-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Information Science
p-ISSN: 2163-1921 e-ISSN: 2163-193X
2013; 3(3): 70-79
doi:10.5923/j.ijis.20130303.04
Conceptualising the Future of Health Informatics: A Discussion
Said Shahtahmasebi1, 2, 3, Renee Millar4
1Director of Research, the Good Life Research Centre Trust, Rangiora, New Zealand
2Voluntary Faculty, Division of Adolescent Medicine, University of Kentucky
3Centre for Health and Social practice, WINTEC, Private Bag 3036, Waikato Mail Centre, Hamilton 3240, New Zealand
4Centre for Health and Social practice, WINTEC, Hamilton, New Zealand
Correspondence to: Said Shahtahmasebi, Director of Research, the Good Life Research Centre Trust, Rangiora, New Zealand.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
This manuscript is a discussion paper highlighting the information dimension of health “informatics”. Health informatics is now a discipline in its own right with many academic institutions establishing health informatics research centres/units and offering qualifications in health informatics. The vast and rapid advancements in information and communications technology (ICT) have considerably improved data storage and access to data. The advancements have also led to a culture that considers technological products as “solutions”. The downside of this culture is that the focus on “solutions” has shifted attention away from the main component of informatics: information. The current health informatics movements (such as e-records and e-health) are focussed on the management of clinical data overlooking data from primary healthcare and non-patient or non-clinical data source. Part of the problem is that information systems do not always communicate with each other. This paper raises the question “what constitutes information?” and argues that attention must be refocused onto access to health information over and above access to clinical data, and proposes a conceptual model to improve access to health information.
Keywords: Databases, ICT, E-Records, Local Knowledge, Evidence-Based Practice, Public Health
Cite this paper: Said Shahtahmasebi, Renee Millar, Conceptualising the Future of Health Informatics: A Discussion, International Journal of Information Science, Vol. 3 No. 3, 2013, pp. 70-79. doi: 10.5923/j.ijis.20130303.04.
Article Outline
1. Introduction
- A proactive health care system provides health care not only at the point of intervention, but also well before intervention is required so that it either eliminate or delays the need for medical and possibly expensive intervention. Whilst medical interventions respond to an event that has already occurred, i.e. treating ill-health, the preventative activities must be based on knowledge and information about human behaviour and its environment to understand the process of ill-health development. Therefore, medical interventions are heavily based on clinical data which are necessary to develop appropriate treatments. This distinction has often been likened to the dynamics of a swiftly flowing river where intervention is downstream activity, i.e. continuously jumping in the river and saving drowning people, and preventative is upstream activity, i.e. understanding how and why people are drowning. Most health service research are downstream, therefore, do not add insight into our understanding of upstream dynamics[1]. In addition to downstream (clinical) information, appropriate upstream (non-clinical) information is required to inform the process of health service policy development.Information is the main currency within the health service industry. Health informatics is essentially the identification, collection and management of data items that may inform the process of health care planning and delivery. The massive and rapid progress in technology promised a bright future for informatics in terms of not only data management but also generating knowledge from data. Unfortunately, within the computing/technology and informatics community, the technological progress, in terms of products and gadgets, is often referred to as “solutions” which has made informatics technology led rather than human behaviour led. Therefore, often increasing data transfer speed, storage capabilities, access to data is quoted as the main feature of an informatics system. In contrast very little has changed since the paper-based information systems in terms of access to meaningful information. The question that arises is whether health care systems are keeping up with what technological advancements can offer in order to meet the complex dynamics of human behaviour in terms of public health needs[2]. Health informatics may be considered as a combination of many disciplines such as computer science (hardware and software), health science, telecommunication, information science and management, health economics, and statistics. The aim is, of course, to identify, collect, manage and process appropriate data to inform the process of health care planning and delivery. As a result, health informatics has grown and become a major field in its own right with most major universities offering post-graduate qualifications and a research career in health informatics. However, the emphasis has shifted to technological, clinical data, and the administration aspects of health informatics. The purpose of this paper is to conceptualise a human behavior-led technological application for health informatics, as opposed to “solution”-led applications. In doing so, we argue that health informatics is more than about learning and teaching how to use new technologies. Furthermore, we discuss that, over and above data collection and storage, the role of informatics is to inform.
2. Background
- Like any other business, the health sector relies heavily on information for its operations; from a government’s fund allocation to the distribution of resources, to health care service development and interventional programmes. Morbidity and mortality statistics have been used for these purposes. Data items such as age, sex, post code, diagnosis, treatment, patient’s outcome, and cause of death are routinely collected and are available through patients’ records.As health care systems have become more and more complex, and in order to respond to all the ill-health needs of its population, some scholars began to equate resources with rising demand and inequalities in health. Health statisticians and health professionals need to refocus, to investigate the largely unmapped terrain upstream[1], particularly in solving the problem of differential class experiences of health[3-5].In an earlier paper, Shahtahmasebi[6] argued that despite the attempts to research and map upstream, health services still rely heavily on downstream research, thus building up information systems consisting of data collected after the event i.e. incidence of an illness which necessitated a consultation with a health service professional. The principle of collecting data on morbidity and mortality, in order to plan for the health needs of the population has inevitably led to a ‘reactive’ health care system. In other words, a health informatics based on clinical data will inappropriately re-define the health needs of the population in terms of number and the nature of interventions required per financial year. Vast improvements in ICT has enabled large volumes of digital information from medical images to large databases/spreadsheets to be shared through high speed broadband modems. In New Zealand, data sharing appears to be patchy and dependent upon health care provider’s information systems and networks[7]. For example, some patients’ hospital records such as x-rays or specialists consultation notes may be visible to the patients’ primary care providers (GP) depending on the area, and district health board. A recent study confirms the incompatibility of information systems across the health sector[8]. On the other hand, health outcomes have been linked to other social, educational and economic outcomes[3-6, 9, 10]. In the context of government policy the UK government acknowledged the link between socio-economic factors, e.g. employment status, and health outcomes in the UK’s mental health strategy[11]. The main issue is how the policy statement of a causal relationship between poverty and mental health outcomes will be translated into relevant and appropriate policy actions? The public, social and political sectors responsible for policy development, implementation and monitoring social, educational and economic outcomes have their own information systems that are likely to be incompatible with those of the health sector. For health informatics to effectively inform health care planning and delivery, it should be able to communicate with the other sectors over and above multi-disciplinary research activities. Although technology is sufficiently advanced to create a unified database most of the efforts in translating access to information have concentrated on access to clinical information. For example, the apparent recommendation and development of e-records by various governments such as the UK, Australia, USA, New Zealand and Canada will ultimately lead to e-health[7]. In the UK e-records are already in use and a campaign is being carried out by the respective agencies to win public opinion through (i) emphasising the advantages of e-records over current information systems, (ii) by providing the public with a choice as whether or not they would like to have an e-record, and (iii) by reassuring the public about security measures to maintain their privacy (see www.nhscarerecords.nhs.uk). In New Zealand, the government has begun public consultations about the introduction of “Shared Care Records” (SCR) http://www.sharedcareplan.co.nz/. The SCR may be a type of electronic patient’s record initially starting with people with long-term conditions and mothers and new born babies. Both the UK’s e-records and New Zealand’s SCRs collect important clinical information that may be accessed by all the stakeholders involved in the provision of care of an individual. The creation of e-records, where important information such as medication history, diagnoses, and allergies are stored for common access is still a downstream philosophy and a reinvention of the wheel.
3. Discussion
- It is argued that the rapid rise in the status of health informatics has coincided with rapid advances in computer and telecommunication technologies. Therefore, in this paper we will not dwell upon the issues that are directly relevant to the development of the technology, but instead focus on the issues that are relevant to the utilisation of the technology. It seems to us that there are two major issues remaining: the appropriate and innovative applications of ICT, and information itself.Technological advancements have led to an increasing number of ICT applications within the health sector from automated patient monitoring systems to the storage and retrieval of patients’ records, virtual lecture theatres, and the application of artificial intelligence (AI) in intelligent information systems e.g. see Buchan[12]. It is not surprising that a joint universities report in New Zealand[13] reported that the New Zealand Government health information strategy was to increase the utilisation of ICTs to improve health care delivery but the strategy appeared to ignore the implications for the skill-based workforce that is needed to implement the strategy. One of the report’s recommendations was for the Government to invest more in health informatics education. As suggested earlier, most educational establishments in New Zealand offer postgraduate diplomas in health informatics e.g. see http://www.hien.otago.ac.nz/index.php?cat=about&page=home. However, such diplomas are designed to bring students up to speed with the ICT applications currently in use in the health sector so that they can play a role in their respective organisations or enable them to seek employment in the health informatics industry. Yet again, a downstream philosophy.Beyond the basics of record keeping, the applications of health informatics have extended to patient care e.g. automated patient monitoring systems; distant care delivery e.g. telemedicine; education and training e.g. telemedicine; virtual classroom[14, 15]; management e.g. hospital records; medical warning systems (MWS), and so on. One of the main issues is that information systems are not connected and do not communicate with each other (http://www.healthnavigator.org.nz/centre-for-clinical-excellence/national-shared-care-plan-programme/). To resolve the issue of non-compatibility, recent decades have witnessed some central strategic planning and implementation of e-records, e.g. in the UK (www.nhscarerecords.nhs.uk) and “Shared Care Record” (SCR) in New Zealand http://www.sharedcareplan.co.nz/. These ideas are marketed in terms of usefulness of access to patients’ records anywhere and anytime and by health professionals who are involved with the care of a patient. The e-records provide a summary of important patient’s (clinical) data such as allergies, diagnoses and medication history. These activities and utilisation of “solutions” are clinical based and are only appropriate for administration of medical interventions. Clinical data does not lend itself to study ‘health’ and inform health care planning. A study of international comparison of health care systems[16] suggests a good but varying degree of international utilisation of ICT in the health sector but raises the question whether data from e-records may necessarily produce quality information to inform, in particular, primary health care service development. Therefore, these information systems should be referred to as ill-health or patient or clinical informatics rather than health informatics.In the past, a number of databases such as the census and a geographical information system (GIS) e.g. see[2, 17-19] have been linked with patients’ records to study the effect of socio-economic factors on health outcomes. Buchan[12] proposes a model to improve access to health data from a variety of sources. Nevertheless, such practice is still dependent on data after the event, non-linked longitudinal aggregated data and only provides a snapshot of socio-economic characteristics of residential areas. There is very little in health records to inform our understanding of disease development – information which is necessary to plan an effective health care system.
3.1. Information
- International comparisons[16] suggests that New Zealand is the biggest relative spender on administration and insurance – but is also one of the best users of information technology computerisation: ‘in New Zealand it is easier to phone the GPs clinic, we are the best at getting information between clinics, hospitals and patients in good time, getting reminders out about cancer checks, and our other mechanisms co-ordinating services across different parts of the system are among the best.’ Clearly, digitising data and automating the administration of health care using information systems has some benefits in providing timely health care services. However, health care information systems require more than administrative data if they are to improve access to information by health care professionals, and, to inform the process of health care planning in order to reduce morbidity and mortality and to improve quality of life[6, 9, 20-25]. Despite a complex ill-health informatics, as the report also suggests[16], New Zealand’s preventative health care and outcomes are relatively poor e.g. chronic conditions such as high blood pressure, high mortality rates (that can be prevented), and high infant deaths. Recently, attention has focused on electronic patients’ records (e-records). This attention is in line with the concept of computerisation of data for administrative purposes e.g. administering clinical care. For example the UK’s health e-records will initially maintain summary care records containing important patient details such as test results, diagnoses, allergies, prescription and medication history (www.nhscarerecords.nhs.uk). Over time these records may be updated every time a patient uses any health care services. A summary record is created once an individual has given consent and this record will be accessible by any health professional who is directly involved in providing care for the individual. The usefulness of such an e-record system is pointed out (www.nhscarerecords.nhs.uk) in terms of access to information ‘at the point of delivery’ and generally in situations where the care provider is not the patient’s own GP: when a patient is away in another part of the country, in accidents and emergency departments or when ambulance services are called out. Similarly, the New Zealand government is introducing the “Shared Care Record” (SCR) http://www.sharedcareplan.co.nz/. The emphasis is on patients’ access and, to some extent, ownership of their own data. This approach will raise more problems than it pertains to solve. For example, the system could potentially allow patients to password protect data items on the SCRs. Such behaviour will defeat the objectives for which shared records are being introduced, i.e. improved care through the health care professional’s access to important patient data at the point of delivery of care.Once again the idea of e-records may appear innovative and in line with improving access to information, however, in the light of the high utilisation of ICT and the computerisation of information systems, e-records may be seen as a re-invention of the wheel. In other words most patient records are already available in a digitised format in a database and (ignoring the economics of it) e-records provide another storage facility with the promise of more access conditional upon patient’s consent. We strongly believe that the technology is advanced enough and is no longer a main issue. The main issue is to decide whether we want a ‘health’ informatics system or a series of ‘ill-health’ database systems. The former can be conceptualised and realised with only a fraction of the costs associated with e-records.
3.2. The Role of Midwifery Informatics
- Most nations, in addition to morbidity and mortality data, collect birth and child development data through nursing services. The difference between different countries is very broadly the continuity in the data and the extent of computerisation. In New Zealand, data may be available in electronic format and also in paper trails. An individual’s health record begins at birth with a unique health ID. In New Zealand, the current process of capturing data during pregnancy involves a number of agencies. The woman (client) may go to a midwife or GP to have her pregnancy confirmed or may do a home pregnancy test. She then chooses a lead maternity carer (LMC), i.e. midwife, GP or Obstetrician. The LMC registers the client with Healthpak (Ministry of Health maternity funding department). The registration form may also be sent to the district health board (DHB) facility, depending on the individual practitioner and the policies of their DHB. Clinical charts may be held by the birthing facility the client is booked into, and some electronic data may be entered on the DHB system. For statistics and payment purposes electronic data are entered through the midwifery and maternity provider organization (MMPO) depending on the system of practice management used by the LMC. Some LMC’s claim directly to Healthpak either online or through the use of paper forms. Others have an arrangement with a maternity facility to provide claiming services for them. Throughout the pregnancy, information is recorded and updated via the chosen method. Referrals may be made to radiology services, laboratory, physiotherapy, mental health services, sexual health services, or other specialist as required, e.g. obstetrician (private or public) who then maintain their own record of information on the client. Women are also enrolled with a primary health organisation (PHO) via their GP. Some systems may be compatible, enabling the easy transfer of information from one caregiver to another. Some labour and birth information may be held by the birth facility. Labour and birth information is sent to the provider organization electronically and/or in paper form. Information about the baby is sent (usually faxed) to birth registrations NZ. The LMC is required to provide the newborn’s details to NIR (National Immunisation Register). In other words, newborns are automatically enrolled in the system without requiring parental consent. However, the NIR provides the option of opting out, i.e. parents can apply to have the child’s information removed from the register. The client and baby are discharged from LMC care prior to six weeks post birth and care is then transferred back to the GP and to the chosen Well Child Provider if the parents consent to this. The immunisation programme is usually commenced at six weeks of age by the GP. Some babies are vaccinated at birth by midwives/nurses if required. Schools and other institutions e.g. hospital emergency departments also provide opportunity for immunisation but records are not always forwarded to the GP or PHO leaving potential for missed care or immunisations being done twice. GP’s cannot access the information from NIR online. They have to phone to request information but often need to leave a message and it may take several days before it can be followed up. Even in New Zealand which has a lead on the utilisation of ICT in the health sector, communication between health practitioners is still paper based.However, during pregnancy and child birth and subsequent child development the system appears to be amassing life history data on individuals, albeit in a fragmented and multi-medium format. These data are potentially health informatics and have been ignored for decades.
3.3. The Role of Nursing Informatics
- In New Zealand, similar to the UK, midwives hand over duties to Plunket nurses (health visitors). Plunkets and health visitors make regular visits to the families for monitoring purposes and collect observations on mother and baby and the family environment. These visits are not for medical or clinical reasons and monitoring and non-clinic observations may be describing life processes. The Plunket hands over its duties to the School Nurse once the child enters primary school. The GP and primary care services provide for the medical needs of the mother and baby whilst in the community. Once again Plunkets and health visitors and school nurses could potentially be holding a valuable mine of historical health data which have been overlooked yet again[26]. Over the last three decades or so nursing informatics has developed into a specialty within the nursing profession and some claim it has helped advance the art of nursing into the science of nursing[27]. Nursing informatics may be viewed as the application of ICT in storing and communicating nursing data with particular reference to the clinical setting. For example, automated patient monitoring systems collect data such as blood pressure, pulse, temperature, and send warning signals to nurses e.g. seehttp://www.nursing-informatics.com/revealing/power.html. However, the application of nursing informatics goes beyond bedside care, and administration. Anotherapplication is telemedicine/telenursing[28]. The advancement in technology, including mobile technology and palmtops capable of receiving graphics and super fast broadband capable of transferring large amounts of data such as images, x-rays, means improved telenursing. Over and above rapid access to data, nursing informatics is, in essence, still a downstream philosophy and activity, and therefore, it presents all the issues raised above. In other words, in the community and primary care sector nursing data is still fragmented and does not lend itself to be shared in a fast and efficient way, and, does not inform our understanding of the process of disease development. Nursing informatics can contribute to the development of a unified database and also benefit from it to inform the process of nursing care policy development.
3.4. Conceptualising a Unified Database
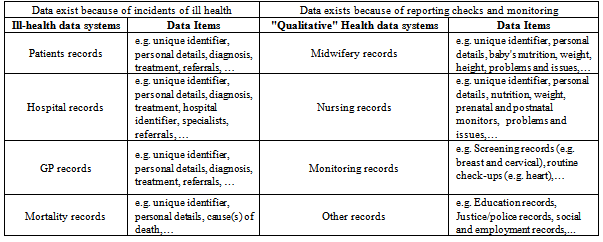
- Table 1 provides an example of routinely collected data that, if complete, can provide upstream data. Together, the data collection systems have the potential to provide life event histories for any individual. The major issue here is that these data collection systems are not linked and do not communicate with each other. It is possible that data collection systems are often purpose-built and designed independently. Nevertheless, most data systems will have a common unique individual identifier(s) that can be used to link data systems together. In an ideal world databases would have been part of the same design and by default would have been linked so that upstream data may inform the planning of downstream activities (clinical interventions). Whilst, we do not live in an ideal world, given the vast advancement in hardware and software technology, we can conceptualise a unified database.As shown in Fig. 1, a virtual mega database may be conceptualised to provide access to life history events including health, morbidity (hospital records) and mortality records for professional practice, and, anonymised and aggregated life histories for research. We do not propose to re-invent the wheel by insisting on another physical database such as e-records. The unified database could be a set of communication software protocols acting as secure gateways to other databases, or, it can be a virtual database which is populated from other databases via communications software protocol. As suggested earlier, health and social outcome data and life event histories are already available but from different sources and in different formats. The technical issues in this scenario will relate to the architectural design of the database (or interface) and populating it with anonymised life history records. Of course the records will have to be linked perhaps via a unique identifier code such as a National Insurance number or social security number. It is also possible to conceptualise a unified database in terms of access to anonymised life histories which are linked by a unique identifier. The basic structure of a unified database will be a ‘hub’ that is enabled to communicate with other available databases and run queries on them. The hub will be software interfaced to perform basic as well as complex time series statistical modelling. In both scenarios, the ability to communicate in real time will need to be considered in order to help health care professionals make informed decisions.
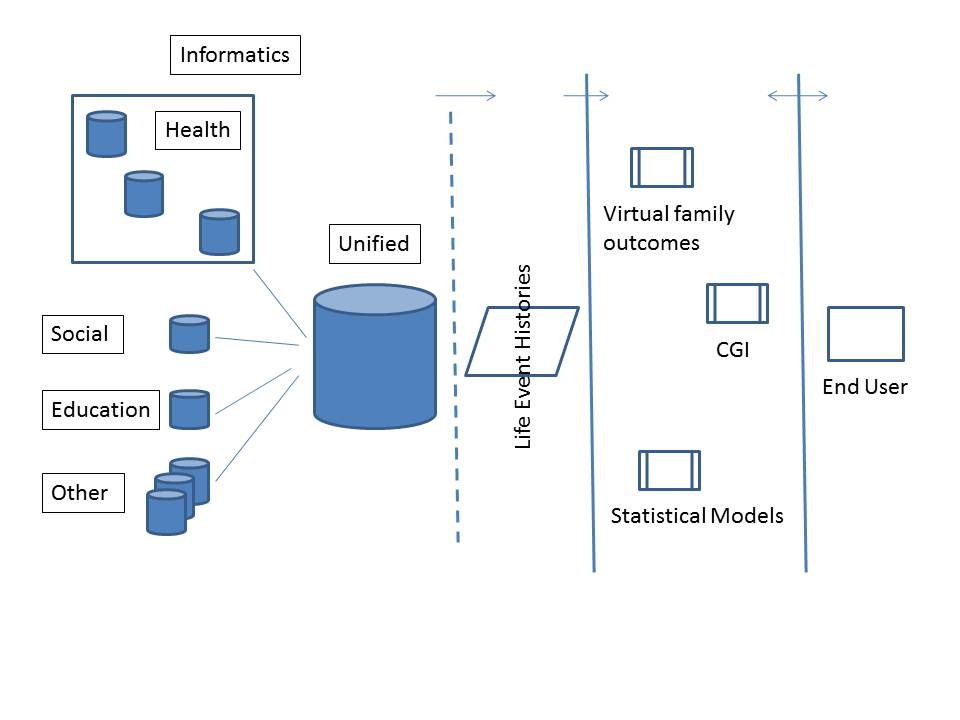 | Figure 1. A conceptual model of a unified (health) informatics |
3.5. Barriers to Adoption of Technologies
- Although, society responds well to technological gadgets and is enthusiastic about technology, its application in public administration is resource intensive, politicised and is challenged with legal and ethical issues including privacy and confidentiality. In the UK, during 1993-4, a proposal for the analysis of hospital records to utilise the added data item ‘social class’ did not proceed because the data item ‘social class’ had not been populated with relevant values. The extraordinary high missing values is not surprising as an exploratory analysis of such records suggested that professionals, on average, reported statutory minimum clinical data requirement. In an evaluation study of the English e-records system[29] a lack of compliance with reporting on all the data items, ethical considerations, skills gap, experience and knowledge of the systems in use, shortage of resources, immediate and free access to an informatics station, are some of the issues raised as barriers to full utilisation of the e-records. The shift towards a technology-based culture may also be reinforcing the barriers to the utilisation of new informatics systems. For example, at the Health Informatics New Zealand (HINZ) Conference 2010, speakers and delegates commonly described the available technologies such as smart pens, smart pads, e-health and mobile technology as solutions. In other words, we can now define, or, perhaps create a problem/market for which there exists a ‘solution’ in the form of a device. By the same token, the fact that we have lots of ‘solutions’ suggests that, as mentioned earlier, the advancing technology is no longer an issue but its applications are.However, most ‘solutions’ appear to address clinical administration e.g. improved and fast access to patients’ records, reduction in human error, and accounting. Given the extent of the technological advancement in hardware and software we ought to have, at some point, asked ourselves why stop with ‘solutions’ for administrative aspects of health care while there are questions that can be investigated? In other words, technological solutions must be human behaviour-led (evidence-based) and not the other way round. This approach can also assist to overcome some of the barriers in the full utilisation of technology. On the other hand, under a human behaviour-led approach barriers can be conceptualised as opportunities in developing more socially acceptable ‘solutions’, see Fig. 1. In other words, the inclusion of human and social parameters in the process of developing informatics systems at the concept stage will enhance the decision making process and its outcomes, see Fig. 2. Indeed, the conceptualisation considers the barriers part of the solution by assuming they are processes in their own right, and, processes are dynamic by nature. Thus barriers become multi-disciplinary research projects to inform the process of defining a unified database and its functions.
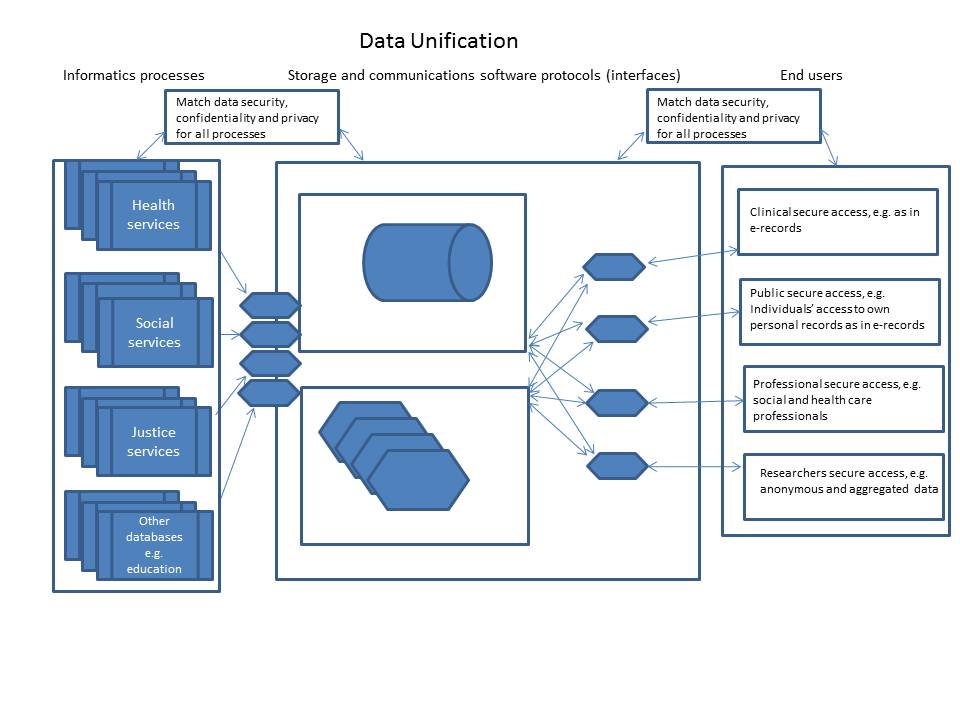 | Figure 2. Conceptualising the informatics processes |
|
4. Concluding Comments
- Ironically, the problems and issues discussed in this paper, including failing to prevent tragedies because different care agencies fail to communicate, were supposed to be resolved through major IT strategies both at government and agency level. The various strategies may have actually contributed to more complexities while addressing the digitisation of data. Due to market forces health care providers may have opted for the IT systems that met their IT strategy for their budget, e.g. value for money. A unified IT strategy approach would have been far better so that all care agencies would be invited to subscribe to the same purpose-build and designed data collection system. This approach would have reduced variability and facilitated communication between systems. However, as part of an IT strategy, some care agencies attempted to improve access to information. For example, with some systems mortality or morbidity (hospital records) data and appropriate population files can be queried through the organisation’s network. This solution can only provide a snapshot of the past mortality and morbidity in the context of a population. There is still no sign of a unified database, despite health outcomes having been linked to variations in social, economic and environmental circumstance[3-5], and the cumbersome methods of combining hospital data with data from other sources.Although meeting the challenges of utilising different datasets can be exciting and satisfying, the question arises yet again: why are health data from the same organisation in different sources some of which are incompatible with each other? Indeed, this was raised in the meeting of the steering group on the ‘Health of the Nation’s targets on Mental Health’, former Yorkshire Regional Health Authority (UK), and was adopted as one of the main guidelines on data collection ([30], pp12). The guideline prescribed that the health service commissioners develop a unified database by 1994 with a particular reference to suicide.In recent years, the under utilisation of technology has been echoed by others[12, 16]. While, Buchan et al[12] suggest methods of increasing access to data in addition to those from patients records, they propose the utilisation of technology for a unified modelling approach. They also propose a probability based graphical representation of analyses of data extracted through a number of interfaces with various data sources including e-records using machine learning and data mining techniques. They suggest that information captured from complex health data sets can be expressed through a framework of probabilistic graphical models in which relevant variables are expressed as graphs. Buchan et al[12] do not discuss the limitations of such an approach, for example their unified modelling approach lacks a statistical modelling approach which allows the selection of a parsimonious model from which inference may be made. Statistical data reduction techniques often used with large data sets are not suitable for inferential purposes[31, 32]. However, they are right to suggest that the graph may be used to guide the development of research questions. As mentioned above, most information systems, once unified, could potentially provide large scale life event histories. Modelling such data requires the understanding of substantive theories underpinning human behaviour such as temporal dependencies which will support the application of appropriate modelling approaches[32]. Other computerised models (e.g. see[33]) claim computers remove the barrier to accessing information with particular application for those ‘underserved’ such as minorities and elderly. In practice barriers remain in place until such a time that a policy is developed to (i) and a distinction between data and information is explicitly made, (ii) enable equal super-fast access to data by all, and (iii) account for the subsequent consequences of that access to data has on human behaviour[2].There are also the important cultural issues that may have been overlooked. Due to a highly dynamic computer and telecommunication industry, there has been a concerted socio-political effort by many nations not only to keep up with but also to lead technological advances. The resulting policies have been to maximise technology, in particular computer literacy through education (e.g. the policy of computers in every classroom) and improvements in access to computers (e.g. through public libraries) e.g. see[34, 35]. Such policies may have had an adverse effect on social and cultural outcomes e.g. the erosion of literacy skills (e.g. see[34, 35]). Nevertheless, upskilling the workforce with the emerging technologies is assumed to meet the needs of the industry. The flipside of the coin could be complacency and a lack of development of other aspects of informatics such as information. The two main issues relevant to information are what constitutes information and how it may be made accessible. In an earlier paper[2] these two issues were expanded and discussed. It was argued that the unregulated world wide access to the internet for depositing and extracting data exacerbated the problems associated with information. For example, the indications are that health services may be moving towards self-treatment using e-health ([36], also see http://computerworld.co.nz/news.nsf/management/health-it-board-drafts-e-health-plan; or,http://www.who.int/goe/ehir/2010/24-august-2010/en/index.html) and the question that needs to be investigated is the effect of technology on health related behaviour and more generally on human behaviour. Having access to and controlling one’s medical records does not necessarily increase one’s knowledge about one’s own health but may influence future health-related behaviour and in turn have a knock on effect on the health care system. Anecdotal evidence suggests that some individuals act on information access through the internet which may lead to a lack of medication compliance or incorrect (self-)treatment without consulting their GP or a medical professional[36, 37]. Quality information when critically assessed empowers individuals and may indeed lead to an informed decision. While access to uncritical data may lead to poor decisions and adversely affect health.It is noticeable that the technological issues are mainly concerned with advancement in the context of speed and user friendliness and system compatibility. It is our opinion that the technology has existed for some time[2] to develop a unified health care database, indeed, as mentioned above, the deployment of e-records provides some support for this argument. Furthermore, fast and super fast broadband has made it easier to share large amounts of data. However, even with the advent of e-records, we appear to be still grappling with the same old issues of access to data while overlooking the threshold when data may actually become information. In a changing environment (e.g. the impact of global warming on health care services) coupled with the dynamics of human behaviour, our information needs may be best served by a unified database that is not only responsive to clinical needs but also responds to the needs of the community and primary health care as well as research. Clearly, the success of such a project will involve tackling the issues raised as barriers to the adoption of technology including ethical considerations. Our approach is to identify and address the barrier issues as independent arms of the project which will inform the development and operationalisation of a unified database. The results from these projects will be reported in due course.IT and ICT have benefited from the health sector which provides a huge market for IT, the question is whether this relationship has led to commensurate benefits for the public. The deployment of a system such as e-records, undeniably improves access to important patient information. Improved access to information may indeed improve clinical decision making and potentially lead to a more effective delivery of care. However, unfortunately, this appears to be the extent of e-records. The real issue is how better e-records will perform than the current relatively low cost system that allows patients to wear a tag with their particular chronic condition, or, questions and answers at the time of delivery of care. Moreover, cases where e-records are updated overtime are simply a replication of the current patient data collection, albeit, in a different medium. In other words, do the outcomes in health care delivery, in an evidence-based decision making environment, justify the millions of dollars on hardware to maintain minimum datasets that are already available?The current (ill-)health informatics systems including e-records and e-health are a downstream philosophy and do nothing to provide further insight into health and the development of ill-health. For health informatics to be effective for the health service as a whole, some effort must be directed at developing software technology in conjunction with super fast broadband to create compatibility between the various sources of health and social data in order to populate a unified database so that it will provide important patient information. For example, a unified database may inform the process of understanding the long-term effects of a behaviour, e.g. maternal smoking or medication[38, 39], on an individuals’ health so that the health care service may become responsive. Finally, the health informatics community must come to grips with what is meant by health information[2], particularly in a climate where there is increasing interest in reaching consumers and patients directly through ICT[40].
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML