-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2015; 4(1): 1-7
doi:10.5923/j.ijpt.20150401.01
The Effects of Low Dye Taping on Vertical Foot Pressure in Subjects with Plantar Fasciitis
Paolo Sanzo, Tony Bauer
School of Kinesiology, Lakehead University, Thunder Bay, Canada
Correspondence to: Paolo Sanzo, School of Kinesiology, Lakehead University, Thunder Bay, Canada.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Introduction and Objective:Heel pain secondary to plantar fasciitis (PF) continues to be common complaint. Gait analysis has led to inconsistent findings regarding lower limb loading patterns but it is thought that mechanical overload may contribute to the development of PF. Clinically, patients with PF often make subtle gait adjustments to reduce force under the foot to alleviate pressure and pain in the symptomatic foot. Therefore, the purpose of this investigation was to analyze the effect of low dye taping (LDT) on vertical foot pressure and the path of centre of pressure (COP) in individuals with PF. Methods:A one group, repeated measures design was used to assess 10 symptomatic individuals (6 females, 4 males; mean age 28 years ± 9.24, height 165 cm ± 9.73, and body mass 69 kg ± 3.96). All subjects had been medically screened and diagnosed with PF by their family physician.Subjects were tested under two conditions, completing 3 trials of walking with and without LDT with a 1 minute rest period between each trial. Vertical foot pressure and the COP were measured using the F-Scan Gait Analysis System.The data were analyzed using descriptive statistics and two way repeated measures ANOVAs. The rejection criteria were set at an alpha level p < .05. Results: Inferential statistics revealed a significant difference for the phase of gait, F(2,54)=321.73, p=.0005 with lower vertical foot pressures found at contact; there was also a significant difference for the taping condition, F(1,54)=105.42, p=.0005 with lower vertical foot pressures found with the application of LDT compared to the no taping condition. There was no significant effect on the path of the COP with only a slight lateralization in the COP curves with the application of LDT. Conclusions: LDT significantly decreased the pressure transmitted through the foot during contact. There was no significant effect on the path of the COP but there was a lateralization in the COP line. LDT may assist with the healing process to prevent chronicity and degeneration from occurring and may be a possible consideration for treatment in the acute stages of PF by unloading the foot. Further study is required examining the therapeutic effects of LDT and possibly comparing it directly to other types of tape.
Keywords: Low dye taping, Foot pressure, Plantar fasciitis
Cite this paper: Paolo Sanzo, Tony Bauer, The Effects of Low Dye Taping on Vertical Foot Pressure in Subjects with Plantar Fasciitis, International Journal of Prevention and Treatment, Vol. 4 No. 1, 2015, pp. 1-7. doi: 10.5923/j.ijpt.20150401.01.
Article Outline
1. Introduction
- Plantar fasciitis (PF) has often been used as a generic term for describing all types of heel pain. The overuse of this term has led to confusion regarding the understanding of this problem. [1] It should be clarified that PF denotes a clinical condition in which the main feature is pain on the plantar aspect of the heel localized to the anteromedial calcaneal tubercle. [1, 2] While reliable epidemiological and incidence rates for PF are lacking, it has been estimated that 80% of patients complaining of foot pain have PF [1, 2] and that 10% of the general population will develop PF at some time in his/her lifetime. [3, 4] In the United States this totals approximately one to two million patients annually [5, 6] accounting for 11-15% of patient visits to healthcare providers. [7, 8] It is also reported that PF is common among obese individuals, military personnel, and runners. [4, 8-11] PF is equally prevalent among the sexes and may occur bilaterally in up to one third of cases. [12, 13]Heel pain has often been a diagnostic and therapeutic challenge to practitioners. It can arise from several anatomical structures including soft tissues, bones, neurological tissues, or referred sources. [8] Alleviation of PF depends upon making an accurate diagnosis and then providing the appropriate treatment. It is important to understand the anatomy and mechanics of the plantar fascia in order to correctly treat the problem.The plantar fascia has several functions in the foot and plays a role in maintaining the medial longitudinal arch and decreasing the force transmitted during weight bearing. [14, 15] In a static stance position the plantar fascia takes up as much as 60% of the stress of weight bearing. [16, 17] The plantar fascia also affects the movements in the subtalar joint during gait. [18, 19] In the presence of excessive subtalar supination or pronation, abnormal force or pressure is transmitted to the plantar fascia. With excessive supination, the calf musculature, Achilles tendon, and plantar fascia are tightened and cannot be extended at heel strike. Ankle dorsiflexion is reduced and the ground reaction forces cannot be adequately absorbed resulting in excessive stretch of the fascia. [20] Conversely, in the presence of excessive pronation, the ligaments supporting the bones of the foot are lax and do not provide adequate support; subsequently, this force is transmitted to the plantar fascia. In this case, ankle dorsiflexion is excessive and the foot is not stable during the stance phase of gait resulting in excessive stretch on the plantar fascia. [20]The treatment of PF ranges from conservative to surgical interventions but the efficacy for the treatment of choice remains elusive. Treatment is often designed to resolve the inflammation, decrease tension and pressure on the fascia and associated structures, and correct any biomechanical abnormalities such as calcaneal or forefoot valgus or varus deformities. [1, 2, 8] Therapeutic taping is one of the conservative treatments commonly used. Taping has been proposed as tier 1 treatment that is supported by fair evidence, consistent with level 3 (retrospective case control), or level 4 (expert opinion) studies. [8] The findings available in the medical literature, however, are variable with conflicting results on the efficacy of use. Despite this, therapeutic taping continues to be used extensively. As a result, the purpose of the present investigation was to measure the effects of low dye taping (LDT) on vertical foot pressure and on the centre of pressure (COP) path during the various phases of gait in subjects with PF.
2. Methods
2.1. Subjects
- Ten participants (six females and four males; mean age 28 years ± 9.24; height 165 cm ± 9.73; and body mass 69 kg ± 3.96) were recruited via purposive sampling. Potential participants were medically screened by their family physician to confirm the diagnosis of PF. Participants were included into the study if they had: 1) heel pain in the morning with the first few steps; 2) heel pain when taking steps after prolonged sitting; 3) pain localized to the anteromedial calcaneal tubercle and/or throughout the plantar fascia; 4) heel pain for less than 1 year; 5) greater than 5 degrees of forefoot varus (overpronated foot) and; 6) no other neurological or vascular foot conditions. Participants were excluded from the study if they: 1) had an acute ankle injury within the past six weeks prior to testing; 2) were allergic to adhesives such as Band Aids, tape, or Tuff Skin and; 3) were receiving any other treatment to the foot at the time of the investigation. All procedures and risks were explained to the subjects, and informed written consent was obtained.All of the testing procedures took place at a foot analysis clinic and laboratory. Testing was conducted during the same time of the day to control for diurnal effects and variation. Ethical approval for completion of the study was obtained from the university research ethics board. Prior to completion of the main study, a pilot study was also conducted to standardize the technique of taping, collection of data, and data analyses by the investigators on a normal healthy cohort.
2.2. Apparatus
- A long arm Baseline® Absolute-Axis™ plastic goniometer was used to complete all of the ankle ROM measures. A Baseline® Electronic Push-Pull Dynamometer (500 lbs capacity) was also used to complete all of the resisted isometric ankle strength measures. These measures were completed as part of the initial screening examination of all potential participants.
2.3. Procedure
- Tracings of the subject's affected foot were taken and the appropriate sized F-scan sensor was trimmed. The sensor was strapped to the plantar aspect of the affected foot using a tight fitting elastic sock to prevent movement between the surface of the foot and the insole. The F-Scan (Teckscan Incorporated) is a computerized insole sensor system that was used to measure plantar pressure and COP. The sensors consisted of a thin insole composed of 960 individual pressure sensors that provided a spatial resolution of four sensors/cm2. The insoles have a semi conductive ink in between the inner surfaces and the electrical resistance change is inversely proportional to the pressure applied to the region. [21] The F-Scan has fair to good reliability reported with intra-class correlation findings ranging from 0.75-0.76 in a diabetic population [22] compared to a Pearson product moment correlation coefficient of 0.93 in a group of normal, healthy subjects. [23] Once the sensors, connection pads, and waist belt was fastened, calibration of the system was performed and subjects were instructed to walk for a few steps to get used to walking with the attached apparatus and to insure that it was firmly attached and accurately recording foot pressure (figure 1).
 | Figure 1. F-scan gait analysis system and pressure insole |
 | Figure 2. Low dye taping technique |
2.4. Data Analysis
- Descriptive statistics were used to compare the mean and standard deviations for vertical foot pressure changes with and without tape. Two independent variables (phase of gait and taping condition) and one dependent variable (vertical foot pressure) were examined. A two-way repeated measures factorial ANOVA with ANOVA F-test was used to detect significant differences between the dependent variable vertical foot pressure measured in pounds per square inch (psi) under two taping conditions, walking with and without tape during the different phases of gait (contact, mid stance, and propulsion). A Bonferroni correction was implemented to keep the error rates at an alpha level of .05. Descriptive analyses were also used for the COP curves to visually describe the effects of tape to no tape on the COP line and whether a medialization or lateralization occurred.
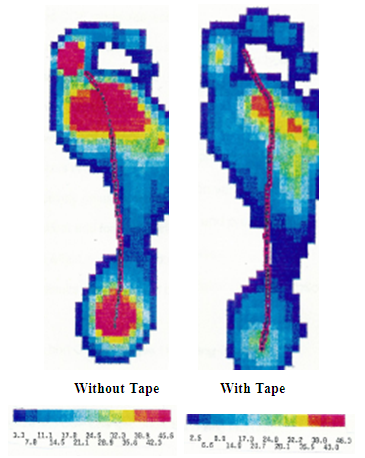
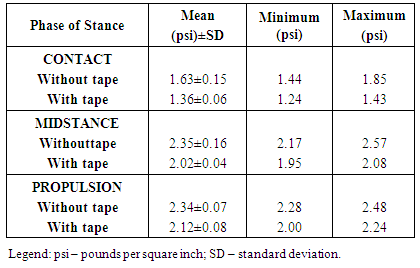
3. Results
- Table 1 presents the mean, standard deviation, minimum, and maximum values for vertical foot pressures during each phase of gait with and without tape. Subjects demonstrated a significant difference for the phase of gait, F(2,54)=321.73, p=.0005 with lower vertical foot pressures found at contact; there was also a significant difference for the taping condition, F(1,54)=105.42, p=.0005 with lower vertical foot pressures found with the application of LDT compared to the no taping condition (figure 3). There was also a slight lateralization in the COP curves with the application of LDT. Lateralization in the COP line occurred at contact and during midstance with tape (figure 4).
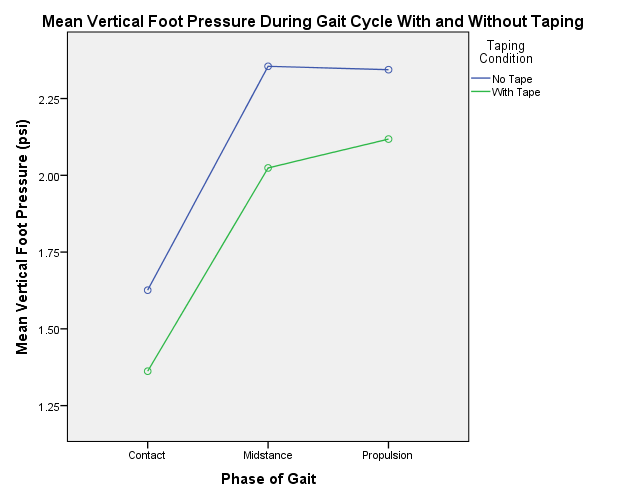 | Figure 3. Mean vertical foot pressure (psi) during the different phases of gait (contact, midstance, propulsion) under two taping conditions (with and without tape) |
|
4. Discussion
- The purpose of this investigation was to measure the effects of LDT on vertical foot pressure and COP in subjects with PF. LDT was effective in significantly decreasing vertical foot pressure under the rearfoot during contact and this is consistent with the findings reported in the literature. The number of studies examining the effects of LDT on foot pressure is limited; however, there is a multitude of studies examining the effects on pain and joint motion.Several authors have all reported that LDT decreased the force under the foot. [21, 25, 26, 31, 32] These authors have also stressed the importance of decreasing the pressure transmitted in the plantar fascia as one of the goals of treating this condition and that LDT is one of the treatments that can be used to achieve this. More recently, Vicenzino et al [25] has reported that taping produced significant increases in lateral midfoot plantar pressures during walking and running and reduced mean maximum pressure in the medial forefoot and rearfoot during walking. The reduction in medial rearfoot pressure is similar to the findings reported in the present study, however, the current study found no significant differences in pressure in the midfoot or forefoot regions.Conversely, Van Lunen et al [26] reported that orthoses and LDT produced similar statistically and clinically significant results for the reduction in pain but no effect on mean and peak plantar pressures while walking or jogging. Seventeen participants were evaluated after 45 seconds of walking and jogging with the use of an orthoses, augmented low dye taping, and with no intervention (control). The use of a modified taping technique that differs from LDT used in the present study may have produced inconclusive findings and making it difficult to compare with the results of the present study.It has been reported that the remodelling of dense connective tissue, such as the plantar fascia, occurs at a slower rate than other more metabolically active tissues such as skin, muscle, and bone. [23] The tensile breaking strength of the plantar fascia has also been reported to be 1.7 to 3.4 times the body weight and forces in the fascia peak at around 800-1000N. [28] The biomechanical events during gait that produce this tensile force include subtalar and mid tarsal joint pronation during first part of the stance phase of gait, soleus and gastrocnemius contraction during terminal stance, and the windlass mechanism during heel off. [14, 29] The use of LDT may assist with reducing some of the force transmitted through the rearfoot and plantar fascia, and prevent overpronation and failure in the tissue from occurring. In the current study, the lateralization evident in the COP line with the application of LDT resulted in supination of the foot thereby reducing the amount of pronation occurring in the foot. This, in turn, may be beneficial in reducing some of the biomechanical stress on the fascia associated with overpronation.The chronicity of PF may be the result of repetitive damage from micro failure of the tissue followed by incomplete repair. When forces exceed the tissue’s tensile strength capability, micro tears often occur resulting in inflammation and subsequent degenerative changes. Recovery from PF may be dependent on the ability of the tissues handling ongoing forces transmitted through this area during weight bearing, walking, and running activities. If weight bearing forces could be controlled to more tissue tolerant levels, then the normal healing process could take place. [27] This further highlights the importance of our findings in that LDT may assist in reducing some of the weight bearing forces and assist with the healing process, preventing chronicity especially if applied early on in the acute phase of healing.In a meta-analysis completed by Cheung et al [30], foot orthoses, motion control footwear and therapeutic taping were able to control rearfoot motion with taping being the most effective intervention. The tape applied increased external tension in the skin, thereby, controlling the amount of motion. It must be highlighted that LDT did not appear to control excessive pronation whereas high dye and stirrups taping did apply the required leverage and support. Several authors have reported similar results with high dye taping reducing maximum rearfoot eversion compared to LDT and no taping. [31, 36] On the other hand, O’Sullivan et al [21] have reported that LDT decreased both pronation and supination in the rearfoot and appeared to reduce general motion in this area. Once again, this highlights the mixed results reported on the effects of tape on foot motion and biomechanics. Our findings also did not find any dramatic changes with the application of LDT. A slight lateralization of the COP line was evident during contact and midstance under the rearfoot and midfoot, but this change was only minimal. The current sample consisted of overpronators as evident by the medial location of the COP line without tape. Excessive pronation has been described as a possible cause of increased tension in the PF and pain. The application of LDT may then result in a reduction of pronation and possibly a reduction in the tension and symptoms associated with PF.Significant research has described mixed results and effects of taping on reducing heel pain and improving function. El Salam and Elhafz [32] have reported that there is no significant difference between the use of LDT and medial arch supports in the reduction of pain and function when measured on a VAS and Foot Pain and Disability questionnaire but reported that medial arch supports were a more convenient option to use. Similarly, a systematic review by Uden et al [4] also supported the use of customized foot orthoses in reducing pain and increasing functional outcomes. Although the present study did not examine the effect on pain specifically, it may help to explain the reason behind some of the positive effects in reducing pain in symptomatic individuals. This information may also be used by the clinician to justify the use of therapeutic taping as a possible treatment intervention. Cheung et al [30] reported that the intervention chosen should be based on patient characteristics, type of activity, and personal preference of the patient and/or clinician. Hunt et al [27] also reported that therapeutic taping should be utilized to promote optimal healing so use in the early stages may be important. The timing of use may then also be a consideration for clinicians. Short term improvement in pain was also reported by Hyland et al [33] who compared the use of stretching of the plantar fascia to calcaneal taping, sham taping, and no taping. Significant improvement in VAS scores were noted with calcaneal taping but no change was reported in patient specific functional scale scores. Similar short term pain management was also reported by Landorf et al [34] and Radford et al [35] when comparing LDT to no taping. Therapeutic taping may be beneficial as a short term form of treatment but not a long term solution due to the possibility of skin breakdown [36] and the fact that the tape will not address other biomechanical causes present.The overall research available remains controversial. In a systematic review examining the taping effects in the treatment of plantar fasciosis, limited results were available supporting the use of taping for short term pain relief and the evidence on effect on disability is inconclusive. [37] Considerations have also been reported on the possible combination of LDT with other interventions. Clinicians often do not treat with a single intervention but rather use clinical reasoning and evidence based practice to treat in a multi-modal manner to optimize healing and treatment results. Research has shown that the combination of LDT with iontophoresis, for example, may produce immediate results and alleviate short term symptoms. This once again supports the efficacy as a short term solution and an adjunct treatment option so that healing is maximized. [36]A limitation to this study was the small sample size and lack of a true control group. Another limitation was the fact that the gait pattern may have been altered due to the tape, cords or sensors in the shoe. Future investigations should include a control group to assess the effect of LDT and also compare different types of tape and the effect on pain, range of motion, function, and pressure over a longer term follow up period.
5. Conclusions
- The findings of the current study found that LDT was effective in significantly decreasing vertical foot pressure under the rearfoot during the contact phase of gait. We can conclude that LDT may be effectively used in patients suffering from PF to decrease vertical foot pressure. LDT may also be an effective treatment in decreasing pressure in other foot injuries but further study is required to assess this generalization. LDT may also assist with the healing process to prevent chronicity and degeneration from occurring and may be a possible consideration for treatment in the acute stages of this disorder.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML