-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Psychology and Behavioral Sciences
p-ISSN: 2163-1948 e-ISSN: 2163-1956
2015; 5(4): 143-147
doi:10.5923/j.ijpbs.20150504.01
Observing the Effects of Mindfulness-Based Meditation on Anxiety and Depression in Chronic Pain Patients
Kim ROD
Hons Life Science and Psychology, McMaster University
Correspondence to: Kim ROD, Hons Life Science and Psychology, McMaster University.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Background: People whose chronic pain limits their independence are especially likely to become anxious and depressed. Mindfulness training has shown promise for stress-related disorders. Methods: Chronic pain patients who complained of anxiety and depression and who scored higher than moderate in the Hamilton Depression Rating Scale (HDRS) and Hospital Anxiety and Depression Scale (HADS) as well as moderate in Quality of Life Scale (QOLS) were observed for eight weeks, three days a week for an hour of Mindfulness Meditation training with an hour daily home Mindfulness Meditation practice. Pain was evaluated on study entry and completion, and patients were given the Patients’ Global Impression of Change (PGIC) to score at the end of the training program. Results: Forty-seven (47) patients completed the Mindfulness Meditation Training program. Over the year-long observation, patients demonstrated noticeable improvement in depression, anxiety, pain, and global impression of change. Conclusions: Chronic pain patients who suffer with anxiety and depression may benefit from incorporating Mindfulness Meditation into their treatment plans.
Keywords: Mindfulness, Meditation, Chronic pain
Cite this paper: Kim ROD, Observing the Effects of Mindfulness-Based Meditation on Anxiety and Depression in Chronic Pain Patients, International Journal of Psychology and Behavioral Sciences, Vol. 5 No. 4, 2015, pp. 143-147. doi: 10.5923/j.ijpbs.20150504.01.
Article Outline
1. Introduction
- Chronic pain is pain that continues a month or more beyond the usual recovery period for an injury, illness, or pain that continues for months or years due to a chronic condition. The International Association for the Study of Pain (IASP) defines pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described by the patient in terms of such damage.” [1] The most common sources of chronic pain are low back problems, arthritis, cancer, repetitive stress injuries, shingles, headaches, and fibromyalgia. Other causes include diabetic neuropathy, phantom limb sensation, and other neurological conditions. Chronic pain can also exist with no apparent cause. [2] In the United States (US) alone, more than 100 million people suffer with chronic pain, costing the nation as much as $635 billion a year in medical treatment and lost productivity. [3]A 2006 survey conducted for the American Pain Foundation evaluated the impact that chronic pain had on 303 chronic pain sufferers who sought care from their physicians and were currently using an opioid to treat their pain. The Voices of Chronic Pain survey found that as a result of pain, more than three quarters of patients (77%) reported feeling depressed, 70% said they have trouble concentrating, and more than half (52%) said their chronic pain has put a strain on relationships with family and friends. More importantly, more than half of the respondents (51%) felt they had little or no control over their pain. [4] In fact, there is significant evidence of comorbidity for anxiety and depression related to chronic pain. [5]Depression often magnifies the pain and reduces patients’ coping skills. Mindfulness training─ the practice of maintaining a nonjudgmental state of heightened or complete awareness of one’s thoughts, emotions, or experiences on a moment-to-moment basis─has been shown to benefit both depression and substance use disorders. [6-12]Although still unclear, this approach may target common behavioral and neurobiological processes. [13-15] In addition to medications for chronic pain, non-medicinal therapies may help teach patients new self-management skills. Mindfulness meditation training has been adapted as a central component of psychotherapy and has shown some efficacy in the treating psychiatric disorders related or involving pain, anxiety, and depression. [17, 18] Dr. Jon Kabat-Zinn developed Mindfulness-Based Stress Reduction (MBSR), based on ancient healing practices, and is a well-defined and systematic patient-centered educational approach that is a relatively intensive training in mindfulness meditation. This core program teaches people how to take better care of themselves and live healthier lives. [19] Dr. Kabat-Zinn’s stress reduction program at the University of Massachusetts Medical School was used as a model for the following observation.
2. Materials and Methods
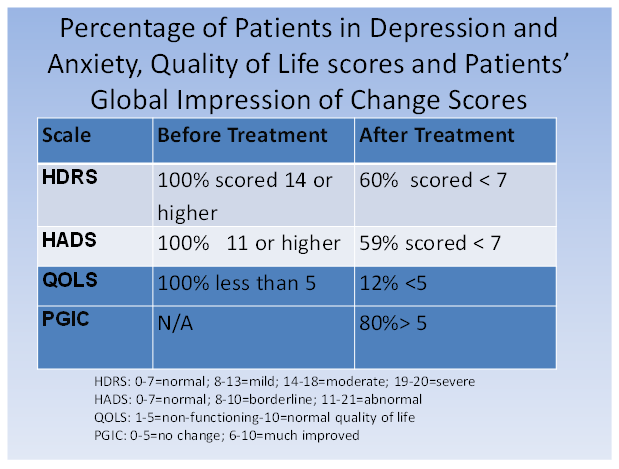
- To be included in the study, patients with chronic pain who complained of anxiety and depression had to score 14 or higher (0-7 = normal, 8-13 = mild depression, 14-18 = moderate depression. 19-20 = severe depression) on the Hamilton Depression Rating Scale (HDRS) [20]; 11 or higher (0-7 = normal levels of anxiety and depression (8-10 = borderline anxiety, 11-21 = abnormal anxiety and depression)on the Hospital Anxiety and Depression scale (HADS) [21]; and less than 5 (0 = non functioning –10 = normal) on the Quality of Life scale (QOLS). [22] On the Numeric Pain Rating Scale (NPRS), [23] 25% of study patients rated their pain as mild, 55% as moderate, and 20% as severe (0 = none; 1-3 = mild; 4-6 = moderate; 7-10 = severe). At the end of the study, patients were to complete the Patient’s Global Impression of Change Scale (PGIC) (0-4= very much worse to no worse, 5 = no change, 6-10 = better to very much better). [24] The baseline entering scores of the above mentioned scales as well as NPRS (Numeric Pain Rating Scale) numbers were recorded as baseline patient states.Patients were observed for eight weeks (3 days a week, one hour per visit along with one hour daily home practices on non-visit days). Mindfulness techniques included the following:● Mindful eating (eating with intention and attention to the sensations of eating like smell, taste, temperature and color)● Mindful breathing (focusing on each breath to become aware of sensations of breathing while aware of the mind’s tendency to jump from one thing to another)● Mindful body scan (being aware of the different body regions and experiencing each part’s sensations and feelings, without trying to change anything)● Mindful inquiry (exploring curiosity, not knowing, and trust through sequential inquiries) ● Mindful walking (being aware of the environment and one’s internal state, such as thoughts, feelings, sensations while walking and bringing awareness to the sensations of feet and legs)
3. Statistical Analysis
- The standardized questionnaires we used have group results as mild, moderate and severe based on 0-10, 0-20, 0-21 number categories or below or above 5 categories based on each specific questionnaire. Since there were 50 participants, any given number of participants belonging to any group (mild, moderate or severe) or below or above 5 represented a number group out of the total 50 patients. This number was translated into a percentage. For example if we had 3 patients who were severe in a group of 50, the number was translated into 6 out of 100 or 6%. The results of these standardized questionnaires are demonstrated based on percentage of patients belonging to each group of Mild, Moderate, Sever – Normal, Borderline, Abnormal – Nonfunctioning or Normal quality of life comparing before and after program results as well as below or above 5 in after program for patient global impression of change results.
4. Results
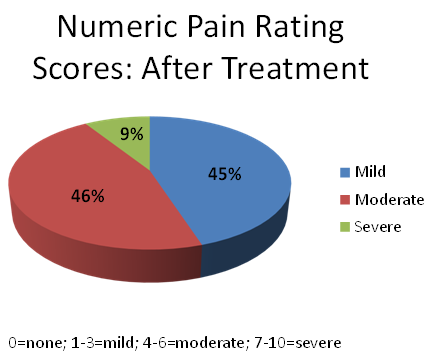
- During the year 2014, a total of 50 patients were enrolled in 10 programs; 47 patients completed the study. Three patients did not complete the study for personal reasons unrelated to the study on the last week of program. Their numbers were based on their answers at their exit points on the last week. Noticeable improvements were observed in patients’ depression, anxiety, and quality of life with this program. Patients also scored favorably on the PGIC. More importantly, the majority of patients were less depressed and anxious after Mindfulness training. On the HDRS, for example, 60% of patients scored in the “normal” range after training compared to 100% who scored in the moderate to severe depression range before treatment. On the HADS, 59% of patients scored normal (none-minimal or normal level of anxiety) after training compared to 100% who scored abnormal levels of anxiety before Mindfulness training (Figure 1).
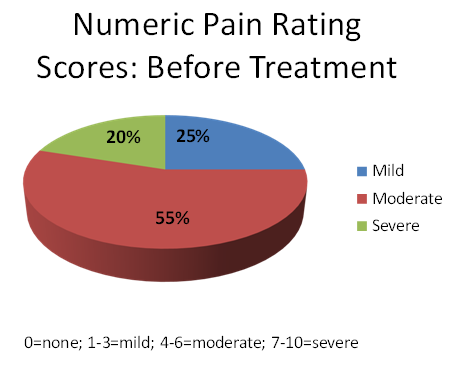 | Figure 2. Numeric Pain Rating Scale Scores before Treatment. 20% had severe pain, 55% Moderate pain and 25% mild pain |
5. Discussion
- Chronic pain, depression and anxiety can affect a person's entire life. Millions of Americans suffer with their pain, resulting in significant loss of productivity and income as well as negative impacts on their personal and family lives. Depression is one of the most common psychological issues facing people who suffer from chronic pain, and it often complicates the patient's conditions and treatment. Anxiety can significantly impair the quality of life in this patient population. Because of the connection between chronic pain, depression and anxiety, it makes practical sense that treatments for these conditions overlap. An ideal treatment approach addresses all the areas of patients’ lives that are affected by chronic pain as well as depression and anxiety. Mindfulness is a simple concept: pay attention to what’s happening in the moment, and when attention moves away, bring it back to the object of focus. The practice of mindfulness is to bring awareness to one’s present experience in a non-judgmental, non-reactive manner. This practice is based on releasing one from their negative past memories and future worries by bringing them to the awareness of the sensations, feelings and thoughts in the present moment. By focusing on the present moment, Mindfulness Meditation has shown promise as a component of addiction treatment. This training may also offer promise for those dealing with depression and anxiety that often accompany chronic pain. In mindfulness-based therapy, individuals focus on the bodily sensations that arise when they feel anxious. Instead of avoiding or withdrawing from these feelings, they remain present and fully experience the symptoms of anxiety as an observer. Instead of avoiding distressing thoughts, they open up to them in an effort to realize and acknowledge that the distressing thoughts are not literally true, observing them as they enter and exit their awareness. Mindfulness has been incorporated with cognitive therapy. There have been six randomized controlled trials of mindfulness-based cognitive treatment (MBCT) in people with a history of depression that, in aggregate, demonstrate that practicing this technique reduces the chances of another episode of depression by almost half. [25, 26] Two studies compared the efficacy of MBCT and gradual discontinuation of maintenance anti-depressants vs. continuation of antidepressants alone. The data showed no significant difference in the number of relapses between the two treatment options. The Kuykenstudy was notable for being conducted in primary care settings and for demonstrating that MBCT was superior for improving quality of life and comparable in cost. [26] MBCT also has been studied in generalized anxiety disorder (GAD), a disorder characterized by chronic worry and physiological hyper-arousal symptoms, panic, and social phobias. [27, 28] These studies have demonstrated significant improvement in anxiety symptoms with MBCT compared to control interventions such as psycho education groups or group-based cognitive therapy.Although Mindfulness meditation has met increasing interest as a therapeutic strategy for anxiety disorders, previous studies have been limited by methodological concerns, including a lack of an active comparison group. A recent study was the first randomized, controlled trial comparing a Mindfulness-Based Stress Reduction (MBSR) program with an active control for Generalized Anxiety Disorder. The results suggested that mindfulness meditation training, in the form of MBSR, can reduce anxiety symptoms in patients with GAD even when compared to an active control condition and is a treatment option worth pursuing in larger investigational trials. [29]In the present observational study, we evaluated the impact of Mindfulness Meditation on patients experiencing depression and anxiety associated with their chronic pain. The results are promising, suggesting that Mindfulness meditation training, including mindfulness of breathing, body scan, inquiry, walking, and eating, may improve levels of anxiety and depression as well as pain intensity.
6. Conclusions
- Our findings suggest that Mindfulness Meditation training is a positive approach for patients with chronic pain who are suffering with depression and anxiety, overall improving their quality of life and pain intensity.
ACKNOWLEDGMENTS
- We would like to thank the participants in this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML