-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Prevention and Treatment
p-ISSN: 2167-728X e-ISSN: 2167-7298
2012; 1(3): 44-48
doi: 10.5923/j.ijpt.20120103.02
Combining Multiple Prevention Strategies in one Health Questionnaire: A Pilot Study
Stefan Morreel 1, Werner Van Peer 1, Veronique Verhoeven 2
1Praktijkhuis de Heuvel, Boechout, Belgium
2University of Antwerp department of primary and interdisciplinary care
Correspondence to: Stefan Morreel , Praktijkhuis de Heuvel, Boechout, Belgium.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
General practitioners are confronted with many required preventive interventions. A solution to this problem is combining several interventions in one questionnaire. Almost no research exists on this subject. In this pilot feasibility study we examine whether a prevention strategy based on a questionnaire increases the number of preventive items in the patient’s records, and we examine the response rate when this questionnaire is given to patients during a routine consultation.An evidence based questionnaire containing 22 questions concerning 11 topics was used in a practice of general practitioners in a semi-rural community. 26 items were studied: the answers to the 22 aforementioned questions plus four more items relating to multiple questions. All were rated before and after the intervention using strict criteria.Of the 104 included patients 46 participated.After the intervention the availability of most items increased but it was only significant for eight items. This unique pilot study clearly shows us that a questionnaire which combines multiple prevention interventions improves the quality of our records. Handing over this questionnaire to patients during routine visits gives a high response rate.
Keywords: Primary Health Care, Preventive Medicine, Preventive Health Services, Quality Improvement, Public Health
Cite this paper: Stefan Morreel , Werner Van Peer , Veronique Verhoeven , "Combining Multiple Prevention Strategies in one Health Questionnaire: A Pilot Study", International Journal of Prevention and Treatment, Vol. 1 No. 3, 2012, pp. 44-48. doi: 10.5923/j.ijpt.20120103.02.
Article Outline
1. Introduction
- General practitioners[GPs] are confronted with an overwhelming amount of required preventive interventions. Due to various barriers both the physician and the patient quickly lose focus[1].The U.S. Preventive Services Task Force for example recommends 45 different preventive interventions[2].In the Flemish guidelines for primary care 500 pages can be found concerning prevention.As it is not possible to use a different implementation strategy for each preventive intervention it might be interesting to implement several interventions at once.With this amount of recommendations it is very hard for a GP to apply all this evidence to one patient. Therefore a more structured way of performing preventive consultations is needed.A possible solution is combining some of theseinterventions in one questionnaire[3]. The Flemish scientific board of general practitioners[DomusMedica] has made such a questionnaire called the health guide[‘de gezondheidsgids’ in Dutch][4].There is a lot of research on single focus preventive interventions[5] but almost no research can be found on combining multiple interventions[2][6].The main objective of this pilot study is to examine whether the use of this questionnaire increases the number of preventive items in the electronic records of the participants. As a secondary objective we assessed how many patients would respond if this questionnaire werepresented during a routine visit.
2. Methods
2.1. The Practice
- This pilot implementation study was conducted at a practice near Antwerp, Belgium. This practice, located in a semi-rural area consists of four GPs of different ages. The ®Windoc 8.8 electronic records system is used. It containsdatasets such as history, current diseases, follow up notes, current medication, physical measurements and a personal calendar. In this calendar curative and preventive interventions for the future are written down. The International Catalogue of Primary Care[ICPC] is used when applicable[7]
2.2. Population
- The study was conducted between 4/1/2011 and 7/15/2011. Every day the first consulting patient meeting the inclusion criteria was asked to participate. These criteria were: aged between 50 and 65 years and being enlistedat our practice. If the GP forgot to include the first patient he was allowed to include the second one. The participants were given time until 10/15/2011 to return for the intervention. A patient could only be included once. In general there were no exclusion criteria. Only exceptionally the GPs were allowed to exclude a patient for a specific reason. For example,a short life expectancy.
2.3. Questionnaire
- The questionnaire was created in 2010 by the Flemish scientific board of general practitioners (DomusMedica). It contains 25 questions about 11 topics: cardiovascular prevention, smoking, diet, physical exercise, diabetes screening, vaccinations (tetanus, flu, pneumococcal), breast cancer screening, cervical cancer screening, colorectal cancer screening, alcohol abuse and medication abuse. All these topics were chosen out of existing evidence based guidelines and respond to the Wilson andJungner criteria for screening[8] Out of the 25 questions we skipped the questions on physical exercise, diet and medication abuse because of the lack of evidence-based criteria to measure them and because the result of these interventions cannot directly be found in the electronic records. All the remaining 22 questions have dichotomous answers (yes or no) except for age, length and height. For performing a health check with this questionnaire the Belgian government pays the GP a fee of €10, 15 per patient.
2.4. The Intervention
- After the patients were given the questionnaire they were asked to book a new visit for the sole purpose of reviewing this questionnaire. During this visit the GP assessed all 22 questions together with the patient. When needed the GP did some minor physical examinations. For each positive answer one or more actions needed to be performed. For example if the patients states to have a family history of cardiovascular disease then this had to be written down in the family history of this patient’s electronic record. So every question has a corresponding item in the records. In this way the current diseases, history, calendar and measurements were updated. When a small intervention (e.g. vaccination) was needed it was performed at once. More time-consuminginterventions (e.g. PAP-smear) were planned during a follow-up visit. This intervention was approved by the ethical review committee of the university of Antwerp under number A11-24 in May 2012. All patients signed an informed consent
2.5. Pre-intervention Measurement
- We did not measure the availability of the answers to the 22 questions but the availability of the corresponding 22 items in the records. We measured four more items which had to be planned if the answer to one or more questions was positive(these items relate to more than one question). In total 26 items were assessed.All the items were rated as available or not available. Not available does not mean false. When for example a patients scored non available for the item ‘Hypertension’ this means that in his current disease list he did not have this item, either because the GP knew the patient doesn’t suffer from hypertension either because the GP isn’t aware of it or forgot to write it down. Criteria were formulated to assess the availability of all the 26 items. E.g. for the item ‘Weight’ this means having had a weight measurement during the past year. In general these criteria can be divided into five types:-Eight items which had to be planned in the personal calendar. E.g. for breast cancer screening a future mammography had to be found in this calendar. -Four items that had to be added to the current diseases list.-Five items were measurements and the exact numbers had to be written down. Eight items were registered as risk factors (e.g. smoking and family history). One item had to be registered in the history (previous cardiovascular event).Medication for hypertension had to be registered in the current medication list.For some patients it was not possible to review their record before the intervention because they returned to soon. They were regarded as missing values.
2.6. Post-intervention measurement
- For the participating patients all 26 items were rated again after the intervention using the same criteria.
3. Statistics
- Descriptive statistics about the included population were conducted with SPSS version 20. We assessed the differences between the participating and thenon-participating population with univariate statistics. Age was the only continuous variable for which we used the unpaired T-test. All the other variables were dichotomous and assessed through the chi square analysis or the Fisher exact test. No sample size calculation was done for the intervention, since the required number of participants would be different for each variable in the questionnaire and since no reliable estimate of effect size could be made due to lack of examples in the literature. Therefore, the results of this pilot study must be interpreted qualitatively rather than quantitatively.
4. Results
4.1. Population
- The flow of patients through the study is shown in figure 1. We offered the questionnaire to 108 patients. In total four patients returned too quickly to do the pre-intervention measurement. No log files were available to rectify this. The mean age was 57,5 years. All patients were included between 4/1/2011 and 7/13/2011. GP one included 25 patients of whom 13 participated (52%). GP two included 44 patients of whom 24 participated(55%). GP three included 13 patients of whom two participated(15%). GP four included 22 patients of whom seven participated(52%). In Total 46 patients participated. The fastest one participated the same day of the inclusion, the slowest one 102 days after inclusion.
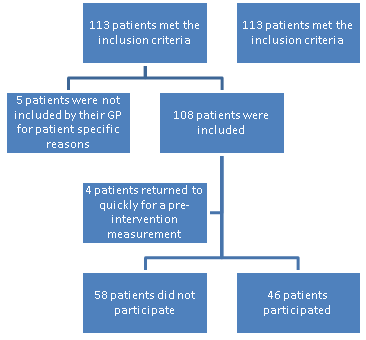 | Figure 1. Flow chart of the study population |
4.2. Pre-intervention Measurement
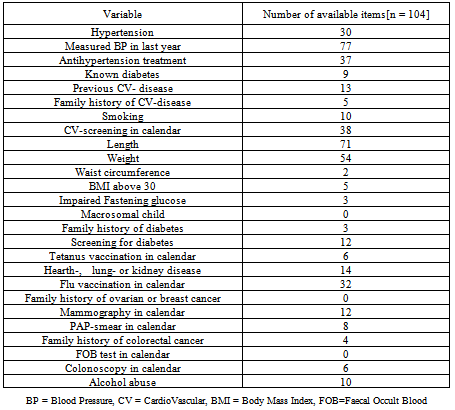
- The results of the pre-intervention measurement can be found in table 1.
4.3. Differences Between the Participating and the Non-participating Patients.
- The participating and the non-participating patients were similar for the variables we studied. We only mention the significant differences. The participants were three years older on average. A length measurement could be found for 80% of the participants and only for 59% of the non-participants. A flu vaccination was planned for 46% of the participants tors and only for 19% of the non-participants tors. Finally a mammography was planned for 36% of the participating patients and only for 10% of the non-participators.
4.4. Post intervention measurement
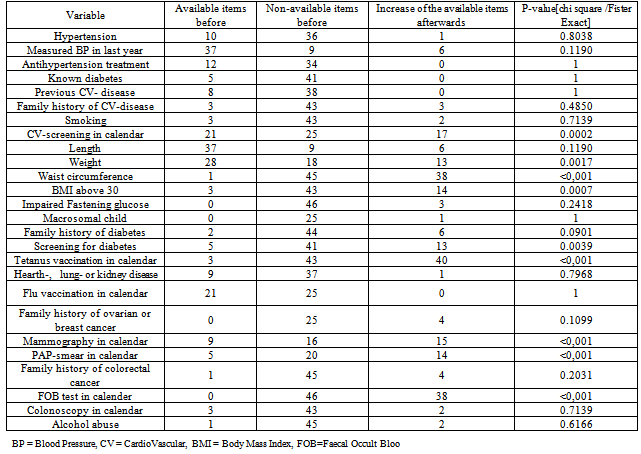
- The results of the Post intervention measurement can be found in table 2.There was an increase for most items but it was only significant for planned cardiovascular screening, weight, waist circumference, BMI above 30, planned screening for diabetes, planned tetanus vaccination, planned mammography, planned PAP-smear and planned FOB test.
|
|
5. Discussion
- In this study we tried to find a solution to the overwhelming amount of preventive interventions in general practice. This study shows that a combined prevention strategy, opportunistically offered by a GP, is successful in terms of preventive measures taken and in terms of response rate. Of the included patients 46% came back for the preventive visit. This is more than in a similar Dutch study where a written invitation yielded a response of 33% and a poster invitation only one percent[9] A small unpublished Belgian trial with the same recruitment strategy as ours had a response of 26%[10] Three out of four GPs had a response rate of about 50%, one had a much lower response of 15%, we do not have a solid explanation for this. The two younger GPs included fewer patients, probably due to a different population with less patients aged between 50 and 65. In the pre-intervention measurement we found reasonable rates for cardiovascular prevention, weight and length measurements, breast cancer screening and alcohol abuse. The rates for tetanus vaccination, diabetes screening, cervical cancer screening and family history of some diseases were rather low. For three items the rates in the participating population were better than the rates in the non-participating population. This might indicate a healthy volunteer bias.[11]After the intervention we saw an increase for 22 out the 26 items. Due to the small number of included patients this increase was only statistically significant for nine items. As expected for those items found to be weak in the pre-intervention measurement analysis we saw a marked increase. Screening for colorectal cancer was a new project for this practice, of the 46 participating patients 40[87%] had either a faecal occult blood test or a colonoscopy planned. In a similar but randomized Canadian trial 51% of the participants had a FOB after the intervention[2] In a large Belgian trial for colorectal cancer screening with postal invitation the response rate was 44,3%.[12]For some items the frequency was too low to assess them in this study(e.g. macrosomic child). This project slightly increased the workload of the practice. Once acquainted to the use of this questionnaire the visits took about 15 minutes. Since the participating patients now have much better records, this project might even lessen the workload in the future. Most patients were enthusiastic about this project, some were not interested. We did not receive any negative reactions.This pilot study has a number of limitations. The questionnaire was based on evidence based and validated guidelines but is not validated itself[13] We also had to remove some of the questions because of the limitations of our electronic records. This was a non-controlled and non-randomized study: part of the increase in preventive actions might be due to a general improvement of our preventive attitudes. However a similar randomised trial did not show improvement in the control group[2] The outcome of this combined intervention in terms of health improvement has not been studied. The fact that GPs were allowed to include only one patient a day might have influenced the results. Due to the small sample size differences between the participating GPs cannot be examined. Finally this was an opportunistic screening strategy. Possibly those patients with the worst preventive status do not frequently attend general practice[14, 15]Due to the above mentioned issues conclusions about the efficacy or efficiency of this questionnaire cannot be drawn.These weaknesses should be addressed in upcoming research. The results of our study are promising, but to generalize these findings there is need for a multi-practice study in a large randomized trial.
6. Conclusions
- There is a large amount of required preventive interventions in general practice. It is not possible to develop an implementation strategy for all these individual interventions in one single practice. A strategy for combining some of these interventions and implementing them at once is needed. As a solution we tested a questionnaire concerning 11 topics and containing 25 questions. This unique study clearly shows us that using this questionnaire is feasible and improves the quality of our records. Presenting this questionnaire during routine visits gives a high response rate. We believe this leads to better and more systematic prevention. Further research on the efficacy and efficiency of this questionnaire is needed.
ACKNOWLEDGEMENTS
- No conflict of interest, no financial resources
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML