-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Psychology and Behavioral Sciences
p-ISSN: 2163-1948 e-ISSN: 2163-1956
2020; 10(1): 9-16
doi:10.5923/j.ijpbs.20201001.02

Minimising Stress Exposure During Pandemics Similar to COVID-19
Mohamed Buheji1, Haitham Jahrami2, Ali Sabah Dhahi3
1Founders of the International Inspiration Economy Project, Bahrain
2Ministry of Health Bahrain, College of Medicine and Medical Sciences, Arabian Gulf University, Bahrain
3Ministry of Health, Bahrain
Correspondence to: Mohamed Buheji, Founders of the International Inspiration Economy Project, Bahrain.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The misinterpretation of the COVID-19 pandemic has the potential for creating devastating stress that might turn into anxiety and other psychological diseases. The social isolation, quarantine, and lockdown can increase stress responses and generate more status of uncertainty. The body of knowledge has a significant gap in relevant to practising resilient practices such as visualising a ‘stress mitigation strategy’ during a long-term pandemic. Based on the synthesis of the literature, a framework for compensating stress during and after pandemics is proposed. The researchers discuss the importance of such a framework as a pressure relief valve in the accumulated ‘pandemic stress exposure’. The proposed framework can be used for future outbreaks once more research empirically tests it and optimise its constraints.
Keywords: COVID-19, Coronavirus, Stress Response, Stress Exposure, Social Isolation and Quarantine, Resilient Communities, Uncertainty, Emergency Psychological Interventions
Cite this paper: Mohamed Buheji, Haitham Jahrami, Ali Sabah Dhahi, Minimising Stress Exposure During Pandemics Similar to COVID-19, International Journal of Psychology and Behavioral Sciences, Vol. 10 No. 1, 2020, pp. 9-16. doi: 10.5923/j.ijpbs.20201001.02.
Article Outline
1. Introduction
- The Novel Coronavirus 2019 (COVID-19), which is known as a severe acute respiratory syndrome Coronavirus 2 has gained intense attention worldwide. This is attributed to the infectious nature of the disease, fast transmission pattern and inadequate preparedness of health authorities to address such an outbreak. The COVID-19 that has been first identified in Wuhan, Hubei Province, China in December 2019 which soon World Health Organization (WHO) declared it as a global pandemic with an international public emergency that poses a threat on public health both physically and psychologically. WHO (2020).COVID-19 has become a stressor as it has affected people's lives in different aspects, and since there is no vaccine against it as yet. Previous studies on the physical and psychological effects of earlier outbreaks of serious infectious diseases, such as SARS, showed increased stress, anxiety, depression and post-traumatic stress among survivors, Wu et al. (2005). The widespread social isolation, quarantine and in certain countries the strict and long curfew measures, in an attempt to contain the global pandemic, could also lead to a high level of psychological distress, Hawryluck et al. (2004). This review attempts to explain the key elements that increase stress responses associated with the COVID-19 outbreak among the public and some action measures to be taken to alleviate it and manage it effectively.The authors review first the COVID-19 pandemic as a crisis that created a psychological polarisation that extends between hope and despair. Stress and ‘stress responses’ are first defined and identified, followed by the challenges brought with the COVID-19 as a pandemic with many uncertainties. Then, the researcher explores the possibilities for eliminating a global anxiety pandemic by mitigating the stress and the physiological pressures that the COVID-19 pandemic is creating. Here ‘emergency psychological interventions’ are presented. The paper goes further to illustrate the factors of stress response during such outbreaks and managing the pandemic exposure influence, taking media as a sample of ‘stress exposure’. Finally, the review ends with the importance of stress mitigation visualisation strategies which lead to the construction of a Stress compensator framework during pandemics as COVID-19.
2. Literature Review
2.1. COVID-19 Pandemic – Between Hope and Despair
- Since its inception and outbreak, December 2019, COVID-19 pandemic became a mental contagion that is causing panic, anxiety, depression and most of all, stress. Every day passes people live between the hope of getting the solution to their health and socio-economic challenges that this virus has managed to disrupt, and feelings of despair where no clarity of when this crisis would end. The consequences of this daily stretching between hope and despair, brings out the worst in us, as mentioned by Okr (2020). However, once we start to realise and accept the scale of the problem and control our negative imagination that leads to fear, we would begin to clear opportunities inside this global challenge. This is what (Daley, 2020) meant by appreciating the scale of our challenges so that it alters the scale of our visionary response.Managing COVID-19 is more than hand washing and social distancing; instead, it is a story between hope and despair. Within this story, we need to manage the stress that comes as a result of being extreme on one end on behalf of the other. This exaggeration as Robinson (2020) sees it is what creates for us fear, which makes us know what happening around us of being of drastic changes that we cannot expect, and we are not competent to face this amount of uncertainty. Living with this uncertainty without using the end of the tunnel creates tremendous levels of stress and then might lead to diseases, out of which anxiety is first.
2.2. Definition of Stress and Stress Responses
- Despite the absence of common definition and conceptualization of stress, that has changed over time; there is consensus that stress is an inherent part of life that is associated with several individually vital physiological, psychological and behavioural symptoms, Monroe and Slavich (2016), Schuler (1980). Stress brings with it different emotional and physical disorders, like depression, anxiety, heart attacks, strokes, gastrointestinal distress, obesity, and hypertension. The higher is this stress the most it can create more symptoms. Frequent headaches sleep disturbance, back and/or neck pain, dizziness, persistent illness, irritability, gastrointestinal problems, excessive worry, muscle tensions, feeling of being overwhelmed, and having difficulty quieting the mind; are just a few examples of stress symptoms. Hence, with such stress responses, many people during a pandemic or crisis like COVD-19 would experience poor concentration, forgetfulness, and low energy. Knowing these stress responses can help in manifesting the build-up of such stress and to know when to use stress reduction techniques that would minimize long-term repercussions, Hurely (2019).Based on Claude Bernard & Charles Darwin's statement that organisms must adapt to ever-changing environmental circumstances to survive, specific definitions for conceptualizing stress emerged. Therefore, stress can be defined as a state of disharmony and is neutralized by a complicated variety of physiologic and behavioural responses that aim to maintain/re-establish the threatened homeostasis (adaptive stress response), Perturbing (1992), Lazarus and Folkman (1984). Based on this definition, stress arises when a person perceives the demands of environmental stimuli to be higher than their ability to meet, mitigate, or alter those demands.
2.3. Identifying ‘Stress Responses’ During COVID-19
- People’s ability to effectively respond to stressors varies considerably. It should be acknowledged that maladaptive stress responses can sometimes be inadequate, or excessive and/or of prolonged reactions which may lead to disease. Moreover, highly potent and/or chronic stressors can have negative effects on a variety of physiologic functions, including metabolism, growth, reproduction, and immune-competence, as well as on behaviour and personality development, Monroe and Slavich (2016). Prenatal life, infancy, childhood, and adolescence represent critical periods in the process of forming the matrix of the adaptive stress response. These periods are characterized by the high plasticity of the stress system and increased vulnerability to stressors.Similar to a previous threatening event heightened stress responses during the COVID-19 ongoing outbreak could be associated with adverse physical and mental health outcomes over time. Some of the stress symptoms that can be experienced during this pandemic include:• Fear and worry about your health and the health of your loved ones• Changes in sleeping or eating patterns• The difficulty of sleeping or concentrating• Worsening of chronic health problems• Increase the use of alcohol, tobacco, or other drugsSuch stress symptoms can be overwhelming, not affecting people at a personal level but rather lead to stress responses. Such an increase in stress responses leads to a disproportionate rise in help-seeking behaviours vs the actual threat, thereby placing the unneeded burden on authorities and diverting the attention of essential resources in times of severe pandemic. For instance, the panic hydrophobic purchasing and storing of infection prevention items as the protective masks, gloves, soap and hand sanitizers have led to global shortages of these necessities. This panic extended even to unjustified crazy demand for toilet papers. Garfin et al. (2020).
2.4. Experience of Stress Responses during Past Outbreaks
- Lee et al. (2007) shown that there are a high-stress level and psychological distress of severe acute respiratory syndrome (SARS) survivors, one year after the outbreak; in comparison with control subjects. The Lee research team even showed that this stress stayed high without signs of decrease. The SARS 2004 survivors showed alarming levels of stress-related psychiatric distress. Therefore, long-term psychological implications of infectious diseases should not be ignored. Lee et al. (2007).Brooks et al. (2020) shown the psychological impact of quarantine, based on 3166 papers reviewed, showed adverse psychological effects, including post-traumatic stress symptoms, confusion, and anger. The Brooks team has demonstrated that the stressors factors came from longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma during the pandemics. The studies included epidemics as SARS, Ebola, H1N1 influenza, Middle East respiratory syndrome (MERS), and equine influenza. The separation and restriction of movement, uncertainty over disease status, besides the fear of being exposed to a contagious disease increase the strength of the stress. Brooks et al. (2020) emphasised for weighing the benefits of mandatory mass quarantine against the possible psychological costs carefully.
2.5. The Challenge of the COVID-19 Pandemic Uncertainties
- WHO (2020) warned that governments, public health, and community leaders should refrain from creating a stigma around people infected or treated for COVID-19 by labelling them as “COVID-19 cases”, “victims” “COVID-19 families” or “the diseased”. The uncertainty of how bad the COVID-19 pandemic will get is creating high levels of stress that can be seen by how people are either over- or under-reacting during this global crisis. Feeling for being ‘out of our control’ of what is happening triggers negative emotions, such as fear and anger. Thus, by managing to minimise the uncertainty, or using it to the benefit of change towards a specific goal would create better resilient individuals or communities. Also, by making sure people hear information that is timely and relevant to their particular circumstances is also likely to help reduce short-term panic. Buheji (2020), McCloy (2020).In situations of extreme uncertainty, our brain struggles to organize itself to the new condition and at the same time, interpret the current challenges. This creates many sources of stress for both communities and individuals. This stress can increase if we do not see an end or alternative outcomes to this extreme uncertainty. Living with such change makes our minds tend to be busy, making many untested stories hundreds of times a day, and this creates further stress.
2.6. Learning from Previous Pandemics
- PAHO (2005) and WHO warned during the ‘avian influenza pandemic’ about a threat with incalculable health, social, and economic consequences, stating that “failure to take this threat seriously and prepare appropriately will have catastrophic consequences.” The psychological consequence was one of the main worries of WHO since the psychosocial disturbance about the pandemic survivors can exceed a person’s emotional response capacity. The most common immediate psychological disturbances among the pandemic survivors were depression and acute, transitory stress reactions. PAHO (2005) emphasised the importance of counting for a certain high level of stress among the population following a pandemic.
2.7. Eliminating Global Anxiety Pandemic by Managing COVID-19 Stress
- We accumulate stress by our body as a positive or an adverse reaction or response to a trigger and is generally a short-term experience or threat. Anxiety is a sustained mental health disorder that can be triggered by stress. Both stress and anxiety have similar physical symptoms, making it difficult to spot the differences between them, especially that both of them can lead to sleepless nights, exhaustion, excessive worry, lack of focus, irritability; besides other physical symptoms as rapid heart-rate, muscle tension, and headaches, Hurley (2019).During COVID-19 pandemic lockdown, quarantine and emphasized social isolation, stress is highly expected, as it is a reaction to the trigger of what is happening so fast or escalating in a few weeks or months. Therefore, the paper would not focus on the positive stress, but rather on the stress that results in stress that leads to poor mental concentration and physical strain.With the sustenance of stressful conditions and reactions, a mental health disorder might be developed by accumulated stress. This most probably is the turning point towards anxiety which be the main cause for more significant functional impairment in different aspects of life.In times of world crisis, as the COVID-19, it is normal that many people experience increased stress. Still, such stress must be managed by both the individuals and the healthcare leaders in the country or the community leaders. Therefore, a proper stratification for a well-designed emergency psychological intervention is crucial if we are to avoid that COVID-19 pandemic does not lead to another crisis represented by a mental health outbreak.
2.8. Emergency Psychological Interventions
- Despite the lack of data highlighting the psychological impacts associated with the COVID-19 outbreak, the need for applying emergency psychological interventions is widely emphasized. The target population in need of psychological interventions include those suspected or confirmed cases of COVID-19 infection, families, and friends of patients, health care professionals as well as the public as a whole. Confirmed and suspected patients with COVID-19 may experience fear from the consequences of the disease. Those patients having symptoms such as difficulty breathing, cough, fever, and chills or experiencing insomnia triggered by corticosteroid treatment can develop anxiety and mental distress. Additionally, patients in quarantine or forced social isolation might feel frustrated, bored and lonely. On the other hand, those which their job has to continue to mix with others might experience the feelings of guilt or have sustained hidden worries about being potential spreaders of infection around their families and others, or have to manage the stigma on their families, Xiang et al. (2020). Chen et al. (2020) reported other significant sources of stress among healthcare providers in China. Their stress comes having to care for the COVID-19 patients while carrying the fear of getting infected, or being the contact that spread the infection to their beloved ones. Besides, fear of lack of protective equipment, these health workers live the difficulty of managing emotionally distressed COVID-19 patients and feelings of incapability, while caring for critically ill or dying patients. Research evidence suggests that the provision of social support for healthcare providers is a critical social factor that can contribute to reduce stress and anxiety, improve sleep quality and enhance self-efficacy of healthcare providers, Xiao et al. (2020b). Consequently, social support enables the healthcare staff to maintain relatively stable emotions, thereby coping better with work pressure. Some of the measures taken by the concerned public authorities to respond to healthcare providers' pressures during the COVID-19 outbreak in China have included establishing psychological intervention services including online courses, hotline services, and in-site psychological counsellors. Other support efforts as the provision of accommodation for staff for rest away, supplying meals and other daily essentials and permitting staff to have a video recording of their daily routine with their loved one and to reduce family members' stress were also provided. This reflects health authorities’ investments in enhancing front people's capacity to better accommodate for high work demands. Likewise, the increased of social capital, known as a collection of resources either actual or potential including social trust, belonging and participation necessary to foster social cohesion, to be associated with positive effects on reducing stress and anxiety among individuals who self-isolated during COVID-19 pandemic, Xiao et al. (2020a).
2.9. Factors of Stress Response During Outbreaks
- Many factors determine our responses to a huge pandemic outbreak similar to COVID-19. The response factors might include our background, personality, age, social factors such as the level of family support, social capital support and the level of economic burden or socio-economic capacity. People who may respond more strongly to the stress of a crisis include older people and people with chronic diseases who are at higher risk for COVID-19: children and teens and people who are helping with the response to COVID-19, like doctors and other health care providers, or first responders, people who have mental health conditions including problems with substance use. Therefore, attention should be paid to support a more vulnerable population to stress.Managing stress response factors do not only help the vulnerable to survive this pandemic but improve how they would survive even more difficult and challenging life afterward, Okri (2020). To manage these stress response factors, we need to control the pandemic exposures first. In this research, we shall give the only sample of this exposure, encouraging further research on the subject.
2.10. Managing the ‘Pandemic Exposure’ Influence
- Since the beginning of the COVID-19 pandemic, many people been complaining about having continuous stress which inevitably threatens immunity and their overall well-being. Stress hormones affect our respiratory and cardiovascular systems. During the stress response, we need to breathe faster to distribute oxygen-rich blood to our body quickly. Therefore, if we already have a breathing problem caused a severe respiratory disease as COVID-19, we are going to make enormous pressure on our heart.Since no one knows that exact length and the end of the COVID-19 pandemic, staying under frequent stress might make the heart work too hard for too long, and this would raise the blood pressure rises, which increases the possibility of having a stroke or heart attack.Stress stimulates the immune system if it is for short term and an immediate situation. But stress hormones are known to weaken the immune system and reduce the body response to foreign viruses if the stress is sustained and become chronic. At the same time, stress found to increase the time it takes you to recover from any illness. Ali (2020)Therefore, WHO (2020) advised for finding out techniques that could boost our capacity to maintain mental wellness during the challenges of COVID-19. The WHO (2020) extended its guideline for managing the exposure of this fierce pandemic to the front-line workers as healthcare staff needs to use long term occupational capacity rather than repeated short-term crisis responses and prepare their mind and be resilient for the pressures that a COVID-19 pandemic expected to bring with it. This can be achieved by an effective communication model that is transparent and keep all the staff involved. The other technique that WHO (2020) recommended for managing the negative exposure of COVID-19 is switching the responsibilities between the workers to go from higher-stress areas to lower-stress ones and vice versa. Partnering between experienced and inexperienced workers using the buddy system also was recommended to reinforce safety procedures. WHO (2020) found that if outreaching personnel enter the community in pairs and if work breaks, flexible schedules are encouraged they would absorb the exposure of the stressful conditions any front line worker would go through.
2.11. Media as a Sample of ‘Stress Exposure’ Influence
- There are many types of ‘stress exposure’ influence we go through in our normal daily life and certainly this even more true during and after a crisis similar to COVID-19 pandemic. The American Institute of Stress (AIS, 2014) mentioned four primary examples that influence the presence of stress in the USA: financial issues, work-related issues, poor nutrition, the political environment, level of violence or crime, sleep deprivation, health crisis issue, and the media overload. In this research and due to the limitation of its scope and purpose, we shall focus on the media stress exposure, as a sample only.In our digital era, social media has become an essential element in shaping the Public’s perception of such a global event. The intensive media coverage and public interest in COVID-19 updates reflect the global concern of this pandemic. However, people's dependency on mass media during the crisis in search of information makes them more susceptible to its effects as it can strongly influence people behaviours. The repeated media exposure to massive information, also known as infodemic phenomena during the COVID 19 outbreak has directly influence and fragment social responses and disrupt the government efforts to contain it, Cinelli et al. (2020). For Instance, media sources describe it as a “killer virus” or perceive it as higher in risk compared to more conventional threats such as influenza or Ebola. This, in turn, can be associated with increased stress, anxiety and panic among healthcare providers and public and pose a threat for public health authorities seeking to mitigate the undesirable consequences of COVID-19.WHO (2020) called for minimising watching, reading or listening to news about COVID-19 as it causes people to feel anxious or distressed, recommending only to be selective in taking what helps to prepare for managing the pandemic and protecting self and the loved ones. This can start by combating infodemic through monitoring and filtering out false information, addressing rumors and correcting myths and misconceptions should be given high priority by the community leaders, Gao et al. (2020). At the same time, the absence of information, whether because the information is unknown to experts or because it is ineffectively communicated, raises the issue of uncertainty leading to heightened appraisals of threat among public and even healthcare professionals working under both physical and psychological pressure, Fischhoff et al. (2018). Therefore, timely updates of information from trusted sources, including experts-talk, is necessary to hinder public fear escalation and rumours amplification and eventually lessen stress responses.
2.12. Visualisation of ‘Stress Mitigation Strategies’
- During the long time of lockdown where millions of people had to stay within a limited space and in conditions they are not used to, attention, personal needs, and feelings are essential for survival. However, this requires refining and exploring deeper purposes of existence and life. Thus, here where people differ in their capacity and resilience in handling stressful conditions of a pandemic like COVID-19. Limits for handling different levels of stress depends on the boundaries and tactics we use to practice and acknowledge our needs and general wellness, which include preventative measures and specific forms of intervention to build more resilient solutions as coping, Buheji (2020). The body of knowledge has a significant gap in relevant to practising resilient economy practices such as visualising the ‘stress mitigation strategies’ which would lead construction like stress compensator framework during pandemics, as the COVID-19.Even though the literature gives directions for coping mechanisms, it does not have a framework for resilience strategies. The strategies needed should help to cope with and moderate the COVID-19 pandemic accumulated stress, regardless of the demographics, the symptoms and the type of isolation, i.e. social isolation, quarantine, and lockdown. The availability of such a framework would help to build a threshold of tolerance and expansion of the options available to handle such spikes of stress responses.
3. Proposing a ‘Pandemic Stress Compensator Framework’
- To create a pressure relief valve in the accumulated ‘pandemic exposure’ and mitigate the factors of ‘stress response’ during and after the COVID-19 crisis, a framework that influences the autonomous psychological intervention is proposed. Based on the literature reviewed, the framework targets to raise the capacity of the COVID-19 individuals and support the communities for managing stress, through two levels. The first level (line 1) focuses on what can be achieved, while the second level (line 2) focuses on the psychological support strategy. This system synthesised from the best practices during crisis and pandemics we call it ‘Pandemic Stress Compensator Framework’.Thus, the compensation of the accumulated stress works as follows. As shown in Figure (1) the first level (line 1) in the framework is set to focus on what can be achieved. Here the tools would depend on the best practices of reducing stress through seeking new opportunities during- and after-pandemic, besides visualising what could be the best outcome of this crisis. This should help people to move from ‘living with the uncertainty’ to the building the ‘capacity of coping with uncertainties’. The second level (line 2), as shown in Figure (1), focus on compensating the stress on the mindset through the ‘psychological support strategy’ which helps to manage or eliminate negative exposures and to support the first level. Here people would need to build their ‘social capital’ and target towards having or working on something, life goal, that would give them a sense of achievement. Such type of support would lead to better ‘psychological resilience’, hopefully with a personality that visualises a better world after the pandemic.
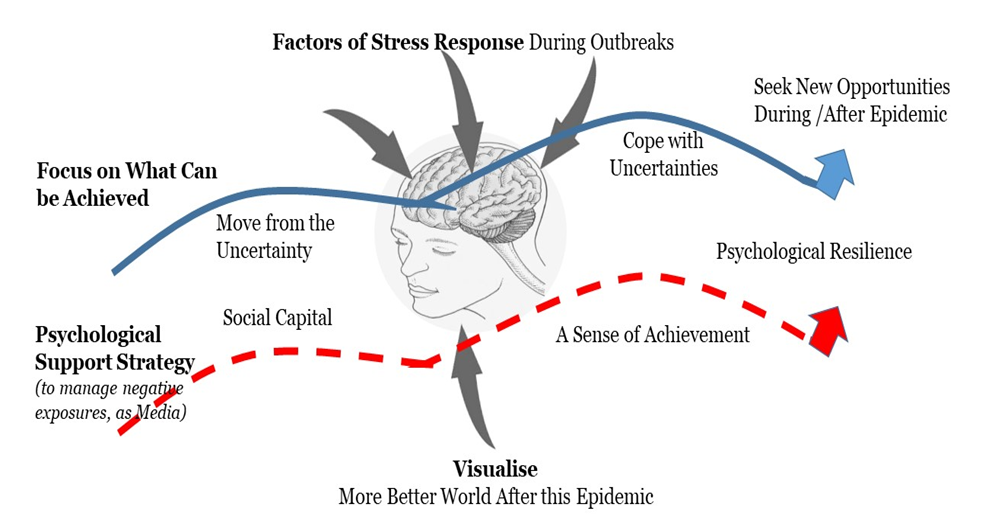 | Figure (1). Illustrates the Proposed ‘Pandemic Stress Compensator Framework’ |
4. Discussion
- Although the literature gives directions for the right mechanism for coping with stress, literary there is no ‘stress absorption framework’ based on clear resilience strategies that help us to deal with a pandemic or moderates its impacts. Having accumulated stress with a huge pandemic, as the COVID-19, needs an uncompromised immune system, with normal stress management mechanisms, this is not achievable. The world needs more than ever today's generic framework that prevents many people and communities from being vulnerable to both the virus and its consequences. So, in addition to washing our hands, and staying socially distant, we need a mindset that let us see hope and opportunities at the end of such quality of life devastating crisis. The COVID-19 have created a new pandemic accumulated stress, regardless of the demographics, the symptoms and the type of isolation, i.e. social isolation, quarantine, and lockdown; therefore, it needs to have a generic framework that helps people turn the negative daily exposure they are going through into a positive visualised outcome.The purpose of the first as proposed by the authors is to address the different exposures of uncertainty loops such as exploring better opportunities for jobs that give you wellness and appreciation for life, than just thinking about actually the job lost. The idea of the first level of the proposed framework then is to maintain the stamina to continue taking risks in life than to get chained and feel hopeless with a series of psychological setbacks. Based on the synthesis of the literature reviewed, people highly need to invest in their social capital in times of crisis to use it to bear the burdens. Besides, having a mind that searches for possibilities and visualises the achievements that can be realised during and after a pandemic would build a unique psychological resilience that could stay with the individual the rest of his. Hence, this framework helps to build a resilient mindset a newly aligned perspective that makes us see a pandemic as COVID-19 challenges as a situation that can be within our control. No matter what the COVID-19 would to the world, these disruptions can be compensated with such a mindset that would benefit from the absorbing mechanisms set within this framework two levels.
5. Conclusions and Recommendations
- In conclusion, the need for monitoring mental health information by public health authorities in the event such an actual pandemic is highly fundamental. Launching a ‘psychological support strategy’ to help those psychologically impacted by a pandemic as COVID-19 outbreak is also essential. Governments and concerned health authorities need to invest in ‘social capital’ and develop a clear strategy on best ways to using social media platforms more effectively, to compensate for the social isolation, as a key element to decrease psychological stress. At the same time, government and healthcare leaders could optimize the people's capacity and foster ‘psychological resilience’ by focusing on changing the people's mindsets. Thus, the concerned decision-makers would exploit the benefit of ‘seeking for opportunities’ amid adversities, to keep or build hope which would make people ‘cope with uncertainties’ and mitigate its related fear during a crisis. This paper raises necessary steps that are crucial to be tackled, in timely measures, to avoid far-reaching consequences than the current pandemic. There are two main limitations of this research. First, it did not go into the details of stress. i.e. the researchers avoided specifying which type of stress they are referring too, whether it is acute or chronic stress; as they believed it is beyond the scope of this research and need an empirical study. The other limitation is that this framework is not tested yet. Thus further studies are recommended for both testing and generalising the framework proposed.This research opens a path for seeing how to create more resilient communities and the world, through turning the pressures and specifically stress of the COVID-19 and similar pandemics to opportunities that can be realised. Further, the utilisation of the framework as a self-diagnostic or community assessment tool can be achieved once more research addressed in this line. The main implication of this study could help the public health officials and the psychiatric and mental wellness stakeholders plan for delivering services that would compensate for the stressful situations created the long-term social distancing, quarantine, lockdown, and isolation or the events of the pandemic on the communities of the world. This study framework supports the rationale for specific stress management protocol, and ensure sufficient supplies are provided. Finally, the researchers hope that this research would work as a pressure relief valve in the accumulated ‘pandemic exposure’ and mitigate the factors of ‘stress response’ that are occurring during and after the COVID-19 crisis and similar future outbreaks.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML