-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Psychology and Behavioral Sciences
p-ISSN: 2163-1948 e-ISSN: 2163-1956
2013; 3(4): 86-94
doi:10.5923/j.ijpbs.20130304.02
Why Adolescents Begin and Stop Nonsuicidal Self-injury? A One-year Follow-up Study
Jianing You1, Min-Pei Lin2, Freedom Leung3
1Center for Studies of Psychological Application & School of Psychology, South China Normal University, Guangzhou, 510631, China
2Department of Educational Psychology and Counseling, National Taiwan Normal University, Taipei, Taiwan (R.O.C.)
3Department of Psychology, The Chinese University of Hong Kong, Hong Kong S.A. R., China
Correspondence to: Jianing You, Center for Studies of Psychological Application & School of Psychology, South China Normal University, Guangzhou, 510631, China.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
This study examined risk and protective factors for nonsuicidal self-injury (NSSI) among a large sample of Chinese community adolescents at two waves over a one-year follow-up period. We predicted the initiation and stop of NSSI by changes in various NSSI correlates in 4,782 school adolescents. Participants completed questionnaires assessing NSSI, emotional vulnerability, family invalidation, depressive symptoms, BPD features, unstable relationship, unstable sense of self, unstable mood, and behavioral impulsivity. Results showed that increases in depressive symptoms, unstable relationship, and behavioral impulsivity put adolescents at a significantly higher risk for future engagement in NSSI. On the other hand, decreases in depressive symptoms, hedonic impulsive behaviors and impulsive substance use made adolescents less likely to continue NSSI. This study indicated the importance of distinguishing risk factors from protective factors for NSSI among adolescents.
Keywords: Nonsuicidal Self-Injury, Risk Factors, Protective Factors, Adolescents
Cite this paper: Jianing You, Min-Pei Lin, Freedom Leung, Why Adolescents Begin and Stop Nonsuicidal Self-injury? A One-year Follow-up Study, International Journal of Psychology and Behavioral Sciences, Vol. 3 No. 4, 2013, pp. 86-94. doi: 10.5923/j.ijpbs.20130304.02.
Article Outline
1. Introduction
- Nonsuicidal self-injury (NSSI), the deliberate, direct, socially unacceptable destruction or alteration of body tissue that occurs in the absence of conscious suicidal intent[1], has become one of the leading public health problems among adolescents[2]. Adolescents seem to be the most vulnerable group for NSSI[3]. Conservative lifetime prevalence rates estimated that around 13-20% community adolescents have ever engaged in NSSI[4-8] and the 12-month prevalence rates ranged from 6-15%[9-11]. Nonsuicidal self-injury is perhaps the most robust and potent predictor of suicide attempt[12] and completed suicide[13]. Thus, NSSI among adolescents is in great need of research and clinical attention. A number of psychosocial correlates of NSSI have been identified among adolescents. These correlates included depressive and anxiety symptoms, anger outburst, low self-esteem, dissociative experience, disturbed family relationships, impulsivity, antisocial behaviors, smoking, drinking and substance abuse[4, 5, 7-9, 14-17]. It appears that these correlates fall into various domains of psychosocial functioning, indicating that NSSI is indicative of multiple underlying problems. The vast majority of previous NSSI research among adolescents was cross-sectional. These cross-sectional studies were significant to the extent that they provided a general picture of NSSI and its psychosocial correlates. However, they examined NSSI in a static perspective, and this snapshot approach may not provide much information for understanding the development and change of NSSI acts. Longitudinal studies would then be much desirable in this sense. Longitudinal studies of NSSI among adolescents have been accumulating in recent years. Yates, Tracy and Luthar[18] found among 245 school students that perceived parental criticism in Grades 6-8 significantly increased the likelihood of becoming a self-injurer in Grade 12, and parental alienation in Grades 9-11 fully mediated this relation. Among a large sample of secondary school students, situational risk factors (i.e. perceived family invalidation and depressive symptoms) were found to be significantly associated with the occurrence of NSSI over a 2-year period, and the maladaptive impulsive behavioral pattern contributed to both the occurrence and repetition of NSSI[19]. Among another large sample of community adolescents, You and Leung[20] demonstrated that relationship problems significantly predicted NSSI over a 6-month interval. Additionally, among 145 adolescent psychiatric inpatients, Guerry and Prinstein[21] found that higher levels of baseline depressive symptoms were associated with attenuated NSSI recovery during the first six months of follow-up. Individuals having a more negative attributional style and more stressful interpersonal life events at baseline tended to experience an increase in NSSI between 9 and 18 months post-baseline. All the longitudinal studies reviewed above explored the risk factors for adolescent NSSI using baseline variables as predictors. This method of over time prediction is useful in identifying adolescents who are at a high risk for later engagement in NSSI. However, these studies were limited to three important ways. First, given the fact that adolescents are at a period of rapid change in both psychological and behavioral domains, it seems to be of not much predicative utility to use variables measured one or two years before to predict behaviors emerged one or two years later. As an explicit behavior that is indicative of multiple underlying problems, NSSI among adolescents may appear or disappear as the internal disturbance exacerbates or alleviates. Thus, it seems to be of greater value to predict changes in NSSI acts by changes in the underlying psychosocial functioning. Second, most of the longitudinal studies examined only risk factors for NSSI; whereas they ignored protective factors which may prevent adolescents from repetitively engaging in NSSI. Protective factors, however, may be important for clinical intervention. Third, traditional longitudinal studies focus on changes in individual participants during a certain period of time. This approach, nevertheless, faces a problem especially when it is used among adolescents. That is, the interested change may not be induced by variables measured; rather, the change may be the consequences of increase in age or changes in overall environment. Thus, an alternative approach may be to compare two different groups of participants, who may undergo the same external environmental change during the same period. Of the two groups, one may remain stable in the research area and the other may change in that area. This method controls the effect of shared environmental change and allows researchers to examine the unique factors that contribute to changes in their interested area.The current study aimed to partly address these limitations. The major purpose of this study was to predict change in NSSI acts by changes in various psychosocial functioning among Chinese adolescents in a one-year follow-up study. To avoid theoretical biases, we included variables from various domains including affective, cognitive, interpersonal and behavioral domains. To explore risk factors for the engagement in NSSI, we compared one group of adolescents who had never engaged in NSSI during the testing period with another group of adolescents who became self-injurers at the second year of assessment. Similarly, to explore protective factors for NSSI, we compared one group of adolescents who repetitively engaged in NSSI in both years with another group of adolescents who stopped their NSSI acts at the second wave.
2. Method
2.1. Participants
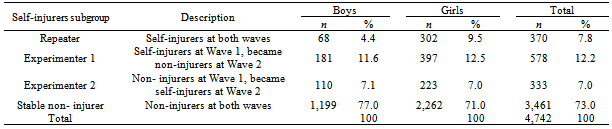
- This study is derived from a large-scale longitudinal study of borderline personality disorder (BPD) features among Chinese adolescents[22]. The sample comprised of adolescents from six secondary schools in Hong Kong. Four of these schools were coeducational (boys and girls), and the other two were girls-only. This resulted in more girl participants than boys. Given that NSSI are reported to be more prevalent among girls in previous studies[4, 7], over-sampling of girls would be desirable to yield greater numbers of those who had engaged in NSSI. Participants were surveyed yearly on 3 occasions. Data used in the present study were drawn from Year 2 and Year 3. To avoid potential confusion, we referred to Year 2 and Year 3 as Wave 1 and Wave 2 in this study. At Wave 1, a total of 6,212 adolescents, aged between 11 and 19 years (M = 14.56, SD = 1.81) were tested, and 68.5% (N = 4,253) of them were females. At Wave 2, a total of 6,421 students were tested and 67.6% (N = 4,342) of them were females. Among the Wave 1 sample, 4,782 participants were successfully followed at Wave 2. Of them, 67.1% (N = 3,210) were females. Attrition of the sample was mainly due to graduation or leaving of students.
2.2. Procedure
- We required written parental consent for student participation and followed standard data collection protocols approved by the Ethics in Human Research Committee of the Chinese University of Hong Kong. Participants completed the questionnaires in classrooms during a 45-minute period. Students absent from school on the day of the study were administered questionnaires later under the supervision of school personnel. The study was framed as a “Study of Emotion and Mental Health among Adolescents”. A unique ID number for each student was created for the data-matching purpose. Strict confidentiality of the study was emphasized. Only research personnel had access to the questionnaires. Because of the cooperation of the school authorities and their strong encouragement for their students to participate in the study, overall student participation rates were close to 99% for both Wave 1 and Wave 2 testing.
2.3. Measures
- Nonsuicidal self-injury (NSSI). At Wave 1, NSSI was assessed by three separate items. Participants rated the frequency of their NSSI behaviors under three different emotions, i.e., anger, sadness and anxiety. Possible responses ranged from 1 “never” to 5 “always”. Those who indicated engagement in NSSI in either one item were considered as self-injurers at Wave 1. At Wave 2, five specific types of NSSI behaviors were assessed using five separate items. These behaviors included self-cutting, burning, biting, punching and banging the head or other parts of the body towards the wall. These five behaviors were selected because they were the most common types of NSSI reported in past studies. Responses were made on a four-point scale, ranging from 1 “never”, 2 “once or twice”, 3 “three to five times” to 4 “six times or more”. Adolescents who indicated engagement in one or more types of NSSI were regarded as self-injurers at Wave 2.Based on participants’ reports of their NSSI acts in the two waves, participants were classified into four subgroups of NSSI: Repeaters, Experimenters 1, Experimenters 2 and Stable non- injurers. These four subgroups are defined in Table 1. Also included in Table 1 are the sample sizes and percentages of each subgroup for the total sample and separately by gender. Nearly three quarters of the total sample had never conducted NSSI during the two-year testing period. About 8% of participants were repetitive self-injurers, and girls tended to be more likely to continue their NSSI acts. The percentages of the two groups of experimenters, who performed NSSI at either one wave, were 12.2% and 7.0% for the total sample, respectively.Emotional vulnerability. The emotion vulnerability scale was a self-developed scale, assessing individual differences on three facets: sensitivity to emotional stimuli, emotional intensity and the time needed to return to emotional baseline. This scale was constructed based on the concept of emotional vulnerability proposed by Linehan’s[23]. It consists of 9 items assessing the three facets of three negative emotions: fear, anxiety and sadness. These three emotions all belong to the withdrawal emotional system. Items in this scale were: “I am easily to feel fear/anxiety/ sadness”, “When I am fearful/anxious/sad, the feeling is very intense” and “When I am fearful/anxious/sad, I need a long time to recover”. Exploratory factor analysis revealed a single factor structure. Participants were asked to rate the items on a five-point scale, ranging from 1 “not like me at all” to 5 “like me very much”. Higher score indicates higher degree of emotional vulnerability. This scale possessed good internal consistency in the present study, with its Cronbach’s alpha being .91 for the Wave 1 data, and .92 for the Wave 2 data.Family invalidation. The 18-item family invalidation scale was self-developed based on the concept of family invalidation proposed by Linehan[23]. Sample items included “I feel that my parents disrespect my opinions” and “When I communicate my feelings with my parents, they consider them wrong or inappropriate”. Responses were made on a 4-point scale, ranging from 1 “strongly disagree” to 4 “strongly agree”. Higher score indicates higher degree of family invalidation. This scale had a Cronbach’s alpha of .96 for both Wave 1 and Wave 2 data in this study.Depressive symptoms. The Chinese version of the Depression Subscale of Symptoms Checklist-90[SCL-90; 24] was used to measure depressive symptoms. The original scale consisted of 13 items. One item, “Loss of sexual interest or pleasure” was deleted in the present study as school authorities considered it not suitable for adolescents. Sample items for the present study were “Feeling low in energy/slowed down” and “Feelings of worthlessness”. Responses were made on a 5-point scale ranging from 1 “never” to 5 “always”. Higher scores indicate more depressive symptoms. This scale had a Cronbach’s alpha of .92 for Wave 1 data and .93 for Wave 2 data in this study. BPD features. The Chinese version of the McLean Screening Instrument for Borderline PersonalityDisorder[MSI-BPD; 25] was used to measure BPD features[26]. In the MSI-BPD, each BPD diagnostic criterion was assessed by one item, with the exception of the transient psychotic feature which was assessed by two separate items. Accord--ing to Zanarini et al., MSI-BPD had adequate one-week test-retest reliability (r =.72), good internal consistency (α =.74) and item-total correlation (ranged between .45 and .63). Since NSSI behaviors were assessed by additional items, we excluded the item assessing NSSI and suicide attempt in MSI-BPD, resulting in 9 items in MSI-BPD. In this study, participants rated their level of symptom severity on a four-point scale, i.e. 1 “strongly disagree”; 2 “disagree”; 3 “agree”; 4 “strongly agree”. Summation of the 9 item ratings gives a “dimensional score”. These 9 items had a Cronbach’s alpha of .86 for Wave 1 data, and .87 for Wave 2 data in this study.Unstable relationship. Five Items assessing unstable relationship were extracted and modified from the Revised Diagnostic Interview for Borderlines[DIB-R; 27]. Sample items were “I either love or hate other people in an extreme way” and “My relationships with other people are very unstable’. Responses were made on a 4-point scale, ranging from 1 “strongly disagree” to 4 “strongly agree”. Higher scores reflect more unstable relationships. It had a Cronbach’s alpha of .78 for Wave 1 data, and .80 for Wave 2 data.
|
3. Results
3.1. Demographic and Attrition Analyses
- The distribution of gender and family structure across the four NSSI subgroups was tested with chi-square analyses. For gender, χ2 (3, N = 4,742) = 40.79, p < .001. As shown in Table 1, girls were more likely to continue their NSSI acts. Boys, on the other hand, were more likely to never try NSSI. For family structure, χ2 (3, N = 4,693) = 21.52, p < .001, NSSI Repeaters were more likely to come from non-intact families than their counterparts from the other three subgroups.In attrition analyses, participants who stayed in the panel were compared with those who left the panel (attriters). Independent t tests showed that attriters scored significantly higher on almost all measures (except for the aggressive impulsive behaviors) than panel members, indicating that they possessed higher levels of emotional vulnerability, family invalidation, unstable relationship, unstable sense of self, unstable mood, depressive symptoms, BPD features, hedonic impulse and impulsive substance use. In addition, girls were more likely to be attriters, χ2 (3, N = 6,174) = 23.27, p < .001. Attriters and panel members did not differ on family structure. The fact that attriters were more disturbed in various domains than panel members suggests that we interpret the following results with caution.
3.2. Differences among Self-injurer Subgroups
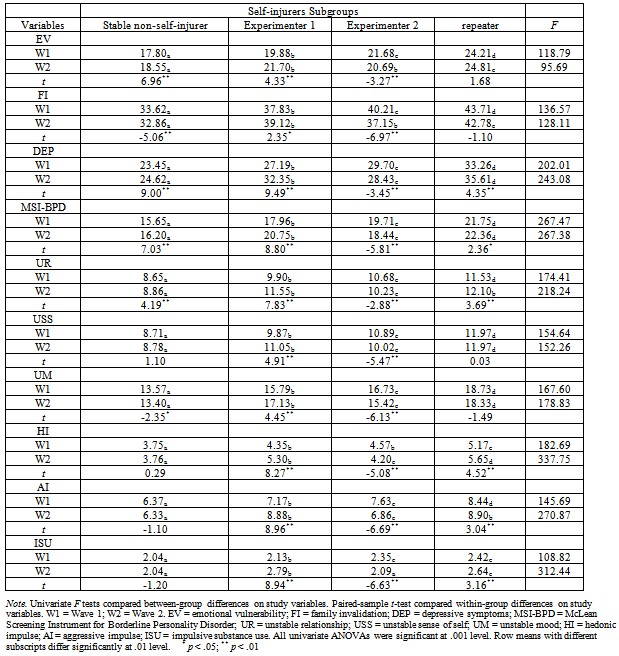
- We performed univariate analyses of variance (ANOVAs) to test whether the four self-injurer subgroups differed on study measures. Table 2 presents the means of all study variables in both waves for the four subgroups separately and the F statistics for each ANOVA. Post hoc analyses were performed using the Bonferroni method. Significant group differences were indicated by different subscripts in the table. All the study variables measured in both waves showed significant differences across the four NSSI subgroups. For all variables (except for impulsive substance use) measured at Wave 1, NSSI Repeaters scored the highest, followed by Experimenters 1 who performed NSSI at Wave 1 but stopped NSSI at Wave 2. These two groups scored similarly on impulsive substance use. Experimenters 2 who did not engage in NSSI at Wave 1 but conducted NSSI at Wave 2 scored in between Experimenters 1 and Stable non- injurers on most variables, but they did not differ significantly from Experimenters 1 on hedonic impulsive behavior. Stable non-injurers scored the lowest on all variables.For variables measured at Wave 2, NSSI Repeaters and Stable non-injurers again scored the highest and the lowest on almost all variables, respectively. Experimenters 2 were elevated and ranked behind NSSI Repeaters on most measures. They got similar scores with Repeaters on unstable relationship and aggressive impulsive behaviour, and even scored higher on impulsive substance use than Repeaters. Experimenters 1, on the other hand, improved in all domains and scored in between Experimenters 2 and Stable non- injurers on most variables, except that they did not differ significantly from Experimenters 2 on emotional vulnerability and family invalidation, and they scored similarly with Stable non-injurers on impulsive substance use.
|
3.3. Changes in Study Measures within NSSI Subgroups
- To test changes in all study measures within each NSSI subgroup, paired sample t tests were performed with Wave 1 and Wave 2 variables for each NSSI subgroup. Results are also shown in Table 2. To our most interest, Experimenters 1 improved significantly in all domains from Wave 1 to Wave 2; Experimenters 2, on the other hand, deteriorated on all variables. This indicates that initiation in NSSI was accompanied with deterioration in multiple domains. In addition, Repeaters experienced more depressive and BPD symptoms, suffered more unstable relationship, and possessed higher levels of hedonic and aggressive impulse,as well as impulsive substance use at Wave 2 than at Wave 1.
3.4. Predicting Changes in Self-injurer Status by Changes in Study Variables
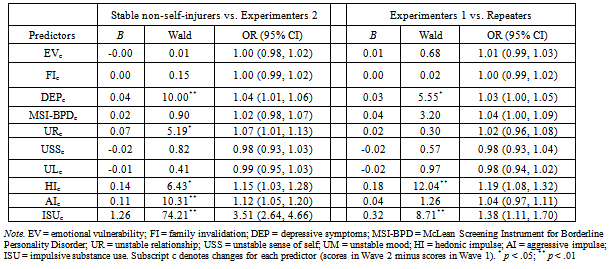
- To examine changes in which variables could successfully predict changes in NSSI status, multivariate logistic regression analyses were performed, with the change scores of each variable as the predictors. The change score for each variable were computed by subtracting its Wave 1 score from its Wave 2 score. Two pairwise comparisons were considered: (a) Stable non- injurers versus Experimenters 2; and (b) Experimenters 1 versus Repeaters. Findings are summarized in Table 3, showing regression coefficients, Wald statistics, odds ratios (OR), and 95% confidence intervals for odds ratios (95% CI) for each predictor.
3.4.1. Stable non-injurers versus Experimenters 2
- This logistic regression examined changes in which variables put adolescents at a higher risk for engaging in NSSI. A test of the full model with all predictors against a constant-only model was statistically significant, χ2 (10, N = 4,782) = 273.77, p < .001, indicating that the predictors, as a set, reliably distinguished between Stable non-injurers and Experimenters 2. As for individual predictors, changes in depressive symptoms (OR = 1.04, 95% CI = 1.01-1.06), unstable relationship (OR = 1.07, 95% CI = 1.01-1.13), hedonic impulsive behavior (OR = 1.15, 95% CI = 1.03-1.28), aggressive impulsive behavior (OR = 1.12, 95% CI = 1.05-1.20), and impulsive substance use (OR = 3.51, 95% CI = 2.64-4.66) were predicative of later engagement in NSSI. As indicated by the magnitude of odd ratios, change in impulsive substance use was the strongest predictor. Those who increase their substance use by 1 unit were 3.5 times as likely to engage in NSSI as those who remained their level of substance use.
3.4.2. Experimenters 1 versus Repeaters
- This logistic regression analysis examined changes in which variables protected adolescents against continued NSSI acts. The full model with all predictors was significant, χ2 (10, N = 4,782) = 81.38, p < .001. Changes in depressive symptoms (OR = 1.03, 95% CI = 1.00-1.05), hedonic impulsive behavior (OR = 1.19, 95% CI = 1.08-1.32) and impulsive substance use (OR = 1.38, 95% CI = 1.11-1.70) were statistically significant. Change in impulsive substance use was again the strongest predictor. Those who decreased their substance use by 1 unit were 38% more likely to restrain from continued engagement in NSSI than those who remained their level of impulsive substance use.
4. Discussion
- In this research, we followed a large sample of Chinese community adolescents and examined the patterns of their NSSI use over a 2-year period. We classified adolescents into four subgroups according to their NSSI use over time: a) Repeaters (i.e. those who reported engagement in NSSI in both waves of assessment); b) Experimenters 1 (i.e. those who reported engagement in NSSI in Wave 1 but not in Wave 2); c) Experimenters 2 (i.e. those who reported engagement in NSSI in Wave 2 but not in Wave 1); and d) Stable non-injurers (those who reported no NSSI in both waves of assessment). This study revealed significant between - group differences on various NSSI - related variables, as well as within-group differences across the two waves of assessment. Among changes of all study variables from Wave 1 to Wave 2, we also identified significant predictors for changes of NSSI use.
4.1. Prevalence of NSSI at the Two Waves of Assessment
- In the present sample, more than one fourth of adolescents have engaged in NSSI in a two-year period, indicating that this phenomenon is not uncommon among Chinese adolescents. For the total participants, about 8% of them continued their NSSI acts throughout the two years, with girls being more than twofold as likely to be repeated self-injurers as boys. This gender difference indicates that girls may suffer longer and more severe disturbance than boys. Boys, on the other hand, were less likely to conduct NSSI repeatedly.
|
4.2. Between-group Differences on Study Variables
- Comparing among the four NSSI subgroups, our results suggest that repetitive self-injurers were the most disturbed group. They continuingly suffered the worst psychosocial functioning during the 2-year assessment period, indicating that the underlying disturbance of NSSI repeaters may be chronic and somewhat uncontrollable. These individuals may have no other ways to deal with their problems and consider NSSI as their final solution. Both groups of experimenters, on the other hand, suffered less serious problems than repeaters in most domains even at the testing wave they conducted NSSI. In addition, one group of experimenters experienced a higher level of extensive psychosocial disturbance during the period they engaged in NSSI than the other group of experimenters who did not conduct NSSI at that time. This indicates that engagement in NSSI was largely due to situational factors at that time. This result furthers our understanding of NSSI that adolescents’ NSSI acts may vary with the level of their psychosocial functioning.
4.3. Predicting Self-injurers Status Change by Changes in Study Variables
4.3.1. Risk Factors for NSSI
- Our results showed that deteriorations in depressive symptoms and interpersonal relationship, more hedonistic and aggressive impulsive behaviors, and more substance use were significant risk factors for the engagement in NSSI. This is consistent with some previous cross-sectional studies which also found associations between these variables and NSSI (e.g., Ross & Health, 2002; You & Leung, 2012; You et al., 2012). The unique contribution of the present study is that although engagement in NSSI was associated with changes in multiple psychosocial functioning, only changes in depressive symptoms, interpersonal relationships, and impulsive behaviors were deciding factors for adolescents’ change from non-self-injurers to self-injurers. In particular, the change in impulsive substance use was the most potent predictor. For non-self-injurers starting to engage in NSSI, the odds for those who drank more and took more drugs were several times higher than that for those who remained their substance use level. It is possible that alcohol and other illicit drugs impaired the functioning of the prefrontal cortex, which is responsible for problem solving, decision making and impulse control. Thus, increasing substance use lowers adolescents’ coping ability and disinhibits theirinappropriate impulse, both of which may make adolescents more prone to use maladaptive coping behavior, such as NSSI, to deal with their problems.
4.3.2. Protective factors for NSSI
- Similar as the risk factors for NSSI, protective factors that kept adolescents from repetitively engaging in NSSI were less depressive symptoms, hedonistic impulsive behaviors and substance use. Less interpersonal problems andaggressive behaviors would not make self - injurers discontinue their NSSI acts. Therefore, changes in depressive symptoms, hedonistic impulsive behaviors and impulsive substance use were consistent predictors of NSSI behavior change.
4.4. Strengths and Limitations of the Present Study
- There were several strengths of this study. One was the large sample size which maked our results quite reliable. Another important strength was the use of a longitudinal design, which allowed us to examine the change of NSSI behaviors and associated changes in psychosocialadjustment. To our knowledge, the present study was the first one to investigate NSSI behavior in the perspective of change, and the results broadened our understanding of the risk factors and protective factors for NSSI. Limitations included a limited sample of school adolescents only, which restricted the generalizability of our results. In addition, we used different methods to assess NSSI at the two waves, which might lead to variation in the reported rate of NSSI. Finally, we followed NSSI acts of the sample for only 2 years. A longer period of observation may be more desirable.
4.5. Implications
- This study has important implications for future research and practice. The finding that increase in substance use was the most powerful predictor for the transition from non – self - injurers to self-injurers emphasizes the importance of closely attending to adolescents’ substance use level, because alcohol and other drugs will not only do harm to adolescents’ physical health, but are also tied to other psychosocial morbidity, e.g., increased risk of NSSI. In addition, this study suggests that girls are more likely to continue their NSSI behavior. Parents and school authorities may thus pay more attention to girls’ mental health.
5. Conclusions
- The present study examined risk and protective factors for adolescent NSSI using a longitudinal design. Depressive symptoms, unstable relationship, and behavioral impulsivity were significant risk factors which put adolescents at a higher risk for future NSSI, while decreases in depressive symptoms, hedonic impulsive behaviors and impulsive substance use were protective factors which decreased or stopped adolescents’ NSSI. This study suggests that engagement in NSSI may co-vary with the experience of emotional problems and/or engagement in other impulsive behaviours.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML