velocity values were found. Conclusions: This study provides an experimental method for future studies. These study results show that there were no significant differencies between the two treatment methods (tape and bandage) on acute edema. The low stretch multilayered compressive bandage can be safely used for acute edema.
Keywords: Taping, Bandages, Tourniquets, Rabbits
Cite this paper: Asuman Saltan, Yeşim Bakar, Handan Ankarali, Comparison of the Use of Kinesio Tape and Shorts Stretch Bandage to Changes in Volume of the Peripheral Blood Flow, International Journal of Prevention and Treatment, Vol. 4 No. 2, 2015, pp. 23-28. doi: 10.5923/j.ijpt.20150402.01.
Article Outline
1. Introduction
- Compression therapy is an accessible and popular modality in the treatment of injury. For treatments of injury, increasing the amount of blood flow is one of the mechanisms in the healing process. The accumulation of fluid and edema around an injury site also increases tissue damage, delays healing, and can result in some degree of chronic disability [1, 2].The purpose of compression is to stop hemorrage and reduce swelling. Compression is applied to limit the amount of edema caused by the exudation of fluid from the damaged capillaries into the tissue [1-3]. Controlling the amount of inflammatory exudate reduces the amount of fibrin and ultimately the production of scar tissue which helps to control the osmotic pressure of the tissue fluid in the injured area [1-5].According to Block JE [3] compression modalities must provide the patient with the maximum degree of comfort and the shortest time to functional recovery. Bandages, elastic wraps, and intermedıate pressure devıces are always used for edema [3]. Studies in which modality must be choice is definitely not due to studies not only including the using of modalities; therefore, there is no evidence concerning edema treatment [2, 4, 5]. The present study includes no treatment groups; thus, our results alone provide the only effects of the modalities.A multilayer bandage can only be stretched a little, and is usually used to maintain the volume reduction from the manual lymphatic drainage. It provides mild pressure during resting, and creates higher pressure during muscle contraction to prevent skin extension. The lymphatics are compressed between the muscle and the bandage, causing them to be manually pumped [6].As we know, the immediate effect is the most important in the recovery of edema. Kinesio tape (KT) may be an alternative option in the treatment of edema, especially when an immediate effect is needed [7, 8]. Dr. Kase claimed that applying KT would have physiological effects, including removing the congestion of the lymphatic fluid or hemorrhages under the skin [6, 9]. This mechanism has no effect on compression for solving edema [9]. After applying the KT, the taped area will from convolutions to increase the space between the skin and the muscles. Once the skin is lifted, the flow of blood and lymphatic fluid is promoted. This helps to give more space and take the pressure off the interstitial fluid. The popularity of the application of tape during the rehabilitation process, shows the need for empirical evidence on the effect of KT [2, 8]. At the same time, the purpose of the study is to compare the immediately effect of both the KT and bandage on edema.The specific null hypothesis included the following: 1) No differences existed in the outcome measurements between using a bandage or no treatment in the immediate effect on the edema.2) No differences existed in the outcome measurements between using the tape and no treatment in immediate effect on the edema.3) No differences existed in the outcome measurement between using the tape and bandage in the immediate effect on the edema. Our study will be helpful in the further development of evidence-based treatment recommendations and protocols.
2. Materials and Methods
- All the procedures were approved by the institutional animal care and use committee. A total of 21 male New Zealand white rabbits were randomly placed into a KT group (n=7), a bandage group (n=7), and a control group (n=7). Experimental animals weighing 2.5-3.0kg were administered the mixture of ketamine chloride (35 mg / kg) and xylazine chloride (5 mg / kg) intramuscularly using a syringe pump, and anesthesia was provided. The anesthesia was maintained during the experiment when necessary (1.6ml / kg / hr.). The sub-anesthesia level was followed with the monitoring of the respiratory pattern and finger pinch reflex. The fur of the anterior face of the right hind leg and the dorsal part of the leg was cut. Thus, the application area was free of any hair. The body temperature of the animals was controlled at 37.8-39.2°. Initially, the measurements of the circumference and the Doppler (for the blood flow and the pulse) were carried out without applications (no KT and bandage) on the rabbit (n=21). Then, the edema was allowed to form by applying a tourniquet over the popliteal lymph nodes for 20 minutes. The resulting edema circumference was evaluated with a tape measure after applying a tourniquet. The volume of the peripheral blood flow and pulse was measured again after applying the tourniquet. Then, the KT were applied for a 20 min period to the rabbits (n=7). In this manner, the KT group was created. The short stretch bandage was applied for a 20 min period to the rabbits (n=7). The bandage group was created in this way. No application was carried out on the control group (n=7). The kinesio taping was applied to the areas most likely to affect the blood circulation. Taping is not applied to the pathway of the lymph flow. As we know, it is necessary to first open up the areas that the lymph will be draining towards. This study did not include manual lymph drainage. KT was applied from the proximal to the distal on the limb using the grill method (Figure 1). The short stretch bandage was applied from the metatarsophalangeal joints to the poplitea (Figure 2).
 | Figure 1. Application of Kinesio tape |
 | Figure 2. Application of bandaging |
2.1. Statistical Analysis
- Descriptive statistics were computed as mean±SE (Standart Error of Mean) for variables in each subgroups. Two factor repeated measurement analysis of variance with one factor within (time periods) and one factor between (groups) were used to compare “different times”, “groups” and “times x group interaction” with regard to pulse, circumferences, and blood flow followed by the Tukey’s multiple comparisons test. The level of p < 0.05 was considered as statistically significant. All statistical computations were done by using the SPSS (ver.18.0) program.
2.2. Results
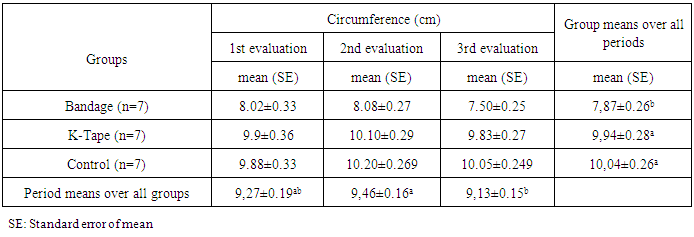
- There was no significant interaction between the groups and the measurement time (p = 0.134) as a result of the comparison performed in terms of the measurement of the circumference. Accordingly, it can be said that the difference between the groups depending on the time of the measurements did not change. Considering the difference between groups, it was determined that there was a significant difference between the bandage with the control (p = 0.0001), and between the bandage with the KT (p = 0.0001). According to the these results, it can stated that the control was significantly higher compared to the bandage, and a significantly a higher average was abtained in the KT group compared to the bandage in the normal one, both after the tourniquet and the other applications. However, the difference between the control group and the KT group was not significant, and this result did not change in the normal group after tourniquet and after the applications either. In addition, when the differences between the measurement times were examined, it was found that these differences did not change from group to group (p=0.085). There was no significant difference between the normal group after the applications (p=0.294), but the circumference measurements after the tourniquet were determined to be significantly higher compared to the measurements after the application (p=0.002). The descriptive statistics for each the measurement times and the circumference measurements of each group are given in Table 1.
|
|
|
2.3. Discussion
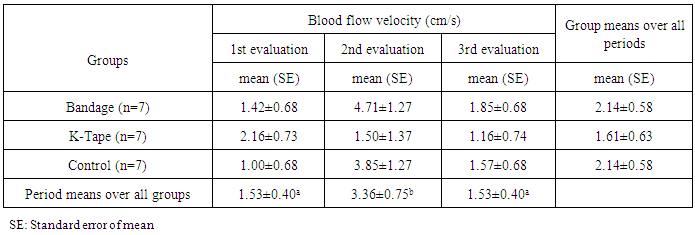
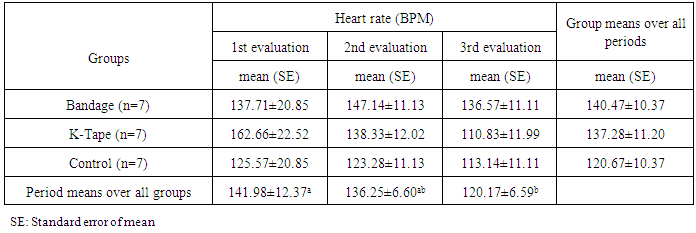
- Our study is the first experimental study comparing KT and short-stretch bandage applications. In our study, the effects of two important applications commonly used for edema were investigated experimentally. No significant differences statistically in volume change outcomes were found among the three groups. There were no changed values in the circumference, blood flow, and pulse were found. However, this study proved that there were no statistically significant differences in the pulse values and blood flow values. According to the mathematical calculations the short-stretch bandage, showed that it is capable of putting pressure on the tissue, the KT, which has a property of adhesion to the skin, was effective on the edema without affecting the arterial blood circulation. It can be said observationally and subjectively that both applications of the KT and short-stretch bandage were effective on the edema, but the short-stretch bandage provided more impact.Also, according to these mathematical calculations we can interpret subjectively the immediately effects of both methods. Here are some mathematical calculations for subjectively results. When the data in Table 1 was analyzed, the average differences of the circumference measurement were given for the control, the KT and the bandage groups: the difference between the 1st and 2nd measurements (1.32cm, 1.10cm 0.06 cm); the difference between the 2nd and 3rd measurements (0.15cm, 0.27cm 0.58 cm) and the difference between the 1st and 3rd measurements (0.17cm, 0.52cm and 0.07 cm). We can suggest that tourniquets can be used to create edema without requiring surgical procedures in order to increase the rate and the number of applications, because the values of the circumference measurement increased in all three groups after the tourniquet. The results obtained also evaluated the efficacy of the tourniquet application used to create the edema in the experimental animals while at the same time exhibiting the effectiveness of the applications. This study would suggest that tourniquets can be used to create edema without requiring surgical procedures in order to increase the rate and the number of applications because the values of circumference measurement increased in all three groups after tourniquet. However, it was calculated mathematically that the edema that formed through the tourniquet was the highest in the control group (1.32cm). However, when the mean differences in the 1st and 3rd circumference measurements of the control group were evaluated, it was observed that the edema still continued with a difference of 0.17 cm. The reduction in the edema was observed in the groups that underwent the application. The most important difference here, was that a reduction in the edema that was provided in the bandage group (0.52cm) was greater than the KT group (0.07 cm). Based on this, it can be said that both observationally and subjectively both the applications of the KT and short-stretch bandage were effective on the edema, but the short-stretch bandage provided more impact.We analyzed how the pulse values were affected by the applications. When the differences of the average value of the pulse of the KT group (the difference in the 1st and the 2nd measurements (0.66cm / s); the difference in the 2nd and 3rd measurements (0.34cm / s) and the difference in the 1st and 3rd measurements (1.00cm / s)) were calculated mathematically for the three measurement times, it was observed that the values had a continuous downward trend. However, the pulse values of the bandage group, particularly in the period after the application [the difference in the 1st and 2nd measurements (3.29cm/s); the difference in the 2nd and 3rd measurements (2.86cm/s); the difference in the 1st and 3rd measurements (0.43cm/s)] and the control group [the difference in the 1st and 2nd measurements (2.85cm/s); the difference in the 2nd and 3rd measurements (2.28cm/s); the difference in the 1st and 3rd measurements(0.57cm/s)] appeared to be high and close to the initial value. When the differences in the average values of the blood flow were calculated mathematically, and it was observed that the values behaved similarly in all the three groups. The blood pressure values, respectively: in the control group, the difference in the 1st and 2nd measurements (2.29bpm); the difference in the 2nd and 3rd measurements (10.14bpm) and the difference in the 1st and 3rd measurements (12.44bpm); in the KT group, the difference in the 1st and 2nd measurements (24.33bpm); the difference in the 2nd and 3rd measurements (27.50bpm), and the difference in the 1st and 3rd measurements (51.83bpm); and in the bandage group, the difference in the 1st and 2nd measurements (9.43bpm); the difference in 2nd and 3rd measurements (10.57bpm) and the difference of 1st and 3rd measurements (1.14bpm) all behaved similarly. A well-defined randomized controlled trial using this model could provide the clear evidence needed to guide decisions regarding the clinical application of tape and compression with immediate effect [8, 13-15]. Unfortunately, the studies are not uniform in their choices of experimental and control groups, study duration, sample size, or surgical procedure, which renders the “evidence” diluted. Previous reviews have attempted to disentangle the effects of tape and static compression to elucidate the independent contributions of each. The task has been daunting [14-17]. Additionally, because of the different indications for use, types of treatment modalities, and clinical heterogeneity, it was impossible to pool the results in a meaningful way with respect to some index of improvement.KT has become extremely popular recently; however, there remains a paucity of evidence on the use of KT for edema as well as other conditions [18].Finally, there is a lack of research comparing these two different methods for the treatment of edema.The purpose of this study was to compare the effectiveness of edema control in the immediate effect between the KT and the short stretch bandage on healthy tissue. The results revealed no significant difference to edema between the three conditions. Both the KT and the short stretch bandage were not effective in reducing edema when compared to the no application condition. The KT and short stretch bandage appear to be viable alternative methods for addressing the edema in case both of them had the same effect as no application. According to our results, the doppler indicated no major changes to the blood flow after the applications. Thus, we can say with some confidence that both of them have no major adverse effects. The ideal pressure, which can be applied on the artery by compression, is currently being investigated [19-21] This study provides additional information to the literature for studies investigating the pressure to be applied to the arteries in the region by the compression applied for the treatment of venous insufficiency, lymphedema, and edema etc. However, it is KT application which is the recommended option as an alternative to the short-stretch bandage application for clinical cases where arterial blood flow is not to be affected (venous insufficiency, lymphedema, and edema etc.).
3. Conclusions
- In conclusion, our study can make an important contribution to the literature as the first experimental study comparing KT and a short-stretch bandage application. However, individual and environmental factors that might influence the application were eliminated as much as possible because we completed our study as an animal experiment. The standard conditions were created for the application. In the homogeneous conditions provided, two application types, KT and short-stretch bandage applications, were compared and evaluated with the control groups. Therefore, the data with high evidence values, which can be a base for future studies, especially in the field of physiotherapy, have added to the literature.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML