-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Psychology and Behavioral Sciences
p-ISSN: 2163-1948 e-ISSN: 2163-1956
2017; 7(3): 67-71
doi:10.5923/j.ijpbs.20170703.01

Constellation of Factors for Non-Compliance with Non-Pharmacological Advices to Percutaneous Coronary Intervention Patients
Mohiuddin Mohammad Alamgir1, M. Shafiqur Rahman2, Rukhsana Shaheen3
1Deputy Commandant, Combined Military Hospital Dhaka, Dhaka, Bangladesh
2Associate Professor (Community Medicine), Army Medical College Jessore, Jessore, Bangladesh
3Assistant Professor (Community Medicine), Shaheed Tajuddin Ahmed Medical College, Gazipur, Bangladesh
Correspondence to: Mohiuddin Mohammad Alamgir, Deputy Commandant, Combined Military Hospital Dhaka, Dhaka, Bangladesh.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

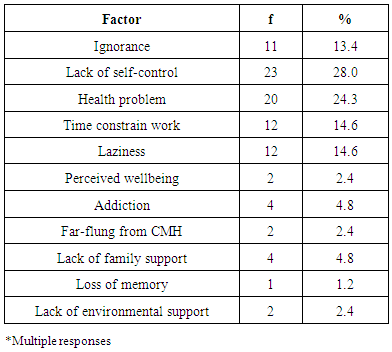
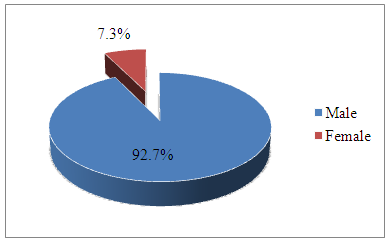
This study was an attempt to find out the constellation of factors interplaying for non-compliance with non-pharmacological advices to percutaneous coronary intervention patients attending Combined Military Hospital Dhaka, Bangladesh. This was a qualitative, obtrusive (reactive), descriptive socio-medical research using face to face in-depth interview with conveniently selected eighty-two ‘peer reviewed’ samples of percutaneous coronary intervention patients. Data were analyzed using limited descriptive statistics as well as Rothman’s concept of causal constellation, which were interpreted through both etic and emic approaches to draw conclusion. All ethical issues including avoiding plagiarism have been taken care of. The findings of the study show that necessary factors responsible for non-compliance of non-pharmacological management advices making web of constellation were ‘lack of self-control’, ‘addiction’, ‘ignorance’, ‘laziness’, ‘health problem’, and ‘time constrain work’. The study concluded with the suggestions for strengthening health literacy among percutaneous coronary intervention patients in Combined Military Hospital Dhaka. The study hinted for further probing of constellation factors among such patients in general population.
Keywords: Non-compliance, Non-pharmacological advice, Percutaneous coronary intervention patient
Cite this paper: Mohiuddin Mohammad Alamgir, M. Shafiqur Rahman, Rukhsana Shaheen, Constellation of Factors for Non-Compliance with Non-Pharmacological Advices to Percutaneous Coronary Intervention Patients, International Journal of Psychology and Behavioral Sciences, Vol. 7 No. 3, 2017, pp. 67-71. doi: 10.5923/j.ijpbs.20170703.01.
Article Outline
1. Introduction
- Evolution of life in earth, not just a geologic second ago, led to the appearance of human life. Each human follows a life course which ends with death [1]. Death is preceded by certain diseases that have two types of dimensions: communicable disease and non-communicable disease (NCD). Non-communicable diseases currently cause more deaths than all other causes combined, and NCD deaths are projected to increase from 38 million in 2012 to 52 million by 2030 [2]. Death of a human being before age of seventy years is considered as premature [3]. At present there appears an unprecedented opportunity to alter the course of NCDs which can prevent the majority of premature deaths. One pattern of NCD is coronary artery disease (CAD), which is one of the leading causes of mortality and morbidity in developed world, as well as developing countries like Bangladesh [4]. Moreover, it continues to be a major public health problem. Treatment of CAD is essential and coronary artery bypass grafting (CABG) was the only alternative to pharmacotherapy for the treatment of CAD till 1977. After that gradually, another modality of treatment, that is, percutaneous coronary intervention (PCI) has surpassed CABG as the most common means for treating CAD because of improvement of materials used, the use of stents, and pharmacotherapy. Percutaneous coronary intervention is safe due to reduced radiation exposure, quick mobilization of patient and no procedural complication [5]. Persons having established CAD and undergone PCI are already at very high risk of development of further events of cardiovascular disease (CVD) and need compliance with life-long follow-up of medical advices. Patients’ compliance to medical advices is crucial for better prognosis, which involves many factors, and makes it difficult to comply life-long. The post-PCI management of CAD patients involves both pharmacological (i.e., medicines) and non-pharmacological (i.e., lifestyle advices) management for restoration of normal functional coronary artery and/ or treatment of co-morbid medical condition(s) [6]. The estimations of World Health Organization (WHO) indicate that in developed countries compliance to long term medical advices for NCDs in the general population is around 50.0 percent, which is much lower in developing countries [7]. This study aims to look into the constellation of factors and find out the necessary causes that influence non-compliance with non-pharmacological management advices after discharge among PCI patients attending Combined Military Hospital (CMH) Dhaka, Bangladesh.
1.1. Research Theme
- Just as statistical significance establishes causal relationship in quantitative studies, Rothman’s causal constellation pies point to causal association in qualitative studies [8]. Compliance of treatment follow-up, where many different component causes have been identified for each of its types in relation to ‘universal variables’, this study delved into identification of a final common pathway representing a web of causation comprising of only necessary causes for non-compliance with non-pharmacological management advices.
2. Methods and Materials
- The study was approved by the Ethical Committee of the Armed Forces Medical Institute, Dhaka, Bangladesh. The purpose of the research was explained to participants, who thereafter gave verbal informed consent.This qualitative obtrusive (reactive) descriptive socio-medical study was conducted in the naturalistic setting of CMH Dhaka. The study population were patients with PCI who attended CMH Dhaka for follow-up advice. No specific time interval between follow-up advice and interview was considered. Convenient variety of non-probability sampling technique was applied during January and February 2016 to pick up total 82 sample units, which was agreed on peer review and considering data collection time in hand, PCI patients flow per day, and the time allocated for each interview through ‘grand tour neutral probing’. Coherent PCI patients aged 18 years or more of both sexes were included. Those, not entitled to get treatment from CMH Dhaka, denying consent, or unable to communicate were excluded. Interviews were continued until content saturation was reached, or no new themes emerged. Some interviews were audio-taped and transcribed to facilitate analysis.
3. Result
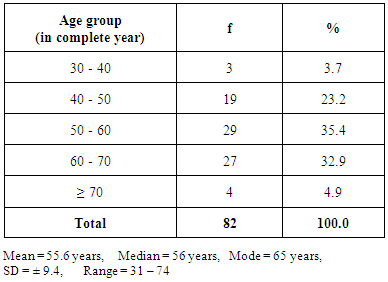
- Sex and Age Distribution of PCI PatientsThe study revealed that out of total eighty-two PCI patients 92.7 percent of the patients were male and the rest 7.3 percent were female as shown in Illustration 1.
 | Illustration 1. Pie Chart Showing sex Distribution of PCI Patients |
|
|
|
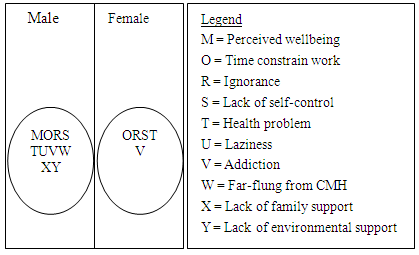 | Illustration 2. Rothman’s Causal Pies Showing Constellation of Factors for Non-compliance with Non- pharmacological Management Advice by Sex |
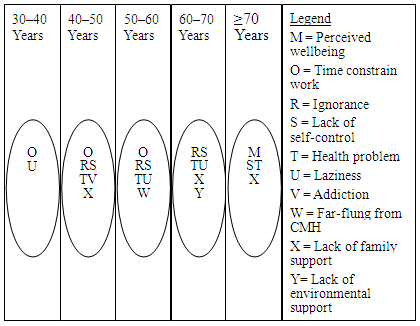 | Illustration 3. Rothman’s Causal Pies Showing Constellation of Factors for Non-compliance of Non- pharmacological Management Advice by Age |
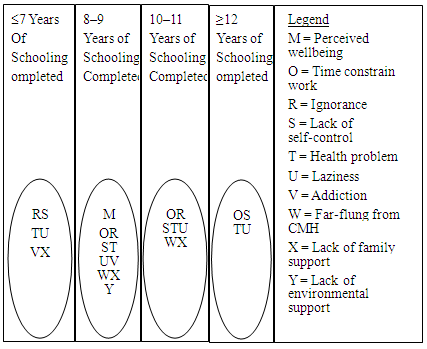 | Illustration 4. Rothman’s Causal Pies Showing Constellation of Factors for Non-compliance with Non-pharmacological Management Advice by Educational Qualification |
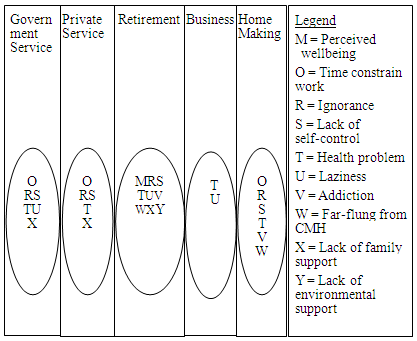 | Illustration 5. Rothman’s Causal Pies Showing Constellation of Factors for Non-compliance with Non-pharmacological Management Advice by Occupation |
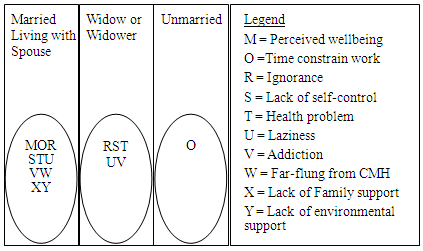 | Illustration 6. Rothman’s Causal Pies Showing Constellation of Factors for Non-compliance of Non-pharmacological Management Advice by Marital Status |
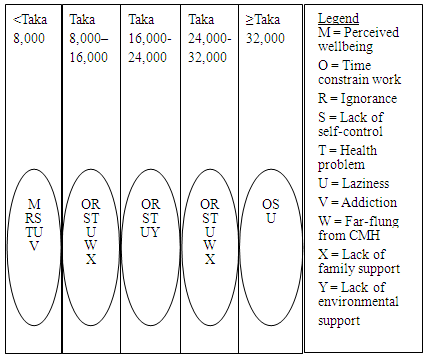 | Illustration 7. Rothman’s Causal Pies Showing Constellation of Factors for Non-compliance with Non-pharmacological Management Advice by Monthly Income |
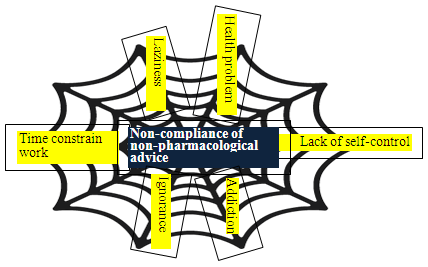 | Illustration 8. Spider-Web Diagram Showing Web of Causation for Non-compliance of non-pharmacological Management Advice |
4. Discussions
- Collectively the necessary causes form the constellation of cause for the outcome of compliance. Among all the PCI patients, ‘health problem’, ‘ignorance’, ‘time constrain work’ ‘lack of self-control’, ‘addiction’, and ‘laziness’ emerged as constellation of cause for non-compliance with non-pharmacological management advices. In short, the constellation factors for non-compliance with non-pharmacological management advices are the outcome of both nature and nurture components of bio-psycho-social environment [9]. Probably, cohesively these factors interact in a synergistic way for non-compliance. To adhere with non-pharmacological management, programs of health literacy intervention maybe instituted among PCI patients and their associates in CMH Dhaka.
5. Conclusions
- The treatment compliance of percutaneous coronary intervention patients is the outcome of bio-psycho-social phenomena. The phenomena were analyzed using Rothman’s causal pies concept. Constellation of factors for non-compliance to non-pharmacological management advices among percutaneous coronary intervention management are ‘ignorance’, ‘time constrain work’, ‘lack of self-control’, ‘addiction’, ‘laziness’, and ‘health problem’. Recommendations suggested from this study:• To minimize the problem of non-compliance, appropriate efforts are required in the form of motivational counseling campaign or health educational program for the percutaneous coronary intervention patients in Combined Military Hospital Dhaka for reinforcing the compliance with medical management. • Further studies are required among percutaneous coronary intervention patients in general population of Bangladesh for better understanding of compliance with follow-up advices in respect of their social anatomy and concomitant medication use.
ACKNOWLEDGEMENTS
- The researchers wish to extend their gratitude to the authority of Combined Military Hospital Dhaka for the support in collecting data from the hospital.The researchers remain indebted to all the participants who agreed to cooperate in the process of gathering data, without which a work like this would not be possible.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML