-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Psychology and Behavioral Sciences
p-ISSN: 2163-1948 e-ISSN: 2163-1956
2017; 7(1): 27-31
doi:10.5923/j.ijpbs.20170701.05

Parental Stress Experiences with NICU Admission in a Tertiary Care Centre
Neetika Ashwani1, Neela Aruna Rekha2, C. Suresh Kumar3
1Special Newborn Care Unit (SNCU), Niloufer Hospital, Osmania Medical College, Hyderabad, India
2Department of Gynaecology and Obstetrics, Niloufer Hospital, Osmania Medical College, Hyderabad, India
3Department of Neonatology, Niloufer Hospital, Osmania Medical College, Hyderabad, India
Correspondence to: Neetika Ashwani, Special Newborn Care Unit (SNCU), Niloufer Hospital, Osmania Medical College, Hyderabad, India.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: To determine the stress levels among parents of babies admitted in Neonatal Intensive Care Unit (NICU) and to identify demographic parameters that influence their stress levels. Methods: A cross sectional study was done at a tertiary care hospital in South India over a three month period. Stress levels were assessed using Parental Stressor Scale: Neonatal Intensive Care Unit (PSS: NICU) questionnaire among 100 extramural NICU parents (mother or father) by doctors with more than 24 hours of admission. Stress was quantified using Likert scale. The statistical analysis was done using R programming software. Results: The mean scores for the subscales sights and sounds, looks and behavior, alteration in the parental role and staff behavior and communication were (1.75), (2.11), (2.48) and (1.47) respectively. Maturity of baby, parents’ gender in sights and sounds domain and parents’ education in staff behavior domain were associated with higher stress levels respectively, as rest of the stress levels are not significant due to small sample size. Conclusions: Combined, the findings of the present study which not only documents stress experienced by parents of NICU infants but also highlight emotional consequences and the individual nature of parents’ response to the NICU experience. NICU parents are under moderate stress and appropriate counseling targeted towards specific stressors is required. Future research should monitor more closely how parental stress changes throughout the infant’s NICU stay. This information can be used to design effective coping strategies for parents at different time points during their infant’s hospitalization.
Keywords: Parents’ stress, Neonatal intensive care unit (NICU), Stressor PSS: NICU
Cite this paper: Neetika Ashwani, Neela Aruna Rekha, C. Suresh Kumar, Parental Stress Experiences with NICU Admission in a Tertiary Care Centre, International Journal of Psychology and Behavioral Sciences, Vol. 7 No. 1, 2017, pp. 27-31. doi: 10.5923/j.ijpbs.20170701.05.
Article Outline
1. Introduction
- Neonatal Intensive Care Unit (NICU) environment has the potential to exacerbate stress for parents of infants admitted to the unit. NICU mothers especially experience multiple stressors related to preterm birth, medical condition of the baby, complexity of the NICU environment and perceived vulnerability of the infant, in addition to stressors associated with the normal transition process to parenthood [1, 2].Environmental factors that can influence parents’ unique reaction to having an infant in the NICU might include difficulty in fulfilling their parental role, the medical equipment used for intervention, and the communication patterns and behavior of the staff [3, 4]. Miles and Carter [3] explained that as a result of the various factors that can influence the parents, each parent develops his or her own way of cognitively appraising, or making judgments about the NICU experience. For example, some parents, may view their situation as positive since their infant is getting the care he or she needs, others may see it as negative when the infant or staff is unable to correspond to their expectations or needs, some parents may cope by using the environmental resources available to them such as the support of the NICU staff, while others may use personal resources such as family, friends or financial assets.Parental stress resulting from experiences with infants hospitalized in NICU is well documented in western literature [1-7]. Less literature review is found for developing countries. Increased information about how parents of hospitalized high-risk infants perceive NICU, and also an understanding of the needs of such parents may enable NICU Staff to identify parents at risk and plan interventions to meet those needs and promote family functioning. In light of this, it is important to identify factors associated with increased parental stress in order to develop effective interventions for improving mental health in NICU parents.Niloufer Hospital for Women & Children is a tertiary care teaching hospital that receives several sick extramural neonates delivered in the state of Telangana and adjoining states of Maharashtra, Andhra Pradesh and Karnataka. This study was conducted to determine the levels of stress experienced by parents of babies admitted in NICU in a tertiary care centre in south India. This can help the staff to understand the problems perceived by the parents. Small changes during the hospital stay can meet bigger expectations especially for mothers, to alleviate postpartum stress.
2. Material & Methods
- Design and SamplingThe current study is a cross sectional study carried out at Niloufer Hosptial, a tertiary care hospital catering to maternal and child health in Telangana, a southern state of India. A convenient sample of 100 parents was taken based on a previous study [8]. Hundred parents (mothers or fathers) of high-risk infants who were hospitalized in the NICU of Niloufer Hospital, Osmania medical college were recruited for the study. The study period was from September 2016 to November 2016. Informed consent was obtained from the parents for the study. Inclusion criteria for the study were parents of the preterm babies and neonates with other illnesses (like asphyxia, birth injuries, congenital malformations, Jaundice, etc) that necessitated their admissions into the unit for special care. For their information to be included in the study, their infants had to remain in the NICU for at least 24 hours. Infants born in the hospital were excluded from the study. To obtain data on stress, we approached the parents at a time when they were visiting but not holding their babies, and when not involved with other NICU personnel. Questionnaires were administered at that time as well. Instruments used for the study include:Parental Stressor Scale: Neonatal Intensive Unit (PSSNICU) developed by Miles and Funk [9] and designed to measure the parents’ perception of stressors within the NICU. The scale consists of four sub-scales that measure stress related to a) sights and sounds, b) appearance and behavior of the infant, c) the impact on parents’ role and their relationship with their baby, and d) the parents’ relationship and communication with the staff. The responses to the PSS:NICU were scored on a 5-point Likert scale ranging from 1 point for “not at all stressful”, 2 points for “mild stress”, 3 points for “fairly moderate stress”, 4 points for “very stressful” and 5 points for “extreme/ severe stress”. Higher scores indicate more stress.These demographic data was obtained from the medical records and included information on the parents’ age, marital status, ethnicity, education and occupation. Data collected on the infants’ demography included their gestational age, birth weight, diagnosis and length of stay.Data AnalysisData was analyzed using R programming software version 3.0. For descriptive statistics, Mean and SD for continuous variables and frequencies for categorical variables were calculated. Normality test was done using Shapiro wilk test. Though variables were not normally distributed, t test and ANOVA was performed as the sample size was large enough (n=100) for two and more than two groups respectively. Simple and multiple linear regression was carried with and without adjusting for other confounding variables respectively. P value <0.05 was considered statistically significant.
3. Results
- Mean age of the parents participating in the study was 23.9 ± 3.2 years. Twelve fathers and eighty eight mothers participated in the study. Fifty eight of the births were spontaneous vaginal while forty two were cesarean deliveries. Thirteen (13%) of the parents were not formally educated, 14% went to primary school, 49 % received high school education while 24% were graduates. The major maternal obstetric complications recorded were hypertension (10%), hypothyroidism (8%) and anemia (7%). The profile of the neonates was as the following: 57% of them were the first child and 57% were boys. Their mean (SD) weight was 2093 ± 755 grams and ranged from 750 to 3500 grams; the gestational age at birth ranged from 27 to 40 weeks with a mean (SD) of 34.58 ± 3.6 weeks. Sepsis (37%) was the most common admission diagnosis followed by prematurity with hyaline membrane disease (26%), respiratory distress syndrome (18%), birth asphyxia (8%) and others.Table 1 depicts the various components of PSS: NICU and their corresponding parental stress scores. Mean (SD) scores of the components were as following: sights and sounds 1.75 (0.317), infants’ behavior 2.11 (0.146), parental role alteration 2.48 (0.486) and staff behavior 1.47 (0.72). Demographic characteristics like parents’ gender, age, maturity of the baby, length of stay and education are shown in (table 2). Parents’ age and length of stay did not significantly affect the stress levels with NICU admission. However, gestation age, parents’ gender and education were associated with higher levels of stress. The stress level of fathers was found to be significantly higher than mothers in the sights and sounds domain. Term neonates affected the parents more in the sights and sounds domain. Parents with lesser education faced problems with the staff behavior and communication domain. Linear regression was conducted for all the four components. However, only sights and sounds and staff role were significant after adjusting for other confounding variables and are shown in Table 3. Similar to bivariate analysis, Parents’ gender (P=0.001) and maturity of the baby (P=0.011) were found significantly associated with sights and sounds. Staff behavior was significantly associated with education (p=0.002). The beta coefficients were lowest in uneducated compared to other levels of education.
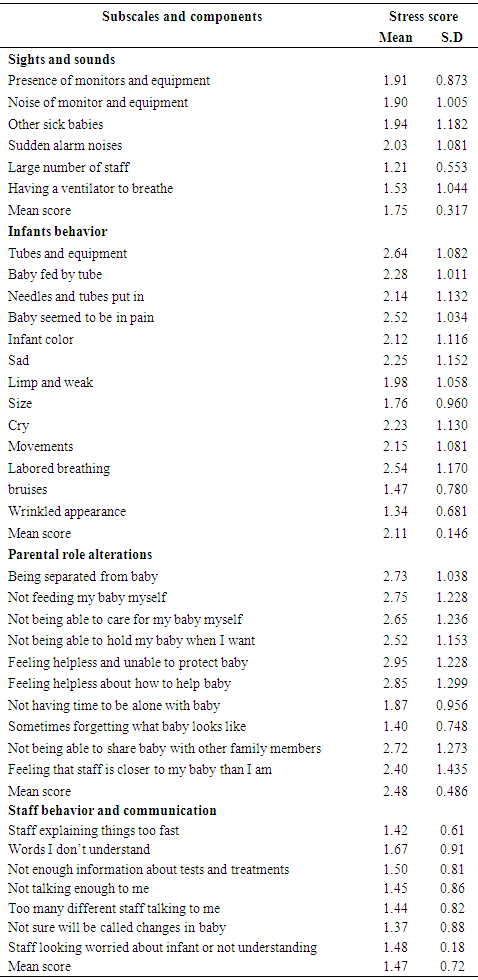 | Table 1. Parental stress measured by PSS:NICU (n=100) |
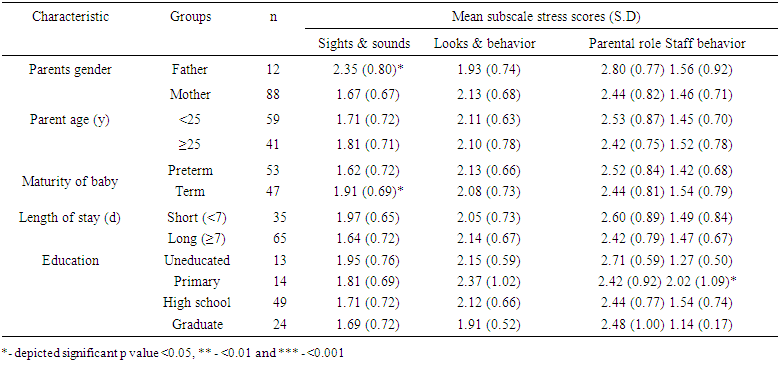 | Table 2. Parental stress levels in relation to demographic parameters |
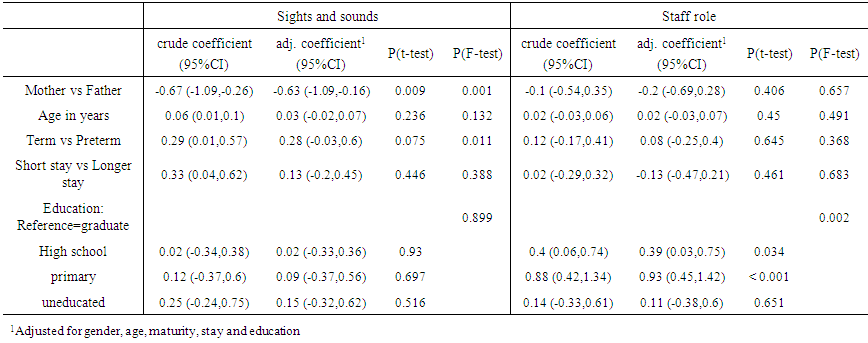 | Table 3. Simple and Multiple linear regression analysis for sight and sounds (Adjusted model P <0.001) and Staff role (Adjusted model P value <0.001) |
4. Discussion
- The aim of this study was to assess the stress levels in parents and the impact of various factors affecting the levels of stress in parents of low socio economic group in a south Indian tertiary hospital. The magnitude of parents sources of stress in the current study, assessed by the PSS:NICU with “alteration in parenting role” a leading source of stress followed by "the appearance and behavior of the infants and special treatment", “sights and sounds” and “staff behavior” were detected similar to that reported in previous publications with mean scores of (2.48), (2.11), (1.75) and (1.47) respectively [5, 10-12]. The results of the present study in terms of environmental stressors showed that "the sudden sound of the monitor buzzer and special facilities and equipments of the unit", respectively, were the most experienced stressor agents by parents with high risk neonates in NICU. Among the individual components, “Feeling helpless and unable to protect baby, Feeling helpless about how to help baby and Not feeding my baby myself” were the stressors with maximum scores. The study indicated that parental stress for NICU sights and sounds is significantly influenced by parents’ gender, infant gestational age, a few parents reported stress in the area of staff and communication similar to previous studies [13, 14]. According to studies [8, 10], consistent predictors of stress were length of stay, extreme prematurity, increased maternal age and cardiovascular diagnosis. In the present study, parents’ gender, staff communication and maturity of baby were significantly associated with higher parental stress. The study indicated stress and anxiety experienced by fathers appears to be significant than mothers. There have also been inconsistent findings in studies that have statistically compared mothers’ and fathers’ mean PSS:NICU scores. In the United Kingdom study by Franck et al. [11] and the Canadian study by Perehudoff [7], mothers were reported to experience more stress than fathers from the NICU environment. In contrast, for the USA study by Franck et al. [11] and the Canadian study by Shields-Poe and Pinelli [6], there were no significant differences in stress scores between mothers and fathers. A limitation with both Perehudoff [7] and Shields-Poe and Pinelli [6] were that the scoring method they used for the scale was not stated. Furthermore, fathers of NICU infants have been shown to play an important role in maintaining family stability during their infant’s admission [15, 16], which Levy-Shiff et al. [17] suggested is due to the mother and infant being in different hospitals, or the mother being physically incapacitated. In the present study, fathers experienced sights and sounds as the most stressful aspect of the unit, which was found in two previous studies [6, 7]. Fathers may not have been as prepared for this experience, compared to mothers, due to work commitments and staff being only available at certain times to orientate them to the unit. Other possible reason being that in developing countries more responsibility is on the male member of the family, it might be hard to juggle with the situation.Term birth was found significant in the sights and sounds domain. It appears that the traumatic experience of the term birth and the physical separation from the newborn upon NICU admission is sufficient to generate substantially elevated levels of stress before factors related to their infant’s illness severity may come into play. The present finding contradicts with other studies where preterm mothers were more stressed [12, 13, 15, 16], this difference could be as sepsis and asphyxia rate is high in developing countries hence mothers might be under tremendous stress with their normal weight babies being admitted in the hospital. Therefore, it is recommended that parents, particularly mothers with high risk pregnancies be provided with some explanations before labor in NICU during checking the neonatal intensive care unit. These explanations include the causes of devices alarms, rush of the staff, equipments and facilities of the unit, ventilators, intravenous tubes and monitors. This resonates with previous studies showing that parental trauma in the NICU is less related to infant characteristics than it is to alterations in their parental role [18].A study by Chourasia et al showed no statistical significance in three domains (infants’ behavior, parental role alteration, sights and sounds) in respect to education but in present study education was influenced in the staff behavior and communication domain [8]. Lesser educated and uneducated parents’ were found to have higher stress. This emphasizes that NICU parents are always under stress and they require special attention and specific NICU educational support. Assurance that the staff will communicate parents if the infant’s condition deteriorates may increase parents’ comfort when unable to be at the infant’s bedside, particularly at night. Provision of competent care in a calm and reassuring manner as well as clear communication and careful explanations geared to parental comprehension capability may reduce parental anxiety. Interventions addressing NICU parent stress, depression, and anxiety not only improve parents’ outcomes but infants’ outcomes as well [19, 20]. The strength of the present study was the evidence that fathers also experience stress with the NICU admission. Another, strength is that that the infants of parents sampled were representative of the diverse range admitted to NICUs. Parents were not excluded by way of their infant’s gestational age, birth weight, or type of medical condition. This study perhaps is the second Indian study pertaining to this important issue in a developing country similar to study done by Chourasia et al [8]. However, the present study also has a few limitations. The sample was a convenience sample and may not be representative of the population. Variation in time of administration of the PSS: NICU (24 hrs after admission in NICU) is another limitation because different events happen at particular times in the unit. More often, NICUs especially in the tertiary care centre in India have increased workload that health personnel including doctors and nurses find less time to focus on parental stressors in the NICU environment and give appropriate counseling to alleviate their anxiety. Finally, in consideration of the findings, it should be mentioned that this study was conducted in an open-bay NICU. Therefore, the results presented in this study might not generalize to other units with a private-suite design. It is possible that the social culture in open-bay units is more supportive due to parent-to-parent interactions, which may help in reducing stress levels. On the other hand, the increased privacy of individual rooms might make mothers feel more comfortable when spending time with their infant and consequently reduce parental stress. Future research is necessary to establish how differences in the NICU design influence parental stress levels.
5. Conclusions
- The health status of the infant might vary on a day-to-day basis and might affect parental stress to different degrees at different time points during their infant’s hospitalization. Stress levels upon NICU admission can therefore decrease or increase toward NICU discharge as parents gain a better understanding of the magnitude of their infant’s health status and the clinical implications of his/her illness. Identifying aspects of the babies, parents and the environment that can cause stress may be useful in assisting health personnel in understanding their importance and in improving the quality of care. Due to the mixed findings of previous studies regarding gender and maturity differences in experience of stress from the NICU, these differences found in the present study needs replication. Understanding parental stress may also help health personnel in assisting them towards improving their ability to meet the needs of their babies and to develop the skills required for fulfilling their role.
ACKNOWLEDGEMENTS
- We thank Dr. Raja Sriswan Mamidi, Scientist B, National Institute of Nutrition, Hyderabad for assistance with statistical analysis and for comments that greatly improved the manuscript.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML