-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2013; 2(2): 19-22
doi:10.5923/j.ijpt.20130202.02
Traumatic Trapeziometacarpal Dislocation: Two Case Reports and Literature Review
Pedro José Labronici1, Bruno de Araújo Silva1, Gustavo José Labronici1, Leonardo de Andrade Moreira2, Robinson Esteves Santos Pires3
1Orthopaedic and Traumatology Department / Santa Teresa Hospital. Petrópolis (RJ), 25685-040, Brazil
2Orthopaedic and Traumatology Department / Felício Rocho Hospital. Belo Horizonte (MG), 30110-060, Brazil
3Orthopaedic and Traumatology Department / Federal University of Minas Gerais and Felício Rocho Hospital. Belo Horizonte (MG), 30110-060, Brazil
Correspondence to: Robinson Esteves Santos Pires, Orthopaedic and Traumatology Department / Federal University of Minas Gerais and Felício Rocho Hospital. Belo Horizonte (MG), 30110-060, Brazil.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Trapeziometacarpal dislocation generally occurs due to trauma. Various treatment methods have been applied, including conservative and surgical options, however no gold standard approach exists for this rare injury. This study aims to report treatment outcomes of two traumatic trapeziometacarpal (TM) dislocation cases, including one patient who evolved with excellent functional outcome despite conservative treatment. A literature review of this uncommon hand injury is performed.
Keywords: Trapeziometacarpal Joint, Dislocation, Thumb, Surgery
Cite this paper: Pedro José Labronici, Bruno de Araújo Silva, Gustavo José Labronici, Leonardo de Andrade Moreira, Robinson Esteves Santos Pires, Traumatic Trapeziometacarpal Dislocation: Two Case Reports and Literature Review, International Journal of Prevention and Treatment, Vol. 2 No. 2, 2013, pp. 19-22. doi: 10.5923/j.ijpt.20130202.02.
Article Outline
1. Introduction
- Trapeziometacarpal dislocation is a rare hand injury1,2. Epidemiologically, it accounts for less than 1% of all hand traumas3. The lesion is usually due to an axial force transmitted through partially flexed thumb, forcing the joint to deflect toward dorsal 2,4. Due to volar part of the ligament being thicker and stronger, dislocation occurs in dorsal direction1,2.Optimal treatment strategy for traumatic TM dislocation remains under discussion. Closed reduction and cast, open or closed reduction with temporary K-wire fixation, and dorsal capsule and ligament reconstruction have been used to stabilize the joint2.5. Few cases have been reported however, and a protocol has yet to be developed6.This study aims to report the outcomes of two traumatic trapeziometacarpal dislocation cases and perform a literature review.
2. Case Reports
2.1. Patient 1
- A 29 year old man, right-handed, was victim of a bicycle accident. Left hand examination in the emergency room showed deformity and swelling at the dorsolateral region,evaluating with pain and functional thumb disability. Anteroposterior and oblique radiographs showed dorsal TM joint dislocation . (Figures 1A and 1B)
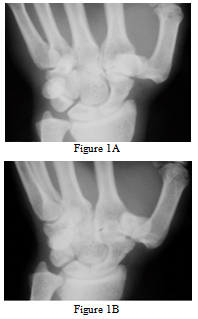 | Figures 1. 1A and 1B - Anteroposterior and oblique hand X-Ray views showing dorsal trapeziometacarpal dislocation |
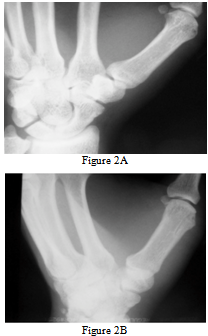 | Figure 2. 2A and 2B – Anteroposterior and oblique hand X-Ray views showing the TM joint 9 months after injury |
2.2. Patient 2
- A 49 year old man was involved in a motorcycle accident. Right hand examination showed pain and thumb functional disability. Anteroposterior X-Ray showed trapeziometacarpal dislocation (Figure 3). After lidocaine injection, reduction was performed, but the joint remained unstable. The patient was scheduled for closed reduction and K-wire percutaneous fixation (Figure 4). After 6 weeks, K-wires were removed, and the patient started physical therapy (Figure 5). Despite partial reduction loss shown 1 month after K-wire removal, normal function was reestablished, and the patient was pain free after 6 month follow-up (Figure 6).
 | Figure 3. X-Ray in AP hand view showing TM dislocation |
 | Figure 4. X-Ray in AP view showing percutaneous TM fixation (K-wires) |
 | Figure 5. 6 weeks after K-wire fixation |
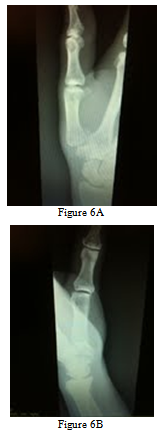 | Figure 6. 6A and 6B and: X-Ray in AP and lateral views. Observe partial TM reduction loss |
3. Discussion
- Traumatic TM dislocation is associated with varying degrees of ligaments and capsule injuries. Anterior oblique ligament is a short and strong structure. For many years, it was considered the key stabilizer to prevent dorsal joint dislocation1. Bettinger et al7 reported that anterior oblique, radial, and ulnar collateral ligaments should be considered the main dynamic thumb stabilizers. Harvey8 and Pagalidis9 proposed oblique posterior and intermetacarpal ligaments as contributing to joint stability. However in a cadaveric study, Strauch et al10 demonstrated that the dorsoradial ligament complex was the limiter of dorsal dislocation and responsible for obtaining joint stability. These findings were clinically confirmed by Shah et al4, who observed no ligaments or volar capsule injuries in four TM dislocation cases. Fotiadis et al 11 found the capsulo-ligamentar complex completely injured while the volar ligament was preserved.Bosmans et al1 showed promising results in two patients with isolated TM dislocation after closed reduction and plaster. Khan et al12 found satisfactory results in a patient with bilateral TM dislocation treated by closed reduction and plaster. Kural et al13 also found similar results after closed reduction and plaster in a TM dislocation patient. Like the other authors, a satisfactory outcome was obtained by applying closed reduction, cast, and physical therapy after a 9 month follow-up in the first patient. When using closed reduction, percutaneous K-wire fixation necessity remains controversial. Watt et al14 showed positive results in 12 patients treated by cast or K-wire fixation. One third of cast patients and two-thirds of K-wire patients had instability and dorsal joint subluxation. Discomfort and hand weakness was reported by all unstable joint patients. Despite partial reduction loss after K-wire removal, patient two evaluated with total functional recovery and pain free. Due to instability degree, K-wire removal was performed after six weeks. However, the literature recommends K-wire removal after four weeks for avoiding limitation of function. Jacobsen et al6 showed a closed reduction and percutaneous K-wire fixation case that evolved with slight instability and radial subluxation.Simonian et al15 compared early ligament reconstruction with closed reduction and K-wire fixation. Ligament reconstruction group presented better outcomes, with normal range of motion, absence of pain, and full apprehension force. Chen2 reported good results after dorsal ligament reconstruction. Shah et al4 advocated that open reduction and fixation with Kirschner wires without ligament reconstruction would be inappropriate for this injury pattern.Determining the appropriate treatment, especially rare, poorly reported injuries remains challenging. Several authors suggest conservative treatment with closed reduction and plaster when joint stability is achieved1,12,13. Other authors report that ligament reconstruction should be avoided in cases of acute injury. However, it seems that open or closed reduction plus K-wire percutaneous fixation may not always guarantee a good outcome2,4,6,14,15.The present study contains several limitations. Small sample size lacked sufficient power to determine the best treatment option. Despite good outcome after partial joint reduction loss, several authors reported discomfort and weakness with the same injury pattern.As strengths, the study reports two rare hand injury cases. As also described in the literature, the authors emphasize that, if the joint stability is achieved after reduction, plaster cast immobilization and physical therapy can produce good outcomes.
4. Conclusions
- Despite partial reduction loss in the patient who underwent surgery, good outcomes were achieved in both cases. More studies with higher evidence level are necessary to determine the gold standard treatment for this uncommon injury.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML