-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2013; 2(3): 38-40
doi:10.5923/j.ijpt.20130203.03
Brittle Asthma; A Case Report
Raja Ahsan Aftab1, Amer Hayat Khan1, Irfhan Ali2, Syed Azhar Syed Sulaiman1, Nafees Ahmed1
1Department of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, 11800, Malaysia
2Department of Respiratory Medicine, Penang General Hospital, Penang, Malaysia
Correspondence to: Amer Hayat Khan, Department of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, 11800, Malaysia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Introduction: Asthma is a varied disease, while brittle asthma is identified as its distinct phenotype. Terms brittle asthma described for asthmatic patients whose peak expiratory flow (PEF) was chaotic. Brittle asthma is characterized by wide variation in PEF despite treating with high doses of inhaled steroids. Broadly, two types of brittle asthma have been classified. Type 1 brittle asthma is characterized by more than 40% variation in PEF. Type 2 brittle asthma is characterized by severe acute attacks and could lead to death or mechanical ventilation for respiratory insufficiency. Case representation: A 13 year old Malay boy was admitted to hospital, complaining shortness of breath and chest tightness. The patient was recently hospitalized for uncontrolled asthma. The case represents brittle asthma with recurrent bronchospasm, severe acute exacerbation of bronchial asthma secondary with hospital acquired pneumonia. Conclusion: The patient was treated with multiple drug therapy. One week after the initiation of treatment patient feels better and is discharged. Parents are advised to prevent allergen exposure.
Keywords: Brittle Asthma, Peak Expiratory Flow (PEF), Respiratory Insufficiency
Cite this paper: Raja Ahsan Aftab, Amer Hayat Khan, Irfhan Ali, Syed Azhar Syed Sulaiman, Nafees Ahmed, Brittle Asthma; A Case Report, International Journal of Prevention and Treatment, Vol. 2 No. 3, 2013, pp. 38-40. doi: 10.5923/j.ijpt.20130203.03.
1. Introduction
- Asthma is a heterogeneous disease. Brittle asthma is identified by its distinct phenotype[1] and merely accounts for 0.05% of asthmatic population[2]. It is characterized by vide variability of peak expiratory flow (PEF) despite taking high dose of corticosteroids. Patients with variation of PEF are on increased risk of mortality for which, exact mortality of brittle asthma is not known, however[3,4]. Depending upon peak expiratory flow rate, it is sub classified into two types namely type 1 and type 2 .Diagnosis of brittle asthma involves PEF monitoring and assessment for the factors responsible for poor control of asthma. Majority (60%) of patients with type 1 brittle asthma are food intolerant. Double blind placebo controlled trials confirms that over 50% of these patients are intolerant to wheat and dairy products[5]. Moreover, psychosocial morbidity, poor quality of life and asthma related events are a commonly associated with brittle asthmatic patients[6,7]. Immunoglobulin deficiency, autonomic imbalance and relative resistance to anti inflammatory action of steroids are also considered to be the associated factors[8].Identifying and avoiding the allergen exposure is critical in the management and treatment of brittle asthma. Long term subcutaneous infusion of β2 agonist has showed improvement in symptoms and variation of PEF in 50% patients[9]. Effectiveness of alternative immunomodulatory treatment in steroid resistant brittle asthmatic patients is not yet certain.
2. Case Presentation
- A 13 years old Malay boy with history of bronchial asthma was admitted to hospital. The patient complained of shortness of breath and chest tightness and had a recent history of hospitalization because of uncontrolled asthma. Patient was a student and did not consume cigarette or alcohol. Patient was not known to have any drug allergy and did not have family medical history.On Physical examination the patient was alert, conscious, tachypnic and anxious. The blood pressure was raised with a respiratory rate of 30bpm. Cardiovascular function was recorded to be normal with no murmurs at atrioventricular (AV) or semilunar (SV) valves. Lung examination showed generalized rhonchi, prolong expiratory phase, good equal breath sound and generalized coarse crepitation. White blood count was higher (15.36 x 103/µL) indicating infection and suspicion was made over Hospital acquired pneumonia. Serum potassium level (3.4 mmol/L) was found lower than the normal range. Respiratory infections often being predisposing factors for acute asthmatic episode, the patient was in this case was hence, treated aggressively. The patient was initially provided acute treatment and was then admitted.
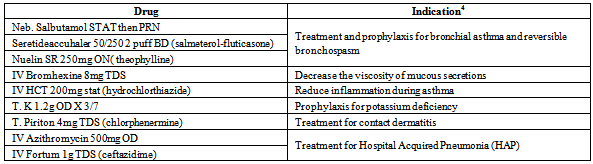
|
3. Discussion
- The therapeutic goals for the patient is to reduce asthmatic attack , prevent recurrent episode, identify and avoid precipitating factors , educating patient regarding medication and increasing patient’s adherence to his medications. Finally improving patient’s quality of life by maximizing the therapeutic response and minimize the side effects of drug therapy. The case study represents uncontrolled brittle asthma, drug interactions and predisposing factors as respiratory tract infection that could lead to asthma morbidity in children. The incidence of drug interactions can be 20% for patients taking 10 to 20 medications[10]. It is critical for doctors to assess the prescriptions before patients are discharged. Salmeterol-theophylline interaction leads to increased blood pressure and tachycardia[4], increased blood pressure in current case may well be due to Salmeterol-Theophylline interaction. However appropriate interval between the dosing of the drugs can reduce the risk of interaction. Role of pharmacist in facilitating doctors in identifying drug interactions and providing they alternate solution cannot be over emphasized. The patient had severe bronchospasm after eating chicken, oranges and grapes. Educating patient mother in avoiding such food is strongly recommended. Since 90% of brittle asthmatics are atopic, avoiding home allergens including pets cigarette smoke can be effective in managing the patient[5].Respiratory tract infections are important triggers for asthma exacerbations in adults and children[11, 12]. Between 14% to 45 % acute exacerbation of asthma are thought to be associated with respiratory tract infection in children[13, 14]. Patients with hospital acquired pneumonia may remain totally asymptomatic[15]. The patient recent hospital admission and increased WBC count, doctor suggest hospital acquired pneumonia as per patient record. Chronic respiratory tract infection may well be the most likely reason behind the patient recent asthma exacerbation. Early diagnosis and aggressively treating respiratory tract infection can reduce risk of asthma exacerbationDiagnosing the patient with brittle asthma involves careful exclusion of possible factors responsible for poor asthma control including PEF, since patients with brittle asthma have chaotic PEF. Compliance with daily self assessment PEF can give an indication of asthma control to patients and can help doctors in managing their patients. Educating and assessing the patient’s inhaler technique can be therapeutically beneficial.
4. Conclusions
- Respiratory tract infection can lead to asthma exacerbation in children. Educating patient and constant supervision can reduce acute attacks and improve patient’s quality of life. PEF should be monitored regularly; this could help the doctor to assess the patient situation better. Patient counseling about potential side effects of the medication and motivating the patient to take medications as directed is recommended. Helping assess the patient own condition could reduce recurrent asthma attacks.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML