-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Psychology and Behavioral Sciences
p-ISSN: 2163-1948 e-ISSN: 2163-1956
2017; 7(1): 41-48
doi:10.5923/j.ijpbs.20170701.07

Subjective Sleep Quality and Anger
Félix Arbinaga
Department of Clinical and Experimental Psychology University of Huelva, Huelva, Spain
Correspondence to: Félix Arbinaga, Department of Clinical and Experimental Psychology University of Huelva, Huelva, Spain.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Anger as an emotion has proven to influence health. However, there is little research about the relationship between anger and subjective sleep quality. This paper analyses anger and its expression regarding subjective sleep quality. 581 people have participated (58 % of women) with an age of M=32.19-SD=15.59 years. The PittsburghSleepQualityIndexand theState-TraitAngerExpressionInventory-2were applied. People with a worse subjective sleep quality (> 5 PSQI score) face a higher chance of experimenting trait-anger, anger expression-in and anger expression-out in a degree that may interfere with their optimum behaviour. People with a sleep duration of <7 h, compared to those that claim to sleep ≥7 h, show a higher probability of obtaining trait-anger, state-anger, emotion, verbal expression and physical expression scores that interfere with their behaviour. To point out the necessity of considering objective measures about sleep and its relations with negative emotions.
Keywords: Anger, Emotional Control, Sleep
Cite this paper: Félix Arbinaga, Subjective Sleep Quality and Anger, International Journal of Psychology and Behavioral Sciences, Vol. 7 No. 1, 2017, pp. 41-48. doi: 10.5923/j.ijpbs.20170701.07.
Article Outline
1. Introduction
- Anger is one of the emotions considered basic or primary that is characterised by activation and tendency to attack. It usually comes up as a reaction to a threat, coercion or harm, or before a situation of frustration or differential treatment [1]. If the anger is intense and sustained over time, it usually affects health through sympathetic hyperactivity [2].Spielberger, Jacobs, Russel and Crane [3] differentiated between Anger, Hostility and Aggression, being the former a necessary component, yet not sufficient, of the other two. Their model is based on anger as an emotion characterised by feelings of irritation or annoyance of variable intensity; where it is possible to differentiate state-anger from trait-anger, the latter being more or less stable. Because of its influence over health, the way anger is expressed has to be taken into consideration (anger-in, anger-out). Both anger-in, or internalised, and anger-out, or externalised, have been related to aggravating factors in cardiovascular health [4, 5]. However, it has also been suggested that anger-out is a protective factor for myocardial infarction and stroke [6], while also improving sleep quality of coronary heart disease patients [7, 8].The emotions have been studied regarding their relations with sleep [9], highlighting its bidirectional nature. Sleep disorders affect emotional reactivity, while sleep quality is strongly affected by emotional reactions to previous events [10-12]. Sleep deprivation and insomnia are related to the increase of emotional reactivity and the greater activation of the amygdala before emotional stimul, being REM sleep important for emotional processing and emotion reorganisation specific to brain activity [10, 13]. Sleep deprivation has been showed to be closely tied to aggressive incidents in humans and animals [14-16] and sleep alterations after an exposure to a traumatic event may contribute to difficulties in emotional regulation and to exacerbate the negative consequences [17, 18]. Daytime emotional stress is mitigated in accordance with the sleep quality and the emotional self-control possessed; the greater the self-control, the greater mitigation of the effects [19].The way that previous emotional states to sleep affect REM sleep and the subsequent modulation of the sympathetic activity during the sleeping period [20] have also been studied. Daytime emotional states are associated to sleep quality; the people that acknowledge daily experiences with negative emotions such as anxiety or irritability often exhibit poor sleep quality [21, 22], insomnia [23, 24] and other related issues. Daily stressful events, alongside an inadequate emotional reaction to them, are characterised in implying a lower sleep spindle density [25] and alterations both to sleep duration and REM sleep [26].The specific study about anger and its relations with subjective sleep quality has been researched very little [27-29]; albeit it has been considered indirectly in studies about hostility and sleep [15, 30-32] or as a limited part of broader studies [7, 11, 27, 33-36].It may be pointed out that morningness-eveningness appears to be related to impulsivity and anger in the general population. Impulsivity can exert a big influence over the association between morningness-eveningness and anger, as a moderator or mediator factor [33].Evidence has been provided about how, amongst the middle-aged adult population, high levels of trait-anger are associated with sleep disorder symptoms [28]. Stoia-Caraballo, et al., [29] discovered that anger rumination and negative affect deteriorate sleep quality in university students. It is indicated that patients diagnosed with insomnia show more alexithymic characteristics, a higher anger level and anger expression than the control group or group without insomnia [27]. The increment of anger-in increases the probability of poor sleep quality; whereas the increase of anger-out can reduce such probability in patients with coronary heart disease (CHD) [7, 8]. It is pointed out that sleep quality can act as a protective factor when there is a lower cardiac vagal control [37].On the other hand, it is indicated that the control of the emotional expression helps to reduce its impact over sleep [19]. It has thus been proposed that the excessive and inadequate expression or suppression of anger is associated with a risky lifestyle at early ages [34]; proving the existence of significant relations between the answers of the young offenders in measures of anger and general health [35].As it has already been stated, by modulating the sympathetic activity, intense and sustained over time anger may lead to health issues [2, 20]. Sympathetic hyperactivity has proven to be relevant in sleep and the pathology associated. For this reason, influences have been determined in the deterioration of the baroreflex sensitivity and sleep fragmentation [26], affecting as well the obstructive sleep apnoea [38] among others. With the available evidence, along with the influence that anger has shown over other pathologies that, direct or indirectly, are related to sleep [7, 8, 27, 33], it suggests that if the modification of anger expression improves sleep quality or reduces cardiovascular morbidity and mortality, it deserves more research.In this sense, the proposed aim was to analyse how anger is characterised and the way it is expressed, with regard to subjective sleep quality. In this sense, finding higher scores was expected for state-anger and trait-anger in those people that present a poor subjective sleep quality or other problems associated to it. In the same way, it was expected that those people with some sleep problems indicated a higher score for anger expression-out (anger-out) and anger expression-in (anger-in) and less control over them.
2. Method
2.1. Participants
- A total amount of 581 people have participated (58% of women) with M=32.19 years of age and an SD=15.59 (Min=19 and Max=64 years of age). 4.1% of the participants said they had no education, 9.3% a primary education, 9.1% a secondary education and 77.5% that they were attending university or had finished their university education. Regarding their civil status, 71.4% claimed to be single, 22.2% married, 2.6% separated/divorced and 3.8% widowed.
2.2. Procedure
- The data collection took place between September 2015 and June 2016. The contact with the participants, to perform the tests, was carried out by different procedures (university class presentations and announcements, community centres and senior care centres). The participation requirements were to know how to read and write, to not suffer from a chronic illness, to sign an informed consent and to take part in the study voluntarily. The study was approved by the University's Bioethics Committee.
2.3. Instruments
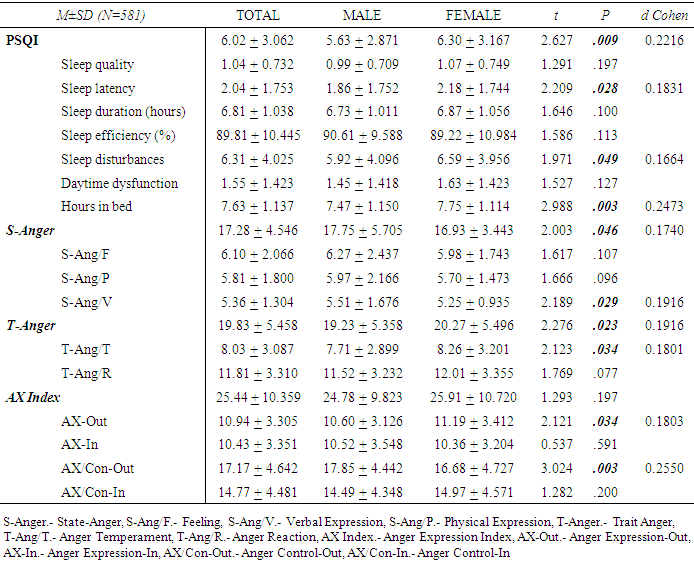
- A brief interview was conducted ad hoc about sociodemographic variables (age, gender, civil status, level of education, weight, height, Body Mass Index (B.M.I.)) and existing chronic illnesses.To assess the Subjective Sleep Quality the Pittsburgh Sleep Quality Index (PSQI) [39] was applied in its Spanish adaptation [40]. It showed a high internal consistency (Cronbach’s alpha of .81). The predictive validity data of Buysse et al. [39] indicated that if a cut-off point of 5 was set (score > 5 defines worse sleep quality), the sensitivity was 89.6% and the specificity 86.5%. The 19 items analyse the defining factors of sleep quality, grouped into seven components: quality, latency, duration, efficiency and sleep disturbances, use of sleeping medications and daytime dysfunction. Each component is assigned a 0-3 score. The total PSQI score is obtained by adding the seven component scores. It should vary from 0 to 21 points (the higher the score, the worse the sleep quality).To evaluate Emotion-Anger the State-Trait Anger Expression Inventory-2 (STAXI-2) [41] was considered in its Spanish adaptation [42]. The Spanish STAXI-2, with 49 items, keeps the same structure of the original. A total score for State-Anger (S-Anger) is obtained, with three subscales that assess the different components of the intensity of anger as an emotional state: Feeling (S-Ang/F), Verbal Expression (S-Ang/V) and Physical Expression (S-Ang/P). A total score for Trait-Anger (T-Anger) with two subscales Anger temperament (T-Ang/T) and Anger reaction (T-Ang/R). Lastly, a scale for the Anger Expression Index (AX Index) with four subscales: Anger Expression-Out (AX-Out), Anger Expression-In (AX-In), Anger Control-Out (AX/Con-Out), Anger Control-In (AX/Con-In). A total score is obtained that provides a general measurement of the anger expression and control. The authors report a test-retest correlation of .71 and a Cronbach's alpha coefficient of .89 for the State-Anger scale, of .82 for the Trait-Anger one and of .69 for the Anger Expression Index [42]. For [43] the subjects with scores higher than 75 centile, in the Trait-Anger and Anger Expression Index scales, experimented or expressed feelings of anger to a degree that may interfere with their optimum behaviour; not happening the same in the State-Anger scale for which a different distribution of the scores was carried out.
2.4. Statistical Analysis
- Descriptive statistics are considered to characterise the sample (e.g. M, Sd). The indexes of internal consistency were calculated using the Cronbach’s alpha for the PSQI, the State-Anger scale (Feeling, Physical Expression, Verbal Expression), the Trait-Anger scale (Temperament, Anger Reaction) and the Anger Expression Index (Anger Expression-Out, Anger Expression-In, Anger Control-Out, Anger Control-In). The Significance Tests, such as the Chi-square test for categorical variables and the analysis of variance (ANOVA) along with Student's ttest, with least significant difference post-hoc tests (Scheffe y Bonferroni) for continuous variables. The effect size has been calculated using Cohen's d, Phi coefficient and eta-squared (ηp2). The Odds Ratio (OR) has been calculated as a degree of association between a exposure and a result. A bivariate Pearson correlation analysis has been carried out between the studied variables.
3. Results
- The mean age of the sample group is 32.19 years of age (SD=15.59) (see Table 1), obtaining significant differences between men and women and in weight, height and BMI. In this sense, the 4.6% of the sample showed underweight, the 65.4% normal weight and the 29.9% overweight.
|
|
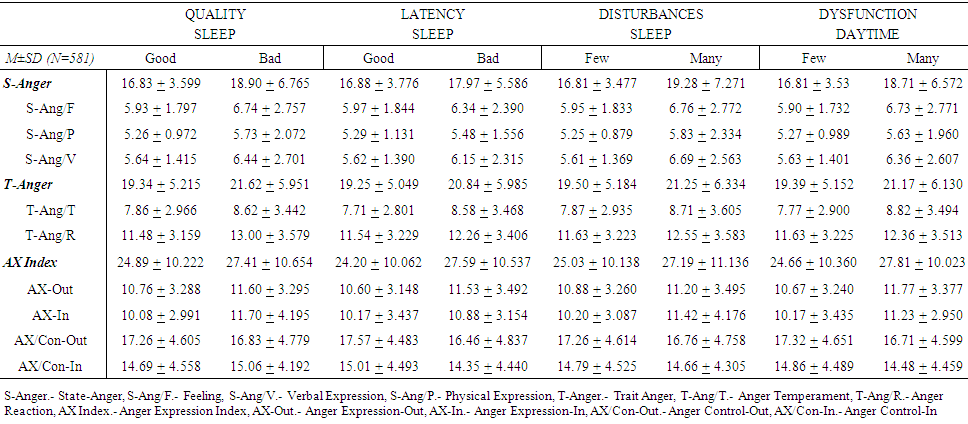 | Table 3. Mean scores and standard deviation for the STAXI-2 scales according to sleep problem categories in the PSQI |
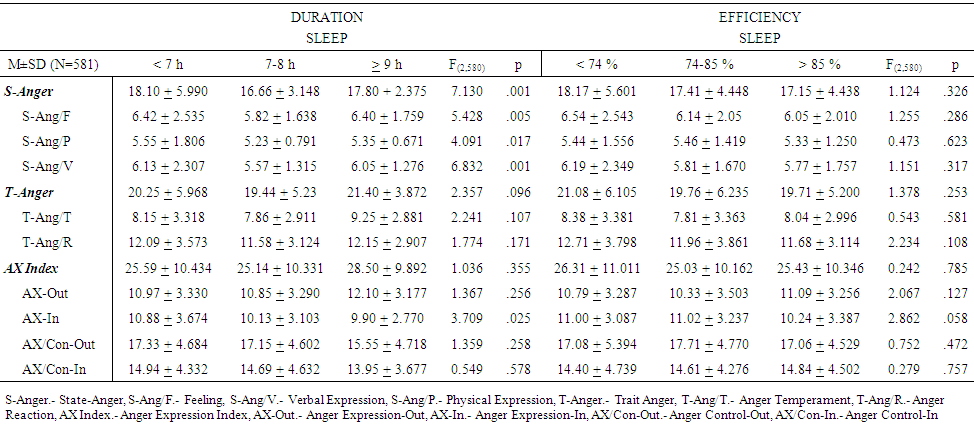 | Table 4. ANOVA between the scores for the STAXI-2 scales according to PSQI Sleep duration and Sleep Efficiency |
4. Discussion
- The proposed aim was to analyse how anger is characterised and the way it is expressed, with regard to subjective sleep quality. In this sense, it was expected to find higher scores for stateanger and trait-anger in those people that present a poor subjective sleep quality or other problems associated to it. In the same way, it was expected that the people with some sleep problems indicated a higher score for anger expression-out (anger-out) and anger expression-in (anger-in) and less control over them.The data has shown that the people with a worse subjective sleep quality (> 5 PSQI score) face a higher chance of obtaining higher scores, in a degree that may interfere with their optimum behaviour, for trait-anger, for anger expression-in and for verbal expression; but not for state-anger, feeling and physical expression. When the sleep quality item is analysed, the participants that present poor sleep quality obtain higher scores for all the anger-scales, except for anger control-out and anger control-in, where no differences exist with those that admit to a good sleep quality. These data would support the findings of Engin et al, [27] who stated that people with insomnia would present a higher level for anger and anger expression scores.In this same sense, it has become apparent that the people considered to present a high sleep disturbance obtain higher scores both for the state-anger scale and the trait-anger scale and for each of their subscales. However, for the anger expression index they only show worse scores for anger expression-in; not being any different for anger control-in and anger control-out. Therefore, they show a higher probability of interfering scores for trait-anger and anger reactions. Having taking into consideration the hours they claim to sleep, it has been noted that the people who sleep less than 7 h, compared to those that sleep more than 7 h, show a higher risk of showing levels of trait-anger, state-anger, feeling, verbal expression and physical expression that might interfere with their daily activities. Nevertheless, even if the participants manifested differential sleep efficiency, it does not seem to be reflected in the different anger scales; neither for trait-anger, for state-anger nor for the anger expression index.These data support the findings of Shin et. al., [28], in middle-aged adults, when considering that the levels of trait-anger are usually associated with sleep disorder symptoms. In the same way, the results obtained for anger expression-in and verbal expression, in people that show a worse subjective sleep quality, should confirm the indications of Stoia-Caraballo, et al., [29] who found that anger rumination and negative affect worsened sleep quality for university students or confirm the statement that internalised anger should increase the probability of a worse sleep quality [7, 8].Diestel et al. [19] stated that the control of the emotional expression helps to reduce its impact over sleep. However, it has been proven that both anger control-out and anger control-in only manifested differences in relation with sleep latency. Therefore the participants that need little time to fall asleep show a higher anger control-out and anger control-in. That said, control has not behaved differently with regard to sleep disturbances, sleep quality and daytime sleep related dysfunctions.Lastly, it may be pointed out that for the anger emotion, either as a state or trait, the way it is expressed is directly related to a worse sleep quality and to the sleep problems associated that were analysed. It should be noted that the anger control-out and anger control-in scores only appear to be different between the people that need little time to fall asleep and those with a higher latency. A relevant aspect is that no differences were detected in any anger component between the participants according to their sleep efficiency.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML