-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Psychology and Behavioral Sciences
p-ISSN: 2163-1948 e-ISSN: 2163-1956
2016; 6(2): 58-62
doi:10.5923/j.ijpbs.20160602.04

Perception of Behavioral Issues: Exploring the Differences in Perception between Parents and Adolescents
Lesley A. Clack
Department of Health Sciences, Armstrong State University, Savannah, GA, United States
Correspondence to: Lesley A. Clack, Department of Health Sciences, Armstrong State University, Savannah, GA, United States.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

With the increasing prevalence of mental health disorders in children and adolescents, it is important to examine variables that may contribute to children not receiving mental health treatment. Differences in perception of behavioral issues between parents and adolescents may be a key determinant. The Problem Oriented Screening Instrument for Teenagers (POSIT) and Problem Oriented Screening Instrument for Parents (POSIP) were administered to 73 parent and adolescent pairs at a community mental health center. Paired T-tests were conducted for the 5 subscales measured on both the POSIT and POSIP surveys. Differences in scores between adolescents and parents were statistically significant on the Family Relations and Peer Relations subscales. Results indicate that there are significant gaps in perception of behavioral issues between parents and adolescents, particularly regarding peer and family conflict, and reducing those gaps may lead to improved treatment for children and adolescents.
Keywords: Children and adolescents, Behavioral issues, Perception, Parent-child relationship
Cite this paper: Lesley A. Clack, Perception of Behavioral Issues: Exploring the Differences in Perception between Parents and Adolescents, International Journal of Psychology and Behavioral Sciences, Vol. 6 No. 2, 2016, pp. 58-62. doi: 10.5923/j.ijpbs.20160602.04.
Article Outline
1. Introduction
- Parent-child relationships change significantly over the life span. Parents nurture, support, and guide their children’s development in the early years. As children become adolescents, the parent-child relationship changes and becomes a more equal and mutually supportive relationship [1, 2, 3]. This change in the parent-child relationship may be challenging for some parents and adolescents to attain. Due to the changes that occur in parent-child relationships during adolescence and the tensions that may arise, the perspectives of parents have rarely been sought. Therefore, little is known about parents’ perceptions of their relationships with their adolescents, and parents’ conceptions of their parenting role. [3]Most psychological theories of child development highlight the importance of family relations. According to previous studies, parents have a greater impact on adolescent health behaviors than previously thought. While peer influence is the major reason youth initiate negative behaviors, concern about parent disapproval is the primary reason that adolescents choose not to engage in negative behaviors. [4, 5]Little research is available regarding adolescents’ understanding of their mental health issues. Adolescents reportedly have limited ability in identifying mental health problems in individuals; And, according to prior studies, adolescents typically recommend that troubled individuals should seek help from family and friends, indicating that adolescents perceive parents and friends as the people to approach in a time of need. However, those studies have shown that parents’ ability to identify mental health problems in their adolescents varies depending on the nature and severity of the problem. [6-8]Sayal conducted a review of the literature in 2006 to examine parents’ perception of adolescent problems. The review found that although 20% of parents perceived that their child had an emotional or behavioral problem, only 4-6% of parents reported these to be worse than other children’s problems and only 16% believed that their child’s problem was severe enough to warrant treatment. [9] Symptom severity, level of impairment, presence of an externalizing disorder in the child, and mental health problems in the parent were identified to be strong predictors of parental perception of problems in adolescents. [8, 9]The purpose of the study was to examine the differences in perception of behavioral issues between adolescents and parents, with the hypothesis of the study being that there is a significant difference in perception between parents and adolescents. While a further understanding of adolescent perceptions is vital, parental perception of adolescent’s behavioral issues as a problem in need of treatment are also important predictors of mental health service use. Given that parents seem to be the main force behind adolescents receiving treatment, predictors of parental perception of mental health issues, and the significance of the differences between adolescent and parent perception, should be further examined. [10]
2. Methods
2.1. Participants
- Participants in the study were chosen from a community mental health center in Southwest Georgia. Administrative data was used to identify adolescents between the ages of 12 and 18 that were enrolled in child and adolescent mental health services at the study site during the study period. The inclusion criteria for study participation were: 1) an adolescent between the ages of 12 and 18 enrolled in child and adolescent services at the mental health agency at the time of the study, and 2) enrolled in mental health services for at least the past 3 months consecutively. Participants were excluded from the study if they had not lived with their current parent/guardian for at least 1 year consecutively, since that could impact the parent/guardian’s perception of adolescent’s issues. There were 398 children and adolescents enrolled in child and adolescent mental health services at the facility at the time of the study. Two hundred and ten adolescents met inclusionary criteria and were invited to participate in the study. Parents and adolescents were invited to participate in the study through an initial letter mailed to their home, and subsequent follow-ups during the 3 month study period. Only one parent/guardian for each child participated in the study. Seventy three adolescents (Mean age = 14.63, SD = 1.845) and seventy three parents/guardians (Mean age = 49.48, SD = 10.771) participated in the study, a response rate of 34.76%. Of the adolescents participating in the survey, 52.05% (n = 38) were male and 47.95% (n = 35) were female. The racial background of adolescents was 61.64% (n = 45) African American, 34.25% (n = 23) Caucasian, and 4.11% (n = 3) multiracial. The median education level was 8th grade.Of the parents participating in the survey, 13.70% (n = 10) were male and 86.30% were female. The racial background of parents was 67.12% (n = 49) African American and 32.88% (n = 24) Caucasian. The median education level was High School graduate or equivalent.
2.2. Instruments
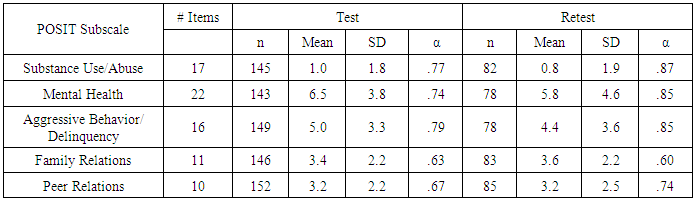
- The Problem Oriented Screening Instrument for Teenagers (POSIT) and the Problem Oriented Screening Instrument for Parents (POSIP) were used to measure differences in perception. The POSIT is a screening tool that was developed by the National Institutes of Health National Institute on Drug Abuse and was designed to identify problems and the potential need for mental health treatment in adolescents age 12 to 19. The internal consistency, test-retest reliability, and validity of each Subscale on the POSIT (see Table 1) have been measured in previous studies, and the survey has been proven to be a reliable tool for assessing adolescent issues. [11] The POSIP is the parental version of the POSIT. It was developed in 1991 by the National Institutes of Health, National Institute on Drug Abuse to determine the differences in perception of problem areas between the parent/guardian and the adolescent, and it can help determine a need for treatment. Differences in specific problem area scores indicate differences in perception of and/or reporting on those problem areas between the parent/guardian and adolescent.Both the POSIT and POSIP include questions over 5 functional areas: Substance Abuse/Use, Mental Health, Family Relations, Peer relations, and Aggressive Behavior / Delinquency. Under the scoring procedure of the POSIT, youth endorsing one or more of the items for each subscale are considered to be at a significant risk and should be recommended for further diagnostic assessment. [12]
|
2.3. Procedure
- Surveys were administered at the community mental health center. Consent was obtained from both parents and adolescents. Informed consent was obtained from parents and youth age 18, and assent was obtained from youth age 12 to 17, directly before administration of the survey. All participants also read and signed a HIPAA authorization form prior to the administration of the survey. The researcher was available to read the forms to any parent or adolescent if needed. Every effort was made by the researcher to ensure the privacy, confidentiality, and protection of research participants. IRB approval was obtained for the study. Surveys were administered to parents and adolescents separately. The researcher was available to answer any questions and/or to read the survey questions to participants if needed. Upon completion of the survey, each participant was given a $10 gift card as gratitude for their participation. Participants were also given copies of the signed consent / assent and HIPAA authorization forms. Surveys were administered after business hours to minimize distractions. Participants were given an unlimited amount of time to complete the survey. The average duration for each participant was approximately one hour. Once the survey and questionnaire were completed, the researcher checked for any missing data before the participants left the study site.
2.4. Analysis
- The differences in scores between parents and adolescents were compared for each group using a paired t-test. Descriptive statistics were derived for analysis. Statistical analyses were conducted using the Statistical Package for Social Sciences (SPSS), Version 21.0. Alpha and power levels were set at the traditional values for social science research (0.05; 0.8) with the goal of maintain good statistical power and statistical significance.
3. Results
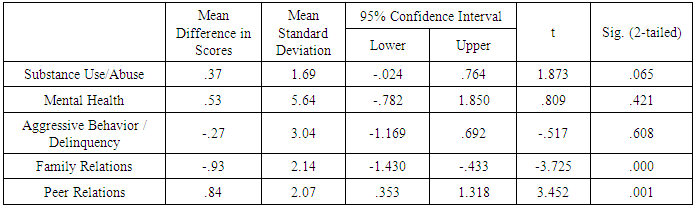
- There was a statistically significant difference in scores between adolescents and parents on the family relations subscale of the surveys. Adolescents reported fewer family relations issues with mean score of 6.48 (SD of 1.86). Parents reported greater family relations issues with mean score of 7.41 (SD of 1.61). In addition, there was a statistically significant difference between parents and adolescents on the peer relations subscale of the POSIT and POSIP. Adolescents reported greater peer relations problems with a mean score of 3.18 (SD of 1.66). Parents reported fewer peer relations problems with a mean score of 2.34 (SD of 1.36). Paired Samples Test Statistics for each Subscale are shown in Table 2. There was not a statistically significant difference in scores between adolescents and parents on the substance use/abuse (mean score of adolescents = 24.97, SD of 7.99; mean score of parents = 24.30, SD of 7.66), mental health (mean score of adolescents = 9.74, SD of 4.80; mean score of parents = 9.21, SD = 4.66), and aggressive behaviour / delinquency (mean score of adolescents = 5.18, SD of 2.75; mean score of parents = 5.45, SD of 3.36) subscales.
|
4. Discussion
- The results of this study revealed that adolescents reported less family conflict than did their parents. This is consistent with prior studies that have shown that parent report of family support differs from adolescent perception. This suggests that adolescent perception may be more predictive of their behavior than parent report. [13] Examining the effects of family conflict, especially on adolescents’ peer relationships, is particularly important since vulnerability is heightened during adolescence. Family conflict poses a social problem to the physical and psychological health and well-being of children, parents, and underlying family relationships and is a cause for concern. Adolescent’s behavioral, emotional, social, academic, and health problems are linked to inter-parental and parent-child conflict. [14]With regard to peer relations, adolescents reported greater conflict than their parents. Prior studies have also found that adolescents are more likely to report internalizing problems than parents. [15] Other studies have also shown that children’s social development and peer competence are influenced indirectly by the parent-child relationship. [16] Adolescents attempt to become independent and make the transition from depending on their family to relying more on their peers. In the adolescents’ struggle to establish a clear sense of their values, beliefs, relationships and independence, family conflicts may act as stressors that further affect their psychosocial adjustment. [19] The need to establish close, enduring emotional bonds with others in order to feel secure and explore the world with confidence is among the most important human needs. Theorists have been interested in the ways in which parental behavior might be related to children’s peer relations and have proposed that parents influence their children’s peer relations through the quality of the parent-child interactions. [20] Evidence suggests that the quality of peer attachment relationships that adolescents form is influenced by the quality of the attachment relationship established between adolescents and their parents. [21]Research has long-recognized the importance of the family for child and adolescent development. Relationships high in quality and low in conflict are associated with more positive outcomes for children, whereas relationships low in quality and high in conflict are linked to negative outcomes. Children exposed to family relationships marked by high conflict and low emotional support will likely display disruptions in their ability to control emotional and physiological responses to stressors. [22] Parents’ beliefs about the causes of their children’s problems may hinder mental health service use. A study conducted by Yeh et al in 2005 concluded that parents who believed that their child’s problems were due to physical causes or trauma were 1.56 times more likely to use mental health services compared with those who believed the problems were due to other causes, such as personality, relationships with friends and family, or family issues. [14, 23] The results of this study did not show any significant differences in perception of the subscales of mental health, substance use/abuse, and aggressive behavior/delinquency. This is consistent with other studies that have found a higher agreement between parent and adolescent perceptions when reporting externalizing symptoms than when reporting internalizing symptoms. [15]
5. Limitations
- There are several limitations worth noting. Adolescents may have been motivated to give answers that presented themselves in a favorable light or to have attempted to provide answers they felt would match that of their parents. Parents may have been motivated to give answers that downplayed their adolescent’s issues to present their children in a more positive light. Every effort was taken to attempt to reduce bias by having the researcher present to answer any questions the adolescents or parents had and to ensure the confidentiality of their responses. Participants may not have been fully aware of their reasons for any given answer because of lack of memory on the subject matter. Surveys with closed-ended questions may have a lower validity rate than other question types. Survey question answer options could lead to unclear data because certain answer options may be interpreted differently by respondents. Respondents may have answered “no” since the option “only once” was not available. The use of surveys assumes that self-report is valid. Researchers have long noted the extent to which individuals in clinical settings deny substance abuse involvement or exaggerate substance use behaviors. [24] The sample was convenient and purposive, which could limit the validity of its external generalizability. The results will only be generalizable to adolescents age 12 to 18 enrolled in a community mental health center with similar demographics of the study population. The researcher, data collector, and analyzer being the same person could pose a threat to external validity. However, the goal of the researcher was to minimize the influence of such factors. Historical and environmental events could be potential threats to internal validity for the study. Unrelated events may have occurred that affected the adolescents and parents, and therefore could have affected their responses to the survey questions. It was not possible to control for these unrelated events. They are random and do not affect the entire study population. Parents and adolescents may have been affected by environmental factors, such as distraction and the effect of being in a study, and these may have affected their responses.Parent perceptions of adolescents’ mental health issues were measured by only one parent’s perspective, and 86.30% of parent respondents were female. Future studies could examine parental dyads which would provide perceptions of adolescent mental health issues from both parents. Self-reporting is always a given limitation due to the influence of social desirability and human memory which can affect the accuracy of the data. Adolescents and parents may have been hesitant to indicate mental health issues. Additionally, this study was based on perceptions, which may change over time. The research design examines relationships rather than cause and effect associations. The mental health state of the parent is a limitation. Parent identification of adolescent’s mental health problems may be influenced by parents’ mental health problems and experience with the mental health service system. Parents with mental health problems may be less capable of recognizing their child’s needs, or they may be more aware of psychosocial symptoms which could positively influence the child’s access to mental health care. [25]
6. Conclusions
- This study has the potential to make significant contributions to the literature on perceptions of behavioral issues of adolescents by adolescents and their parents. Literature is needed regarding perceptions related to adolescent behavioral issues. The results of this study suggest that it may be helpful to utilize the studied questionnaires or similar questionnaires during treatment in order to gain information regarding parent and adolescent perceptions. Clinicians may be more likely to increase adolescents’ motivations for treatment if they elicit adolescents’ perspectives on their own mental health symptoms. Finding common treatment goals between adolescents and parents may be useful in increasing treatment retention. [26] Mental health treatment works and is a critical investment in the future of our youth.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML