| [1] | Miah, M.R., Sayok, A.K., Rahman, AAMS, Samdany, A.A., Akhtar, F., Azad, A.K., Hasan, MM, Khan, M.S., Alam, S.E., Alam, MS., Uddin, M.B., Abdullah, F., Shahriar, C.S., Shamsuddin, MAS., Uddin, M.B., Sarok, A., Rahman, IT., Chowdhury, SC., Begum, M. (2021). Impact of Sensor Networks on Aquatic Biodiversity in Wetland: An Innovative Approach. Geosciences, 11(1), 10-42. doi:10.5923/j.geo.20211101.02. url: url: http://article.sapub.org/10.5923.j.geo.2021110.02.html. |
| [2] | Miah, M.R., Rahman, AAMS., Hasan, M.M., Parisa, J.T., Hannan, M.A., Hossain, M.M., Alam, M.S., Alam, M.S.E., Akhtar, F., Ghani, M.A., Khan, M.S., Shahriar, C.S., Sayok, A.K., Begum, M., Malik, S.U.F., Samdany, A.A., Ahmed, G. and Chowdhury, S.H. (2021). Adverse Effects of Wireless Sensor Technology to Debilitating in Numbness. International Journal of Virology and Molecular Biology, 10(1), 12-25. doi: 10.5923/j.ijvmb.20211001.03. |
| [3] | Miah, M.R. (2018). Assessment of Environmental Policy Instruments along with Information Systems for Biodiversity Conservation in Bangladesh. PhD Thesis. IBEC, UNIMAS, Malaysia. 1–480. url: https://ir.unimas.my/id/eprint/24535/2/Assessment%20of%20Environmental%20Policy%20ftext.Pdf. |
| [4] | Miah, M.R., Rahman, A.A.M.S., Khan, M.S., Samdany, A.A., Hannan, M.A., Chowdhury, S.H., Sayok, A.K. (2020). Impact of Sensor Technology Enhancing Corona Disease. American Journal of Biomedical Engineering, 10 (1), 1-11. doi: 10.5923/j.ajbe.20201002. |
| [5] | Miah, M.R., Rahman, A.A.M.S., Khan, M.S., Hannan, M.A., Hossain, M.S., Shahriar, C.S., Hossain, S.A.M.I., Talukdar, M.T.H., Samdany, A.A., Alam, M.S., Uddin, M.B., Sayok, A.K., and Chowdhury, S.H. (2021). Effect of Corona Virus Worldwide through Misusing of Wireless Sensor Networks. American Journal of Bioinformatics Research, 11(1), 1-31. url: http://article.sapub.org/10.5923.j.bioinformatics.20211101.01.html. |
| [6] | Miah, M.R., Rahman, A.A.M.S., Samdany, A.A., and Chowdhury, S.H. (2021). A Dynamic Scientific Model for Recovery of Corona Disease. Frontiers in Science, 11(1), 1-17. url: http://article.sapub.org/10.5923.j.fs.20211101.01.html. |
| [7] | Miah, M.R., Hannan, M.A., Rahman, AAMS., Khan, M.S., Hossain, M.M., Rahman, I.T., Hossain, M.S., Shahriar, C.S., Uddin, M.B., Talukdar, M.T.H., Alam, M.S., Hossain, S.A.M.I., Samdany, A.A., Chowdhury, S.H., Sayok, A.K. (2021). Processed Radio Frequency towards Pancreas Enhancing the Deadly Diabetes Worldwide. Journal of Endocrinology Research, 3(1), 1-20. url: https://ojs.bilpublishing.com/index.php/jer/article/view/2826. |
| [8] | Miah, M.R., Khan, M.S., Rahman, A.A.M.S., Samdany, A.A., Hannan, M.A., Chowdhury, S.H., and Sayok, A.K. (2020). Impact of Sensor Networks towards Individuals Augmenting Causes of Diabetes. International Journal of Diabetes Research, 9(2), 1-10. doi: 10.5923/j.diabetes.20200902. |
| [9] | Miah, M.R., Hasan, MM., Parisa, J.T., Alam, MSE, Hossain, MM., Akhtar, F., Begum, M., Sayok, AK., Abdullah, F., Shamsuddin, MAS., Rahman, AAMS., Alam, MS., Chowdhury, SH. (2021). Coronavirus: A Terrible Global Democracy. International Journal of Applied Sociology, 11(2), 46-82. |
| [10] | Miah, M.R., Rahman, A.A.M.S., Parisa, J.T., Hannan, M.A., Khan, M.S., Samdany, A.A., Sayok, A.K. and Chowdhury, S.H. (2021). Discovery of Coronavirus with Innovative Technology. Science and Technology, 11(1), 7-29. doi: 10.5923/j.scit.20211101.02. url: http://article.sapub.org/10.5923.j.scit.20211101.02.html. |
| [11] | Miah, M.R. (2020). Cyber Dajjal: Sushaysther Ontoray (Cyber Antichrist: Barrier to Good Health). Papriprakash, Rongmohol Tower, Bondor Bazar, Sylhet, Bangladesh. 1-128. ISBN: 978-984-586-041-3. url: https://www.rokomari.com/book/202988/cyber-dazzal---sushaysther-ontoray. |
| [12] | Roth, G.A., Mensah, G.A., Johnson, C.O., Addolorato, G., Ammirati, E., Baddour, L.M., Barengo, N.C., Beaton, A.Z., Benjamin, E.J., Benziger, C.P., Bonny, A., Brauer, M,, Brodmann, M., Cahill, T.J., Carapetis, J., Catapano, A.L., Chugh, S.S., Cooper, L.T., Coresh, J., Criqui, M., DeCleene, N., Eagle, K.A., Emmons-Bell, S., Feigin, V.L., Fernandez-Sola, J., Fowkes, G., Gakidou, E., Grundy, S.M., He, F.J., Howard, G., Hu, F., Inker, L., Karthikeyan, G., Kassebaum, N., Koroshetz, W., Lavie, C., Lloyd-Jones, D., Lu, H.S., Mirijello, A., Misganaw, T.A.,, Mokdad, A., Moran, A.E., Muntner, P., Narula, J., Neal, B., Ntsekhe, M., Moraes, de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundstrom J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray CJL, Fuster V. (2020). Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. Journal of the American College of Cardiology, 76(25 |
| [13] | Miah, M.R., Hasan,M.M., Hannan, M.A., Parisa, J.T., Uddin, M.J., Uddin, M.B., Rahman, A.A.M.S., Hossain, S.A.M.I., Sharif, M.A., Akhtar, F., Shamsuddin, M.A.S., Alam, M.S.E., Alam, M.S., Abdullah, F., Rahman, M.S., Uddin, M.Be., Shahriar, C.S., Sayok, A.K., Begum, M., Hossain, M.M., Khan, M.S., Ahmed, G., Malik, S.U.F., Samdany, A.A., Ghani, M.A., Hossain, M.S., Nazrin, M.S., Tamim, M.A.K., Selim, M.A., Talukdar, M.T.H., Chowdhury, F.T., Rashid, T.U., Nazim, A.Y.M., Rashid, M., Chowdhury, S.H. (2022). Myths about Coronavirus: A Research Defense. Global Journal of Health Science, 14(2), 63–112. url: https://ccsenet.org/journal/index.php/gjhs/article/view/0/46717. |
| [14] | Hayek, S. S., Brenner, S. K., Azam, T. U., Shadid, H. R., Anderson, E., Berlin, H., Pan, M., Meloche, C., Feroz, R., O’Hayer, P., Kaakati, R., Bitar, A., Padalia, K., Perry, D., Blakely, P., Gupta, S., Shaefi, S., Srivastava, A., Charytan, D.M., Bansal, A., Mallappallil, M., Melamed, M.L., Shehata, A.M., Sunderram, J., Mathews, K.S., Sutherland, A.K., Nallamothu, B.K. and Leaf, D. E. (2020). In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. BMJ, m3513. doi:10.1136/bmj.m3513. |
| [15] | Chan, J., Rea, T., Gollakota, S. Sunshine, J.E. (2019). Contactless cardiac arrest detection using smart devices. npj Digit. Med. 2, 52. doi: https://doi.org/10.1038/s41746-019-0128-7. |
| [16] | Paratz, E. D., Rowsell, L., Zentner, D., Parsons, S., Morgan, N., Thompson, T., … La Gerche, A. (2020). Cardiac arrest and sudden cardiac death registries: a systematic review of global coverage. Open Heart, 7(1), e001195. doi:10.1136/openhrt-2019-001195. |
| [17] | Islam, S. S. ., Rahman, M. F. ., Shams ul Huda, M. ., Kabir, S. H. ., & Hamid, M. A. . (2021). Awareness on Heart Diseases among Bangladesh Army Personnel. Journal of Armed Forces Medical College, Bangladesh, 16(2), 47–50. https://doi.org/10.3329/jafmc.v16i2.55298 |
| [18] | Chowdhury, M., Haque, M. A., Farhana, Z., Anik, A. M., Chowdhury, A. H., Haque, S. M., Marjana, L. L., Bristi, P. D., Al Mamun, B. A., Uddin, M. J., Fatema, J., Rahman, M. M., Akter, T., Tani, T. A., & Turin, T. C. (2018). Prevalence of cardiovascular disease among Bangladeshi adult population: a systematic review and meta-analysis of the studies. Vascular health and risk management, 14, 165–181. https://doi.org/10.2147/VHRM.S166111 |
| [19] | Nolan, .J., Soar, J. and Eikeland, H. (2006). The chain of survival. Resuscitation, 71: 2701. |
| [20] | Lott, C., Truhlář, A., Alfonzo, A., Barelli, A., González-Salvado, V., Hinkelbein, J., … Schmitz, J. (2021). European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances. Resuscitation, 161, 152–219. doi:10.1016/j.resuscitation.2021.02.011. |
| [21] | UNB. (2021). Cardiac arrest Bangladesh’s No. 1 killer in Bangladesh. United News of Bangladesh, Dhaka. Retrieved from https://unb.com.bd/category/Bangladesh/cardiac-arrest-bangladeshs-no-1-killer-in-2020-bbs/65908 (accessed to time on February 19, 2022 at 02:00 pm). |
| [22] | Wissenberg, M., Lippert FK, Folke F, et al. (2013). Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA, 310: 1377–84. doi: 10.1001/jama.2013.278483. |
| [23] | Geocadin, R. G. (2020). Moving Beyond One-Size-Fits-All Treatment for Patients After Cardiac Arrest. JAMA Network Open, 3(7), e208809. doi:10.1001/jamanetworkopen.2020.8809. |
| [24] | Callaway, C. W., Coppler, P. J., Faro, J., Puyana, J. S., Solanki, P., Dezfulian, C., … Weissman, A. (2020). Association of initial illness severity and outcomes after cardiac arrest with targeted temperature management at 36°C or 33°C. JAMA Netw Open, 3(7): e208215. doi:10.1001/jamanetworkopen.2020.8215. |
| [25] | AHA. (2022). About Cardiac Arrest. American Heart Association. Retrieved from https://www.heart.org/en/health-topics/cardiac-arrest/about-cardiac-arrest (accessed time to January 20, 2022 on 11:00am). |
| [26] | Sasson, C., Rogers, M. A. M., Dahl, J., & Kellermann, A. L. (2009). Predictors of Survival from Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. Circulation: Cardiovascular Quality and Outcomes, 3(1), 63–81. doi:10.1161/circoutcomes.109.88. |
| [27] | Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O’Donnell C, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y. (2008). Heart disease and stroke statistics–2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation, 117: e25–e146. |
| [28] | Cone D. (2014). Developing the science of out-of-hospital termination of resuscitation. Resuscitation, 85:446–7. |
| [29] | Fukuda T, Ohashi N, Matsubara T, et al. (2014). Applicability of the prehospital termination of resuscitation rule in an area dense with hospitals in Tokyo: a single-center, retrospective, observational study: is the pre-hospital TOR rule applicable in Tokyo? Am J Emerg Med, 32:144–9. |
| [30] | Morrison LJ, Verbeek PR, Zhan C, et al. (2009). Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation, 80:324–8. |
| [31] | Chiang WC, Ko PC, Chang AM, et al. (2015). Predictive performance of universal termination of resuscitation rules in an Asian community: are they accurate enough? Emerg Med J., 32:318–23. |
| [32] | Ebben RH, Vloet LC, Verhofstad MH, et al. (2013). Adherence to guidelines and protocols in the prehospital and emergency care setting: a systematic review. Scand J Trauma Resusc Emerg Med, 21:9. |
| [33] | Morrison LJ, Eby D, Veigas PV, et al. (2014). Implementation trial of the basic life support termination of resuscitation rule: reducing the transport of futile out-of-hospital cardiac arrests. Resuscitation, 85:486–91. |
| [34] | Bossaert LL, Perkins GD, Askitopoulou H, et al. (2015). European resuscitation council guidelines for resuscitation 2015: section 11. the ethics of resuscitation and end-of-life decisions. Resuscitation, 95:302–11. |
| [35] | Mancini ME, Diekema DS, Hoadley TA, et al. (2015). Part 3: ethical issues: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 132:S383–S396. |
| [36] | Anderson NE, Gott M, Slark J. (2017). Commence, continue, withhold or terminate?: a systematic review of decision-making in out-of-hospital cardiac arrest. Eur J Emerg Med, 24:80–6. |
| [37] | McLennan S, Paterson R, Skegg P, et al. (2011). The use of CPR in New Zealand: is it always lawful? NZ Med J, 124:106–12. |
| [38] | Hennink MM, Kaiser BN, Marconi VC. (2017). Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res, 27:591–608. |
| [39] | Kelly CA and O’Brien MR. (2015). Difficult decisions: an interpretative phenomenological analysis study of healthcare professionals’ perceptions of oxygen therapy in palliative care. Palliat Med, 29:950–8. |
| [40] | Miller S and Dorman S. (2014). Resuscitation decisions for patients dying in the community: a qualitative interview study of general practitioner perspectives. Palliat Med, 28:1053–61. |
| [41] | Smith JA. (2011). Evaluating the contribution of interpretative phenomenological analysis. Health Psychol Rev, 5:9–27. |
| [42] | Smith JA, Flowers P, Larkin M. (2009). Interpretative phenomenological analysis: theory, method and research. London: Sage, 2009. |
| [43] | Lockey AS, Hardern RD. (2001). Decision making by emergency physicians when assessing cardiac arrest patients on arrival at hospital. Resuscitation, 50:51–6. |
| [44] | Marco CA, Schears RM. (2003). Prehospital resuscitation practices: a survey of prehospital providers. J Emerg Med, 24:101–6. |
| [45] | Willmott L, White B, Gallois C, et al. (2016). Reasons doctors provide futile treatment at the end of life: a qualitative study. J Med Ethics, 42:496–503. |
| [46] | Grudzen CR, Timmermans S, Koenig WJ, et al. (2009). Paramedic and emergency medical technicians’ views on opportunities and challenges when forgoing and halting resuscitation in the field. Acad Emerg Med, 16:532–8. |
| [47] | Marco CA, Bessman ES, Kelen GD. (2009). Ethical issues of cardiopulmonary resuscitation: comparison of emergency physician practices from 1995 to 2007. Acad Emerg Med., 16:270–3. |
| [48] | Bradley EH, Curry LA, Devers KJ. (2007). Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res., 42:1758–72. |
| [49] | Anderson, N. E., Gott, M., & Slark, J. (2018). Beyond prognostication: ambulance personnel’s lived experiences of cardiac arrest decision-making. Emergency Medicine Journal, 35(4), 208–213. doi:10.1136/emermed-2017-206743. |
| [50] | Kaptoge, S., Pennells, L., De Bacquer, D., Cooney, M. T., Kavousi, M., Stevens, G., … Altay, S. (2019). World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. The Lancet Global Health, 7, e1332-e1345. doi:10.1016/s2214-109x(19)30318-3. |
| [51] | Tirodkar, M. A., Baker, D. W., Khurana, N., Makoul, G., Paracha, M. W., & Kandula, N. R. (2011). Explanatory models of coronary heart disease among South Asian immigrants. Patient Education and Counseling, 85(2), 230–236. doi:10.1016/j.pec.2010.10.002. |
| [52] | Kitamura T, Kiyohara K, Sakai T, et al. (2014). Epidemiology and outcome of adult out-of-hospital cardiac arrest of non-cardiac origin in Osaka: a population-based study. BMJ Open, 4:e006462. |
| [53] | Lee S, Bellolio MF, Hess EP, Campbell RL. (2014). Predictors of biphasic reactions in the emergency department for patients with anaphylaxis. J Allergy Clin Immunol Pract, 2:2817. |
| [54] | Soar J, Carli P, Couper K, et al. (2021). European Resuscitation Council Guidelines 2021: advanced life support. Resuscitation, 161. |
| [55] | Harper NJN, Nolan JP, Soar J, Cook TM. (2020). Why chest compressions should start when systolic arterial blood pressure is below 50 mmHg in the anaesthetised patient. Br J Anaesth, 124:2348. |
| [56] | Soar J, Maconochie I, Wyckoff MH, et al. (2019). International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation, 145:95150. |
| [57] | Soar J, Pumphrey R, Cant A, et al. (2008). Emergency treatment of anaphylactic reactions—guidelines for healthcare providers. Resuscitation, 77:15769. |
| [58] | Excellence NIfHaC. (2016). Sepsis: recognition, assessment and eraly management. NICE Guideline 51. London: National Insitute for Health and Care Excellence; 2016. |
| [59] | Levy MM, Evans LE, Rhodes A. (2018). The surviving sepsis campaign bundle: 2018 update. Intensive Care Med., 44:9258. |
| [60] | Levy MM, Dellinger RP, Townsend SR, et al. (2010). The surviving sepsis campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med, 38:36774. |
| [61] | Levy MM, Rhodes A, Phillips GS, et al. (2015). Surviving sepsis campaign: association between performance metrics and outcomes in a 7.5- year study. Crit Care Med, 43:312. |
| [62] | Asfar P, Meziani F, Hamel JF, et al. (2014). High versus low blood-pressure target in patients with septic shock. N Engl J Med, 370:158393. |
| [63] | Farmery AD, Roe PG. (1996). A model to describe the rate of oxyhaemoglobin desaturation during apnoea. Br J Anaesth, 76:28491. |
| [64] | Lamontagne F, Meade MO, Hebert PC, et al. (2016). Higher versus lower blood pressure targets for vasopressor therapy in shock: a multicentre pilot randomized controlled trial. Intensive Care Med, 42:54250. |
| [65] | Gu WJ, Zhang Z, Bakker J. (2015). Early lactate clearance-guided therapy in patients with sepsis: a meta-analysis with trial sequential analysis of randomized controlled trials. Intensive Care Med, 41:18623. |
| [66] | Simpson SQ, Gaines M, Hussein Y, Badgett RG. (2016). Early goal-directed therapy for severe sepsis and septic shock: a living systematic review. J Crit Care, 36:438. |
| [67] | Acheampong A, Vincent JL. (2015). A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care, 19:251. |
| [68] | Brotfain E, Koyfman L, Toledano R, et al.(2016). Positive fluid balance as a major predictor of clinical outcome of patients with sepsis/septic shock after ICU discharge. Am J Emerg Med, 34:21226. |
| [69] | Mitchell KH, Carlbom D, Caldwell E, et al. (2015). Volume overload: prevalence, risk factors, and functional outcome in survivors of septic shock. Ann Am Thorac Soc, 12:183744. |
| [70] | Alfonzo A, Harris A, Baines R, Chu A, Mann S. (2020). Clinical practice guidelines treatment of acute hyperkalaemia in adults. London: The Renal Association; 2020. |
| [71] | Moore ML, Bailey RR. (1989). Hyperkalaemia in patients in hospital. N Z Med J, 102:5578. |
| [72] | Shemer J, Modan M, Ezra D, Cabili S. (1983). Incidence of hyperkalemia in hospitalized patients. Isr J Med Sci., 19:65961. |
| [73] | Conway R, Creagh D, Byrne DG, O’Riordan D, Silke B. (2015). Serum potassium levels as an outcome determinant in acute medical admissions. Clin Med (Lond), 15:23943. |
| [74] | DeBehnke DJ, Hilander SJ, Dobler DW, Wickman LL, Swart GL. (1995). The hemodynamic and arterial blood gas response to asphyxiation: a canine model of pulseless electrical activity. Resuscitation, 30:16975. |
| [75] | Wallmuller C, Meron G, Kurkciyan I, et al. (2012). Causes of in-hospital cardiac arrest and influence on outcome. Resuscitation, 83:120611. |
| [76] | Wang CH, Huang CH, Chang WT, et al. (2016).The effects of calcium and sodium bicarbonate on severe hyperkalaemia during cardiopulmonary resuscitation: a retrospective cohort study of adult in-hospital cardiac arrest. Resuscitation, 98:10511. |
| [77] | SaarinenS, Nurmi J, Toivio T, et al. (2012). Does appropriate treatment of the primary underlying cause of PEA during resuscitation improve patients’ survival? Resuscitation, 83: 81922. |
| [78] | Smellie WS. (2007). Spurious hyperkalaemia. BMJ, 334:6935. |
| [79] | Sevastos N, Theodossiades G, Archimandritis AJ. (2008). Pseudohyperkalemia in serum: a new insight into an old phenomenon. Clin Med Res, 6:302. |
| [80] | Ahn S, Kim WY, Sohn CH, et al. (2011). Potassium values in cardiac arrest patients measured with a point-of-care blood gas analyzer. Resuscitation, 82:e256. |
| [81] | Allardet-Servent J, Lebsir M, Dubroca C, et al. (2017). Point-of-care versus central laboratory measurements of hemoglobin, hematocrit, glucose, bicarbonate and electrolytes: a prospective observational study in critically ill patients. PLoS One, e0169593. |
| [82] | Dashevsky M, Bernstein SL, Barsky CL, Taylor RA. (2017). Agreement between serum assays performed in ED point-of-care and hospital central laboratories. West J Emerg Med, 18:4039. |
| [83] | Acikgoz SB, Genc AB, SipahiS, et al. (2016). Agreement of serum potassium measured by blood gas and biochemistry analyzer in patients with moderate to severe hyperkalemia. Am JEmerg Med, 34:7947. |
| [84] | Durfey N, Lehnhof B, Bergeson A, et al. (2017). Severe hyperkalemia: can the electrocardiogram risk stratify for short-term adverse events? West J Emerg Med, 18:96371. |
| [85] | Deasy C, Bray J, Smith K, et al. (2013). Hanging-associated out-of-hospital cardiac arrests in Melbourne, Australia. Emerg Med., 30: 3842. |
| [86] | Batterink J, Lin J, Au-Yeung SH, Cessford T.(2015). Effectiveness of sodium polystyrene sulfonate for short-term treatment of hyperkalemia. Can J Hosp Pharm, 68:296303. |
| [87] | Moussavi K, Nguyen LT, Hua H, Fitter S. (2020). Comparison of IV insulin dosing strategies for hyperkalemia in the emergency department. Crit Care Explor., 2: e0092. |
| [88] | Farina N, Anderson C. (2018). Impact of dextrose dose on hypoglycemia development following treatment of hyperkalemia. TherAdv DrugSaf., 9:3239. |
| [89] | Apel J, Reutrakul S, Baldwin D. (2014). Hypoglycemia in the treatment of hyperkalemia with insulin in patients with end-stage renal disease. Clin Kidney J., 7:24850. |
| [90] | Coca A, Valencia AL, Bustamante J, Mendiluce A, Floege J. (2017). Hypoglycemia following intravenous insulin plus glucose for hyperkalemia in patients with impaired renal function. PLoS One, 12:e0172961. |
| [91] | Scott NL, Klein LR, Cales E, Driver BE. (2019). Hypoglycemia as a complication of intravenous insulin to treat hyperkalemia in the emergency department. Am J Emerg Med., 37:20913. |
| [92] | Boughton CK, Dixon D, Goble E, et al. (2019). Preventing hypoglycemia following treatment of hyperkalemia in hospitalized patients. J Hosp Med., 14:2847. |
| [93] | LaRue HA, Peksa GD, Shah SC. (2017). A comparison of insulin doses for the treatment of hyperkalemia in patients with renal insufficiency. Pharmacotherapy, 37:151622. |
| [94] | Garcia J, Pintens M, Morris A, et al. (2020). Reduced versus conventional dose insulin for hyperkalemia treatment. J Pharm Pract., 33:2626. |
| [95] | Pierce DA, Russell G, Pirkle Jr JL. (2015). Incidence of hypoglycemia in patients with low eGFR treated with insulin and dextrose for hyperkalemia. Ann Pharmacother, 49:13226. |
| [96] | Olasveengen TM, Mancini ME, Perkins GD, et al. (2020). Adult basic life support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation, 142:S4191. |
| [97] | Allon M, Copkney C. (1990). Albuterol and insulin for treatment of hyperkalemia in hemodialysis patients. Kidney Int., 38:86972. |
| [98] | Ahmed J, Weisberg LS. (2001). Hyperkalemia in dialysis patients.Semin Dial., 14:34856. |
| [99] | Lens XM, Montoliu J, Cases A, Campistol JM, Revert L. (1989). Treatment of hyperkalaemia in renal failure: salbutamol v. insulin. Nephrol Dial Transplant., 4:22832. |
| [100] | Excellence NIfHaC. (2019). Sodium zirconium cyclosilicate for treating hyperkalaemia. Technology Appraisal Guidance TA599. London: National Institute for Health and Care Excellence; 2019. |
| [101] | Excellence NIfHaC. (2020). Patiromer for treating hyperkalaemia. Technology Appraisal Guidance TA623. London: National Institute for Health and Care Excellence; 2020. |
| [102] | Zeneca Astra. (2020). Lokelma (sodium zirconium cyclosilicate) for oral suspension: Summary of product characteristics. www.ema.europa. eu/ema/. |
| [103] | Kosiborod M, Rasmussen HS, Lavin P, et al. (2014). Effect of sodium zirconium cyclosilicate on potassium lowering for 28 days among outpatients with hyperkalemia: the HARMONIZE randomized clinical trial. JAMA, 312:222333. |
| [104] | Spinowitz BS, Fishbane S, Pergola PE, et al. (2019). Sodium zirconium cyclosilicate among individuals with hyperkalemia: A 12-month phase 3 study. Clin J Am Soc Nephrol., 14:798809. |
| [105] | Meaney CJ, Beccari MV, Yang Y, Zhao J. (2017). Systematic review and meta-analysis of patiromer and sodium zirconium cyclosilicate: a new armamentarium for the treatment of hyperkalemia. Pharmacotherapy, 37:40111. |
| [106] | Rafique Z, Liu M, Staggers KA, Minard CG, Peacock WF. (2020). Patiromer for treatment of hyperkalemia in the emergency department: a pilot study. Acad Emerg Med., 27:5460. |
| [107] | Olasveengen TM, Semeraro F, Ristagno G, et al. (2021). European Resuscitation Council Guidelines 2021: basic life support. Resuscitation, 161. |
| [108] | Peacock WF, Rafique Z, Vishnevskiy K, et al. (2020). Emergency potassium normalization treatment including sodium zirconium cyclosilicate: a phase II, randomized, double-blind, placebo-controlled study (ENERGIZE). Acad Emerg Med., 27:47586. |
| [109] | Lin JL, Lim PS, Leu ML, Huang CC. (1994). Outcomes of severe hyperkalemia in cardiopulmonary resuscitation with concomitant hemodialysis. Intensive Care Med., 20:28790. |
| [110] | KaoKC, Huang CC, TsaiYH, Lin MC, TsaoTC. (2000). Hyperkalemic cardiac arrest successfully reversed by hemodialysis during cardiopulmonary resuscitation: case report. Changgeng Yi Xue Za Zhi., 23:5559. |
| [111] | Chiu CC, Yen HH, Chen YL, Siao FY. (2014). Severe hyperkalemia with refractory ventricular fibrillation: successful resuscitation using extracorporeal membrane oxygenation. Am J Emerg Med., 32: 943 e56. |
| [112] | Kim Sh, Song Jh, Jung Kt. (2019). Combination of extracorporeal membrane oxygenation and inline hemofiltration for the acute hyperkalemic cardiac arrest in a patient with Duchenne muscular dystrophy following orthopedic surgery—a case report. Korean J Anesthesiol., 72:17883. |
| [113] | Klingkowski U, Kropshofer G, Crazzolara R, Schachner T, Cortina G. (2019). Refractory hyperkalaemic cardiac arrest—what to do first: treat the reversible cause or initiate E-CPR? Resuscitation, 42:81. |
| [114] | Jensen HK, Brabrand M, Vinholt PJ, Hallas J, Lassen AT. (2015). Hypokalemia in acute medical patients: risk factors and prognosis. Am J Med., 128: 607 e1. |
| [115] | Chen Y, Chang AR, McAdams DeMarco MA, et al. (2016). Serum potassium, mortality, and kidney outcomes in the atherosclerosis risk in communities’ study. Mayo Clin Proc., 91:140312. |
| [116] | Skogestad J, Aronsen JM. (2018). Hypokalemia-induced arrhythmias and heart failure: new insights and implications for therapy. Front Physiol., 9:1500. |
| [117] | Steiness E, Olesen KH. (1976). Cardiac arrhythmias induced by hypokalaemia and potassium loss during maintenance digoxin therapy. Br Heart J., 38:16772. |
| [118] | Ogawa T, Akahane M, KoikeS, et al. (2011). Outcomes of chest compression only CPR versus conventional CPR conducted by lay people in patients with out of hospital cardiopulmonary arrest witnessed by bystanders: nationwide population based observational study. BMJ., 342:c7106. |
| [119] | Kardalas E, Paschou SA, Anagnostis P, et al. (2018). Hypokalemia: a clinical update. Endocr Connect., 7: R135R46. |
| [120] | Huang CL, Kuo E. (2007). Mechanism of hypokalemia in magnesium deficiency. J Am Soc Nephrol., 18:264952. |
| [121] | Pasquier M, Hugli O, Paal P, et al. (2018). Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: the HOPE score. Resuscitation, 126:5864. |
| [122] | Pasquier M, Rousson V, Darocha T, et al. (2019). Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: an external validation of the HOPE score. Resuscitation, 139:3218. |
| [123] | Frei C, Darocha T, Debaty G, et al. (2019). Clinical characteristics and outcomes of witnessed hypothermic cardiac arrest: a systematic review on rescue collapse. Resuscitation, 137:418. |
| [124] | Podsiadlo P, Darocha T, Svendsen OS, et al. (2020). Outcomes of patients suffering unwitnessed hypothermic cardiac arrest rewarmed with extracorporeal life support: a systematic review. Artif Organs 2020. |
| [125] | Fujimoto Y, Matsuyama T, Morita S, et al. (2020). Indoor versus outdoor occurrence in mortality of accidental hypothermia in Japan: the Jpoint registry. Ther Hypothermia Temp Manag., 10:15964. |
| [126] | Paal P, Rauch S. (2018). Indoor accidental hypothermia in the elderly: an emerging lethal entity in the 21st century. Emerg Med., 35: 6678. |
| [127] | Strapazzon G, Procter E, Paal P, Brugger H. (2014). Pre-hospital core temperature measurement in accidental and therapeutic hypothermia. High Alt Med Biol., 15:10411. |
| [128] | Pasquier M, Paal P, Kosinski S, et al. (2020). Esophageal temperature measurement. N Engl J Med., 383:e93. |
| [129] | Riva G, Ringh M, Jonsson M, et al. (2019). Survival in out-of-hospital cardiac arrest after standard cardiopulmonary resuscitation or chest compressions only before arrival of emergency medical services: nationwide study during three guideline periods. Circulation 2019. |
| [130] | Strapazzon G, Procter E, Putzer G, et al. (2015). Influence of low ambient temperature on epitympanic temperature measurement: a prospective randomized clinical study. Scand J Trauma Resusc Emerg Med., 23:90. |
| [131] | Muth CM, Shank E, Hauser B, et al. (2010). Infrared ear thermometry in water-related accidents-not a good choice. J Emerg Med., 38:41721. |
| [132] | Henriksson O, Lundgren PJ, Kuklane K, et al. (2015). Protection against cold in prehospital care: wet clothing removal or addition of a vapor barrier. Wilderness Environ Med., 26:1120. |
| [133] | Lundgren P, Henriksson O, Naredi P, Bjornstig U. (2011). The effect of active warming in prehospital trauma care during road and air ambulance transportation—a clinical randomized trial. Scand J Trauma Resusc Emerg Med., 19:59. |
| [134] | Darocha T, Kosinski S, Jarosz A, et al. (2017). Should capnography be used as a guide for choosing a ventilation strategy in circulatory shock caused by severe hypothermia? Observational case-series study. Scand J Trauma Resusc Emerg Med., 25:15. |
| [135] | Pasquier M, Zurron N, Weith B, et al. (2014). Deep accidental hypothermia with core temperature below 24 degrees c presenting with vital signs. High Alt Med Biol., 15:5863. |
| [136] | Mroczek T, Gladki M, Skalski J. (2020). Successful resuscitation from accidental hypothermia of 11.8 degrees C: where is the lower bound for human beings? Eur J Cardiothorac Surg., 58:10912. |
| [137] | Stephen CR, Dent SJ, Hall KD, Smith WW. (1961). Physiologic reactions during profound hypothermia with cardioplegia. Anesthesiology, 22:87381. |
| [138] | Brugger H, Bouzat P, Pasquier M, et al. (2019). Cut-off values of serum potassium and core temperature at hospital admission for extracorporeal rewarming of avalanche victims in cardiac arrest: a retrospective multi-centre study. Resuscitation, 139:2229. |
| [139] | Saczkowski Rs, Brown Dja, Abu-Laban Rb, et al. (2018). Prediction and risk stratification of survival in accidental hypothermia requiring extracorporeal life support: an individual patient data meta-analysis. Resuscitation, 127:517. |
| [140] | Escutnaire J, Ducrocq F, Singier A, et al. (2018). Can we define termination of resuscitation criteria in out-of-hospital hanging? Prehosp Emerg Care, 18. |
| [141] | Gordon L, Paal P. (2018). Normothermic and hypothermic cardiac arrest Beware of Jekyll and Hyde. Resuscitation, 129: e10e1. |
| [142] | Pasquier M, Paal P, Blancher M, Darocha T. (2019). Higher survival chances of hypothermic vs. normothermic cardiac arrest patients with ECLS re-warming. Resuscitation, 134:1612. |
| [143] | Althaus U, Aeberhard P, Schupbach P, Nachbur BH, Muhlemann W. (1982). Management of profound accidental hypothermia with cardiorespiratory arrest. Ann Surg., 195:4925. |
| [144] | Lexow K. (1991). Severe accidental hypothermia: survival after 6 hours 30 minutes of cardiopulmonary resuscitation. Arctic Med Res., 50:1124. |
| [145] | Wood S. (1991). Interactions between hypoxia and hypothermia. Annu Rev Physiol., 53:7185. |
| [146] | Mair P, Gasteiger L, Mair B, Stroehle M, Walpoth B. (2019). Successful defibrillation of four hypothermic patients with witnessed cardiac arrest. High Alt Med Biol., 20:717. |
| [147] | Stoner J, Martin G, O’Mara K, Ehlers J, Tomlanovich M. (2003). Amiodarone and bretylium in the treatment of hypothermic ventricular fibrillation in a canine model. Acad Emerg Med., 10:18791. |
| [148] | Krismer AC, Lindner KH, Kornberger R, et al. (2000). Cardiopulmonary resuscitation during severe hypothermia in pigs: does epinephrine or vasopressin increase coronary perfusion pressure? Anesth Analg., 90:6973. |
| [149] | Kornberger E, Lindner KH, Mayr VD, et al. (2001). Effects of epinephrine in a pig model of hypothermic cardiac arrest and closed-chest cardiopulmonary resuscitation combined with active rewarming. Resuscitation, 50:3018. |
| [150] | Mazur P, Kosinski S, Podsiadlo P, et al. (2019). Extracorporeal membrane oxygenation for accidental deep hypothermia-current challenges and future perspectives. Ann Cardiothorac Surg., 8:13742. |
| [151] | Kim MJ, Yoon YS, Park JM, et al. (2016). Neurologic outcome of comatose survivors after hanging: a retrospective multicenter study. Am J Emerg Med., 34: 146772. |
| [152] | Ruttmann E, Weissenbacher A, Ulmer H, et al. (2007). Prolonged extracorporeal membrane oxygenation-assisted support provides improved survival in hypothermic patients with cardiocirculatory arrest. J Thorac Cardiovasc Surg., 134:594600. |
| [153] | Gruber E, Beikircher W, Pizzinini R, et al. (2014). Non-extracorporeal rewarming at a rate of 6.8 degrees C per hourin a deeply hypothermic arrested patient. Resuscitation, 85: e11920. |
| [154] | Kuhnke M, Albrecht R, Schefold JC, Paal P. (2019). Successful resuscitation from prolonged hypothermic cardiac arrest without extracorporeal life support: a case report. J Med Case Rep., 13:354. |
| [155] | Boue Y, Payen JF, Brun J, et al. (2014). Survival after avalanche-induced cardiac arrest. Resuscitation, 85:11926. |
| [156] | Moroder L, Mair B, Brugger H, Voelckel W, Mair P. (2015). Outcome of avalanche victims with out-of-hospital cardiac arrest. Resuscitation, 89:1148. |
| [157] | Metrailler-Mermoud J, Hugli O, Carron PN, et al. (2019). Avalanche victims in cardiac arrest are unlikely to survive despite adherence to medical guidelines. Resuscitation, 141:3543. |
| [158] | Brugger H, Durrer B, Elsensohn F., et al. (2013). Resuscitation of avalanche victims: evidence-based guidelines of the international commission for mountain emergency medicine (ICAR MEDCOM): intended for physicians and other advanced life support personnel. Resuscitation, 84:53946. |
| [159] | Van Tilburg C, Grissom CK, Zafren K, et al. (2017). Wilderness Medical Society Practice Guidelines for prevention and management of avalanche and nonavalanche snow burial accidents. Wilderness Environ Med., 28:2342. |
| [160] | Kay JE. (2020). Early climate models successfully predicted global warming. Nature, 578:456. |
| [161] | Epstein Y, Yanovich R. (2019). Heatstroke. N Engl J Med., 380: 244959. |
| [162] | Soar J, Berg KM, Andersen LW, et al. (2020). Adult advanced life support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation, 156:A80A119. |
| [163] | Deasy C, Bray J, Smith K, et al. (2011). Paediatric hanging associated out of hospital cardiac arrest in Melbourne, Australia: characteristics and outcomes. Emerg Med., 28:4115. |
| [164] | Robine JM, Cheung SL, Le Roy S, et al. (2008). Death toll exceeded 70,000 in Europe during the summer of 2003. C R Biol., 331:1718. |
| [165] | Hayashida K, Shimizu K, Yokota H. (2019). Severe heatwave in Japan. Acute Med Surg., 6:2067. |
| [166] | Lipman GS, Gaudio FG, Eifling KP, et al. (2019). Wilderness Medical Society Clinical Practice Guidelines for the prevention and treatment of heat illness: 2019 update. Wilderness Environ Med., 30:S3346. |
| [167] | Douma MJ, Aves T, Allan KS, et al. (2020). First aid cooling techniques for heat stroke and exertional hyperthermia: a systematic review and meta-analysis. Resuscitation, 148:17390. |
| [168] | Shapiro Y, Seidman DS. (1990). Field and clinical observations of exertional heat stroke patients. Med Sci Sports Exerc., 22:614. |
| [169] | McDermott BP, Casa DJ, Ganio MS, et al. (2009). Acute whole-body cooling for exercise-induced hyperthermia: a systematic review. J Athl Train., 44:8493. |
| [170] | Hew-Butler T, Rosner MH, Fowkes-Godek S, et al. (2015). Statement of the 3rd International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Br J Sports Med., 49:143246. |
| [171] | Bouchama A, Dehbi M, Chaves-Carballo E. (2007). Cooling and hemodynamic management in heatstroke: practical recommendations. Crit Care., 11:R54. |
| [172] | Litman RS, Griggs SM, Dowling JJ, Riazi S. (2018). Malignant hyperthermia susceptibility and related diseases. Anesthesiology, 128: 15967. |
| [173] | Riazi S, Kraeva N, Hopkins PM. (2018). Malignant hyperthermia in the postgenomics era: new perspectives on an old concept. Anesthesiology, 128:16880. |
| [174] | Wee JH, Park KN, Oh SH, et al. (2012). Outcome analysis of cardiac arrest due to hanging injury. Am J Emerg Med., 30: 6904. |
| [175] | Hall AP, Henry JA. (2006). Acute toxic effects of ‘Ecstasy’ (MDMA) and related compounds: overview of pathophysiology and clinical management. Br J Anaesth., 96: 67885. |
| [176] | Eshel G, Safar P, Sassano J, Stezoski W. (1990). Hyperthermia-induced cardiac arrest in dogs and monkeys. Resuscitation, 20:12943. |
| [177] | Zeiner A, Holzer M, Sterz F, et al. (2001). Hyperthermia after cardiac arrest is associated with an unfavorable neurologic outcome. Arch Intern Med., 161:200712. |
| [178] | Konstantinides SV, Meyer G, Becattini C, et al. (2020). 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J., 41: 543603. |
| [179] | Javaudin F, Lascarrou JB, Le Bastard Q, et al. (2019). Thrombolysis during resuscitation for out-of-hospital cardiac arrest caused by pulmonary embolism increases 30-day survival: findings from the French National Cardiac Arrest Registry. Chest, 156:116775. |
| [180] | Bottiger BW, Arntz HR, Chamberlain DA, et al. (2008). Thrombolysis during resuscitation for out-of-hospital cardiac arrest. N Engl J Med., 359:265162. |
| [181] | Bergum D, Nordseth T, Mjolstad OC, Skogvoll E, Haugen BO. (2015). Causes of in-hospital cardiac arrest — incidences and rate of recognition. Resuscitation, 87:638. |
| [182] | Kurkciyan I, Meron G, Sterz F, et al. (2000). Pulmonary embolism as a cause of cardiac arrest: presentation and outcome. Arch Intern Med., 160:152935. |
| [183] | Pokorna M, Necas E, Skripsky R, et al. (2011). How accurately can the aetiology of cardiac arrest be established in an out-of-hospital setting? Analysis by “concordance in diagnosis crosscheck tables”. Resuscitation, 82:3917. |
| [184] | Aagaard R, Lofgren B, Caap P, et al. (2018). A low end-tidal CO2/arterial CO2 ratio during cardiopulmonary resuscitation suggests pulmonary embolism. Resuscitation, 133:13740. |
| [185] | Davies D, Lang M, Watts R. (2011). Paediatric hanging and strangulation injuries: a 10-year retrospective description of clinical factors and outcomes. Paediatr Child Health, 16:e7881. |
| [186] | GroupS-KS, InokuchiS, MasuiY, et al. (2016). Investigation and treatment of pulmonary embolism as a potential etiology may be important to improve post-resuscitation prognosis in non-shockable out-ofhospital cardiopulmonary arrest: report on an analysis of the SOSKANTO 2012 study. Acute Med Surg., 3:2509. |
| [187] | Heradstveit BE, Sunde K, Sunde GA, Wentzel-Larsen T, Heltne JK. (2012). Factors complicating interpretation of capnography during advanced life support in cardiac arrest—a clinical retrospective study in 575 patients. Resuscitation, 83:8138. |
| [188] | White RH. (2003). The epidemiology of venous thromboembolism. Circulation, 107:I48. |
| [189] | Geibel A, Zehender M, Kasper W, et al. (2005). Prognostic value of the ECG on admission in patients with acute major pulmonary embolism. Eur Respir J., 25:8438. |
| [190] | Bova C, Greco F, Misuraca G, et al. (2003). Diagnostic utility of echocardiography in patients with suspected pulmonary embolism. Am J Emerg Med., 21:1803. |
| [191] | Wan S, Quinlan DJ, Agnelli G, Eikelboom JW. (2004). Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta-analysis of the randomized controlled trials. Circulation, 110:7449. |
| [192] | Goldhaber SZ, Haire WD, Feldstein ML, et al. (1993). Alteplase versus heparin in acute pulmonary embolism: randomised trial assessing right-ventricular function and pulmonary perfusion. Lancet, 341:50711. |
| [193] | JanataK, Holzer M, Kurkciyan I, et al. (2003). Major bleeding complications in cardiopulmonary resuscitation: the place of thrombolytic therapy in cardiac arrest due to massive pulmonary embolism. Resuscitation, 57:4955. |
| [194] | Yousuf T, Brinton T, Ahmed K, et al. (2016). Tissue plasminogen activator use in cardiac arrest secondary to fulminant pulmonary embolism. J Clin Med Res., 8:1905. |
| [195] | Böttiger BW, Böhrer H, Bach A, Motsch J, Martin E. (1994). Bolus injection of thrombolytic agents during cardiopulmonary resuscitation for massive pulmonary embolism. Resuscitation, 28:4554. |
| [196] | Penney DJ, Stewart AHL, Parr MJA. (2002). Prognostic outcome indicators following hanging injuries. Resuscitation, 54:279. |
| [197] | Wu JP, Gu DY, Wang S, et al. (2014). Good neurological recovery after rescue thrombolysis of presumed pulmonary embolism despite prior 100 minutes CPR. J Thorac Dis., 6: E28993. |
| [198] | Summers K, Schultheis J, Raiff D, Dahhan T. (2019). Evaluation of rescue thrombolysis in cardiac arrest secondary to suspected or confirmed pulmonary embolism. Ann Pharmacother., 53:7115. |
| [199] | Doerge HC, Schoendube FA, Loeser H, Walter M, Messmer BJ. (1996). Pulmonary embolectomy: review of a 15-year experience and role in the age of thrombolytic therapy. Eur J Cardiothorac Surg., 10:9527. |
| [200] | Konstantinov IE, Saxena P, Koniuszko MD, Alvarez J, Newman MA. (2007). Acute massive pulmonary embolism with cardiopulmonary resuscitation: management and results. Tex Heart Inst J., 34:415 discussion 56. |
| [201] | Fava M, Loyola S, Bertoni H, Dougnac A. (2005). Massive pulmonary embolism: percutaneous mechanical thrombectomy during cardiopulmonary resuscitation. J Vasc Interv Radiol., 16: 11923. |
| [202] | Conrad SA, Broman LM, Taccone FS, et al. (2018). The Extracorporeal Life Support Organization Maastricht Treaty for nomenclature in extracorporeal life support. A position paper of the Extracorporeal Life Support Organization. Am J Respir Crit Care Med., 198: 44751. |
| [203] | Maj G, Melisurgo G, De Bonis M, Pappalardo F. (2014). ECLS management in pulmonary embolism with cardiac arrest: which strategy is better? Resuscitation, 85:e1756. |
| [204] | Swol J, Buchwald D, Strauch J, Schildhauer TA. (2016). Extracorporeal life support (ECLS) for cardiopulmonary resuscitation (CPR) with pulmonary embolism in surgical patients—a case series. Perfusion, 31:549. |
| [205] | Soar J, Maconochie I, Wyckoff MH, et al. (2019). International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation, 140: e826e80. |
| [206] | Hayashi M, Shimizu W, Albert CM. (2015). The spectrum of epidemiology underlying sudden cardiac death. Circ Res., 116:1887906. |
| [207] | Wee JH, Park JH, Choi SP, Park KN. (2013). Outcomes of patients admitted for hanging injuries with decreased consciousness but without cardiac arrest. Am J Emerg Med., 31:166670. |
| [208] | Myat A, Song KJ, Rea T. (2018). Out-of-hospital cardiac arrest: current concepts. Lancet, 391:9709. |
| [209] | Myerburg RJ, Junttila MJ. (2012). Sudden cardiac death caused by coronary heart disease. Circulation, 125:104352. |
| [210] | Yannopoulos D, Bartos JA, Aufderheide TP, et al. (2019). The evolving role of the cardiac catheterization laboratory in the management of patients with out-of-hospital cardiac arrest: a scientific statement from the American Heart Association. Circulation, 139: e530e52. |
| [211] | Nikolaou NI, Welsford M, Beygui F, et al. (2015). Part 5: acute coronary syndromes: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation, 95:e12146. |
| [212] | Roffi M, Patrono C, Collet JP, et al. (2016). 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J., 37:267315. |
| [213] | Ibanez B, James S, Agewall S, et al. (2018). 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J., 39:11977. |
| [214] | Piepoli MF, Hoes AW, Agewall S, et al. (2016). 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) seveloped with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J., 37:231581. |
| [215] | Noc M, Fajadet J, Lassen JF, et al. (2014). Invasive coronary treatment strategies for out-of-hospital cardiac arrest: a consensus statement from the European association for percutaneous cardiovascular interventions (EAPCI)/stent for life (SFL) groups. EuroIntervention, 10:317. |
| [216] | Kotseva K, De Backer G, De Bacquer D, et al. (2019). Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol., 26:82435. |
| [217] | Rauch B, Davos CH, Doherty P, et al. (2016). The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: a systematic review and meta-analysis of randomized and nonrandomized studies—the Cardiac Rehabilitation Outcome Study (CROS). Eur J Prev Cardiol., 23:191439. |
| [218] | MuraroA, Roberts G, Worm M, et al. (2014). Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy, 69:102645. |
| [219] | Ruano-Ravina A, Pena-Gil C, Abu-Assi E, et al. (2016). Participation and adherence to cardiac rehabilitation programs. A systematic review. Int J Cardiol., 223:43643. |
| [220] | Kotseva K, Wood D, De Bacquer D, Investigators E. (2018). Determinants of participation and risk factor control according to attendance in cardiac rehabilitation programmes in coronary patients in Europe: EUROASPIRE IV survey. Eur J Prev Cardiol., 25:124251. |
| [221] | Piepoli MF, Corra U, Dendale P, et al. (2016). Challenges in secondary prevention after acute myocardial infarction: a call for action. Eur J Prev Cardiol., 23:19942006. |
| [222] | Priori SG, Blomstrom-Lundqvist C, Mazzanti A, et al. (2015). 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J., 36:2793867. |
| [223] | Cartledge S, Bray JE, Leary M, Stub D, Finn J. (2016). A systematic review of basic life support training targeted to family members of high-risk cardiac patients. Resuscitation, 105:708. |
| [224] | Cartledge S, Finn J, Bray JE, et al. (2018). Incorporating cardiopulmonary resuscitation training into a cardiac rehabilitation programme: a feasibility study. Eur J Cardiovasc Nurs., 17:14858. |
| [225] | Gonzalez-Salvado V, Abelairas-Gomez C, Gude F, et al. (2019). Targeting relatives: impact of a cardiac rehabilitation programme including basic life support training on their skills and attitudes. Eur J Prev Cardiol., 26:795805. |
| [226] | Kalla K, Christ G, Karnik R, et al. (2006). Implementation of guidelines improves the standard of care: the Viennese registry on reperfusion strategies in ST-elevation myocardial infarction (Vienna STEMI registry). Circulation, 113: 2398405. |
| [227] | Ting HH, Rihal CS, Gersh BJ, et al. (2007). Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the Mayo Clinic STEMI protocol. Circulation, 116:72936. |
| [228] | Glickman SW, Lytle BL, Ou FS, et al. (2011). Care processes associated with quicker door-in-door-out times for patients with ST-elevationmyocardial infarction requiring transfer: results from a statewide regionalization program. Circ Cardiovasc Qual Outcomes, 4:3828. |
| [229] | Kleber C, Giesecke MT, Lindner T, Haas NP, Buschmann CT. (2014). Requirement for a structured algorithm in cardiac arrest following major trauma: epidemiology, management errors, and preventability of traumatic deaths in Berlin. Resuscitation, 85:40510. |
| [230] | Cequier A, Ariza-Sole A, Elola FJ, et al. (2017). Impact on mortality of different network systems in the treatment of ST-segment elevation acute myocardial infarction. The Spanish experience. Rev Esp Cardiol (Engl Ed), 70:15561. |
| [231] | Jollis JG, Al-Khalidi HR, Roettig ML, et al. (2018). Impact of regionalization of ST-segment-elevation myocardial infarction care on treatment times and outcomes for emergency medical services-transported patients presenting to hospitals with percutaneous coronary intervention: mission: lifeline accelerator-2. Circulation, 137:37687. |
| [232] | Filgueiras Filho NM, Feitosa Filho GS, Solla DJF, et al. (2018). Implementation of a regional network for ST-Segment-Elevation Myocardial Infarction (STEMI) care and 30-day mortality in a low- to middle-income city in Brazil: findings from Salvador’s STEMI Registry (RESISST). J Am Heart Assoc., 7: |
| [233] | Cequier A, Perez de Prado A, Moreno R, et al. (2019). Percutaneous cardiological intervention and cardiac surgery: patient-centered care. Position statement of the Spanish Society of Cardiology. Rev Esp Cardiol (Engl Ed), 72: 65863. |
| [234] | Peberdy MA, Donnino MW, Callaway CW, et al. (2013). Impact of percutaneous coronary intervention performance reporting on cardiac resuscitation centers: a scientific statement from the American Heart Association. Circulation, 128:76273. |
| [235] | Salam I, Hassager C, Thomsen JH, et al. (2016). Editor’s choice-is the prehospital ECG after out-of-hospital cardiac arrest accurate for the diagnosis of ST-elevation myocardial infarction? Eur Heart J Acute Cardiovasc Care, 5:31726. |
| [236] | Zanuttini D, Armellini I, Nucifora G, et al. (2013). Predictive value of electrocardiogram in diagnosing acute coronary artery lesions among patients with out-of-hospital-cardiac-arrest. Resuscitation, 84:12504. |
| [237] | Millin MG, Comer AC, Nable JV, et al. (2016). Patients without ST elevation after return of spontaneous circulation may benefit from emergent percutaneous intervention: a systematic review and meta-analysis. Resuscitation, 108:5460. |
| [238] | Barbarawi M, Zayed Y, Kheiri B, et al. (2019). Optimal timing of coronary intervention in patients resuscitated from cardiac arrest without STsegment elevation myocardial infarction (NSTEMI): a systematic review and meta-analysis. Resuscitation, 144:13744. |
| [239] | Lemkes JS, Janssens GN, van der Hoeven NW, et al. (2019). Coronary angiography after cardiac arrest without ST-segment elevation. N Engl J Med., 380:1397407. |
| [240] | Brenner ML, Moore LJ, DuBose JJ, et al. (2013). A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation. J Trauma Acute Care Surg., 75:50611. |
| [241] | Nolan JP, Böttiger BW, Cariou A, et al. (2021). European Resuscitation Council andEuropeanSociety of Intensive Care Medicine Guidelines 2021: post-resuscitation care. Resuscitation, 161. |
| [242] | Mentzelopoulos SD, Couper K, Van de Voorde P, et al. (2021). European Resuscitation Council Guidelines 2021: Ethics of resuscitation and end of life decisions resuscitation. 161. |
| [243] | Wang PL, Brooks SC. (2018). Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst Rev., 8: CD007260. |
| [244] | Holmberg MJ, Geri G, Wiberg S, et al. (2018). Extracorporeal cardiopulmonary resuscitation for cardiac arrest: a systematic review. Resuscitation, 131:91100. |
| [245] | Bougouin W, Dumas F, Lamhaut L, et al. (2020). Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur Heart J., 41: 196171. |
| [246] | Roberts DJ, Leigh-Smith S, Faris PD, et al. (2015). Clinical presentation of patients with tension pneumothorax: a systematic review. Ann Surg., 261:106878. |
| [247] | Hilbert-Carius P, Wurmb T, Lier H, et al. (2017). Care for severely injured persons: update of the 2016 S3 guideline for the treatment of polytrauma and the severely injured. Anaesthesist., 66: 195206. |
| [248] | Laan DV, Vu TD, Thiels CA, et al. (2016). Chest wall thickness and decompression failure: a systematic review and meta-analysis comparing anatomic locations in needle thoracostomy. Injury, 47:797804. |
| [249] | Holcomb JB, McManus JG, Kerr ST, Pusateri AE. (2009). Needle versus tube thoracostomy in a swine model of traumatic tension hemopneumothorax. Prehosp Emerg Care, 13:1827. |
| [250] | High K, Brywczynski J, Guillamondegui O. (2016). Safety and efficacy of thoracostomy in the air medical environment. Air Med. J., 35:22730. |
| [251] | Zwingmann J, Mehlhorn AT, Hammer T, et al. (2012). Survival and neurologic outcome after traumatic out-of-hospital cardiopulmonary arrest in a pediatric and adult population: a systematic review. Crit Care, 16:R117. |
| [252] | Mowry JB, Spyker DA, Cantilena Jr LR, McMillan N, Ford M. (2014). 2013 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 31st annual report. Clin Toxicol (Phila), 52: 1032283. |
| [253] | Gummin DD, Mowry JB, Spyker DA, et al. (2019). 2018 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 36th annual report. Clin Toxicol (Phila), 57:1220413. |
| [254] | Park JH, Shin SD, Song KJ, et al. (2012). Epidemiology and outcomes of poisoning-induced out-of-hospital cardiac arrest. Resuscitation, 83:517. |
| [255] | Safranek DJ, Eisenberg MS, Larsen MP. (1992). The epidemiology of cardiac arrest in young adults. Ann Emerg Med., 21:11026. |
| [256] | Engdahl J, Bang A, Karlson BW, Lindqvist J, Herlitz J. (2003). Characteristics and outcome among patients suffering from out of hospital cardiac arrest of non-cardiac aetiology. Resuscitation, 57:3341. |
| [257] | Hess EP, Campbell RL, White RD. (2007). Epidemiology, trends, and outcome of out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation, 72:2006. |
| [258] | Yanagawa Y, Sakamoto T, Okada Y. (2007). Recovery from a psychotropic drug overdose tends to depend on the time from ingestion to arrival, the Glasgow Coma Scale, and a sign of circulatory insufficiency on arrival. Am J Emerg Med., 25:75761. |
| [259] | Thompson TM, Theobald J, Lu J, Erickson TB. (2014). The general approach to the poisoned patient. Dis Mon., 60:50924. |
| [260] | Kim M, Shin SD, Jeong S, Kwak YH, Suh GJ. (2017). Poisoning-induced outof-hospital cardiac arrest and outcomes according to poison agent. J Korean Med Sci., 32:204250. |
| [261] | Graudins A, Lee HM, Druda D. (2016). Calcium channel antagonist and betablocker overdose: antidotes and adjunct therapies. Br J Clin Pharmacol., 81:45361. |
| [262] | Leis CC, Hernandez CC, Blanco MJ, et al. (2013). Traumatic cardiac arrest: should advance life support be initiated? J Trauma Acute Care Surg., 74:6348. |
| [263] | Gosselin S, Hoegberg LC, Hoffman RS, et al. (2016). Evidence-based recommendations on the use of intravenous lipid emulsion therapy in poisoning. Clin Toxicol (Phila), 54:899923. |
| [264] | Lam SH, Majlesi N, Vilke GM. (2016). Use of intravenous fat emulsion in the emergency department for the critically ill poisoned patient. J Emerg Med., 51:20314. |
| [265] | Cao D, Heard K, Foran M, Koyfman A. (2015). Intravenous lipid emulsion in the emergency department: a systematic review of recent literature. J Emerg Med., 48:38797. |
| [266] | de Lange DW, Sikma MA, Meulenbelt J. (2013). Extracorporeal membrane oxygenation in the treatment of poisoned patients. ClinToxicol(Phila), 51:38593. |
| [267] | Masson R, Colas V, Parienti JJ, et al. (2012). A comparison of survival with and without extracorporeal life support treatment for severe poisoning due to drug intoxication. Resuscitation, 83:14137. |
| [268] | Benson BE, Hoppu K, Troutman WG, et al. (2013). Position paper update: gastric lavage for gastrointestinal decontamination. Clin Toxicol (Phila), 51:1406. |
| [269] | Seger D. (2004). Single-dose activated charcoal-backup and reassess. J Toxicol Clin Toxicol., 42:10110. |
| [270] | Chyka PA, Seger D, Krenzelok EP, Vale JA. (2005). Position paper: singledose activated charcoal. Clin Toxicol (Phila), 43:6187. |
| [271] | Thanacoody R, Caravati EM, Troutman B, et al. (2015). Position paper update: whole bowel irrigation for gastrointestinal decontamination of overdose patients. Clin Toxicol (Phila), 53:512. |
| [272] | Krenzelok EP. (2005). Ipecac syrup-induced emesis . . . no evidence of benefit. Clin Toxicol (Phila), 43:112. |
| [273] | Olasveengen TM, Mancini ME, Perkins GD, et al. (2020). Adult basic life support: International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation, 156:A3579. |
| [274] | Bulger EM, Perina DG, Qasim Z, et al. (2019). Clinical use of resuscitative endovascular balloon occlusion of the aorta (REBOA) in civilian trauma systems in the USA, 2019: a joint statement from the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, the National Association of Emergency Medical Services Physicians and the National Association of Emergency Medical Technicians. Trauma Surg Acute Care Open, 4:e000376. |
| [275] | Brahmi N, Kouraichi N, Thabet H, Amamou M. (2006). Influence of activated charcoal on the pharmacokinetics and the clinical features of carbamazepine poisoning. Am J Emerg Med., 24: 4403. |
| [276] | Skinner CG, Chang AS, Matthews AS, Reedy SJ, Morgan BW. (2012). Randomized controlled study on the use of multiple-dose activated charcoal in patients with supratherapeutic phenytoin levels. Clin Toxicol (Phila), 50:7649. |
| [277] | Liss DB, Schwarz ES, Mullins ME. (2017). Sodium acetate infusion for serum and urine alkalinization. Ann Emerg Med., 70:6012. |
| [278] | Proudfoot AT, Krenzelok EP, Vale JA. (2004). Position paper on urine alkalinization. J Toxicol Clin Toxicol., 42:126. |
| [279] | Sun X, Chen X, Lu J, et al. (2019). Extracorporeal treatment in children with acute severe poisoning. Medicine (Baltimore), 98:e18086. |
| [280] | Haines JA, Jacobsen D, Meredith T, Pronczuk de Garbino J. (1997). International programme on chemical safety — antidotes project. J Toxicol Clin Toxicol., 35:1256. |
| [281] | Betten DP, Vohra RB, Cook MD, Matteucci MJ, Clark RF. (2006). Antidote use in the critically ill poisoned patient. J Intensive Care Med., 21:25577. |
| [282] | Forster V, Leroux JC. (2015). Nano-antidotes for drug overdose and poisoning. Sci Transl Med., 7:290ps14. |
| [283] | Eddleston M, Rajapakse S, Rajakanthan, et al. (2000). Anti-digoxin Fab fragments in cardiotoxicity induced by ingestion of yellow oleander: a randomised controlled trial. Lancet, 355:96772. |
| [284] | Lapostolle F, Borron SW, Verdier C, et al. (2008). Digoxin-specific Fab fragments as single first-line therapy in digitalis poisoning. Crit Care Med., 36:30148. |
| [285] | Schimrigk J, Baulig C, Buschmann C, et al. (2020). Indications, procedure and outcome of prehospital emergency resuscitative thoracotomy-a systematic literature search. Unfallchirurg, 123:71123. |
| [286] | Henry M, Kay MM, Viccellio P. (1985). Cardiogenic shock associated with calcium-channel and beta blockers: reversal with intravenous calcium chloride. Am J Emerg Med., 3:3346. |
| [287] | Ramoska EA, Spiller HA, Winter M, Borys D. (1993). A one-year evaluation of calcium channel blocker overdoses: toxicity and treatment. Ann Emerg Med., 22:196200. |
| [288] | Howarth DM, Dawson AH, Smith AJ, Buckley N, Whyte IM. (1994). Calcium channel blocking drug overdose: an Australian series. Hum Exp Toxicol., 13:1616. |
| [289] | Strubelt O, Diederich KW. (1990). Studies of antidote therapy for nisoldipine intoxication in experimental animals. Arzneimittelforschung, 40:74751. |
| [290] | Graudins A, Najafi J, Rur SM. (2008). Treatment of experimental verapamil poisoning with levosimendan utilizing a rodent model of drug toxicity. Clin Toxicol (Phila), 46:506. |
| [291] | Graudins A, Wong KK. (2010). Comparative hemodynamic effects of levosimendan alone and in conjunction with 4-aminopyridine or calcium chloride in a rodent model of severe verapamil poisoning. J Med Toxicol., 6:8593. |
| [292] | Greene SL, Gawarammana I, Wood DM, Jones AL, Dargan PI. (2007). Relative safety of hyperinsulinaemia / euglycaemia therapy in the management of calcium channel blocker overdose: a prospective observational study. Intensive Care Med., 33:201924. |
| [293] | Yuan TH, Kerns WPI, Tomaszewski CA, Ford MD, Kline JA. (1999). Insulinglucose as adjunctive therapy for severe calcium channel antagonist poisoning. J Toxicol Clin Toxicol., 37:46374. |
| [294] | Boyer EW, Shannon M. (2001). Treatment of calcium-channel-blocker intoxication with insulin infusion. N Engl J Med., 344: 17212. |
| [295] | Espinoza TR, Bryant SM, Aks SE. (2013). Hyperinsulin therapy for calcium channel antagonist poisoning: a seven-year retrospective study. Am J Ther., 20:2931. |
| [296] | Seamon MJ, Chovanes J, Fox N, et al. (2012). The use of emergency department thoracotomy for traumatic cardiopulmonary arrest. Injury, 43:135561. |
| [297] | Kline JA, Leonova E, Raymond RM. (1995). Beneficial myocardial metabolic effects of insulin during verapamil toxicity in the anesthetized canine. Crit Care Med., 23:125163. |
| [298] | Kline JA, Raymond RM, Leonova ED, Williams TC, Watts JA. (1997). Insulin improves heart function and metabolism during non-ischemic cardiogenic shock in awake canines. Cardiovasc Res., 34: 28998. |
| [299] | Engebretsen KM, Kaczmarek KM, Morgan J, Holger JS. (2011). High-dose insulin therapy in beta-blocker and calcium channel-blocker poisoning. Clin Toxicol (Phila), 49:27783. |
| [300] | Holger JS, Stellpflug SJ, Cole JB, Harris CR, Engebretsen KM. (2011). Highdose insulin: a consecutive case series in toxin-induced cardiogenic shock. Clin Toxicol (Phila), 49:6538. |
| [301] | McGlinchey PG, McNeill AJ. (1998). Drug overdoses requiring temporary cardiac pacing; a study of six cases treated at Altnagelvin Hospital, Londonderry. Ulster Med J., 67:138. |
| [302] | Perichon D, Turfus S, Gerostamoulos D, Graudins A. (2013). An assessment of the in vivo effects of intravenous lipid emulsion on blood drug concentration and haemodynamics following oro-gastric amitriptyline overdose. Clin Toxicol (Phila), 51:20815. |
| [303] | Escajeda JT, Katz KD, Rittenberger JC. (2015). Successful treatment of metoprolol-induced cardiac arrest with high-dose insulin, lipid emulsion, and ECMO. Am J Emerg Med., 33: 1111 e14. |
| [304] | Kerns 2nd W, Schroeder D, Williams C, Tomaszewski C, Raymond R. (1997). Insulin improves survival in a canine model of acute beta-blocker toxicity. Ann Emerg Med., 29:74857. |
| [305] | Cole JB, Arens AM, Laes JR, et al. (2018). High dose insulin for beta-blocker and calcium channel-blocker poisoning. Am J Emerg Med., 36:181724. |
| [306] | Fernandes CM, Daya MR. (1995). Sotalol-induced bradycardia reversed by glucagon. Can Fam Physician, 41:65960 63-5. |
| [307] | Escutnaire J, Genin M, Babykina E, et al. (2018). Traumatic cardiac arrest is associated with lower survival rate vs. medical cardiac arrest— results from the French National Registry. Resuscitation, 131:4854. |
| [308] | Bailey B. (2003). Glucagon in beta-blocker and calcium channel blocker overdoses: a systematic review. J Toxicol Clin Toxicol., 41: 595602. |
| [309] | West PL, McKeown NJ, Hendrickson RG. (2010). Iatrogenic lipid emulsion overdose in a case of amlodipine poisoning. Clin Toxicol (Phila), 48:3936. |
| [310] | Kollef MH. (1994). Labetalol overdose successfully treated with amrinone and alpha-adrenergic receptor agonists. Chest, 105: 6267. |
| [311] | Sasyniuk BI, Jhamandas V, Valois M. (1986). Experimental amitriptyline intoxication: treatment of cardiac toxicity with sodium bicarbonate. Ann Emerg Med., 15:10529. |
| [312] | Knudsen K, Abrahamsson J. (1997). Epinephrine and sodium bicarbonate independently and additively increase survival in experimental amitriptyline poisoning. Crit Care Med., 25:66974. |
| [313] | Bradberry SM, Thanacoody HK, Watt BE, Thomas SH, Vale JA. (2005). Management of the cardiovascular complications of tricyclic antidepressant poisoning: role of sodium bicarbonate. Toxicol Rev., 24: 195204. |
| [314] | Gunja N, Graudins A. (2011). Management of cardiac arrest following poisoning. EMA: Emerg Med Australas, 23:1622. |
| [315] | Boehnert MT, Lovejoy Jr FH. (1985). Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med., 313:4749. |
| [316] | Bou-Abboud E, Nattel S. (1996). Relative role of alkalosis and sodium ions in reversal of class I antiarrhythmic drug-induced sodium channel blockade by sodium bicarbonate. Circulation, 94:195461. |
| [317] | McCabe JL, Cobaugh DJ, Menegazzi JJ, Fata J. (1998). Experimental tricyclic antidepressant toxicity: a randomized, controlled comparison of hypertonic saline solution, sodium bicarbonate, and hyperventilation. Ann Emerg Med., 32:32933. |
| [318] | Beck B, Tohira H, Bray JE, et al. (2016). Trends in traumatic out-of-hospital cardiac arrest in Perth, Western Australia from 1997 to 2014. Resuscitation, 98:7984. |
| [319] | Pileggi DJ, Cook AM. (2016). Neuroleptic malignant syndrome. Ann Pharmacother., 50:97381. |
| [320] | Barelli A, Botti P, Della Puppa T. TBST (Toxicological Basic Support and Therapy). (2010). Bologna: Italian Resuscitation Council; 2010. |
| [321] | Roberge RJ, Francis 3rd EH. (2002). Use of naloxone in valproic acid overdose: case report and review. J Emerg Med., 22:6770. |
| [322] | Sztajnkrycer MD. (2002). Valproic acid toxicity: overview and management. J Toxicol Clin Toxicol., 40:789801. |
| [323] | Ghannoum M, Yates C, Galvao TF, et al. (2014). Extracorporeal treatment for carbamazepine poisoning: systematic review and recommendations from theEXTRIP workgroup. ClinToxicol (Phila), 52:9931004. |
| [324] | Sivilotti ML. (2016). Flumazenil, naloxone and the ‘coma cocktail’. Br J Clin Pharmacol., 81:42836. |
| [325] | Penninga EI, Graudal N, Ladekarl MB, Jurgens G. (2016). Adverse events associated with flumazenil treatment for the management of suspected benzodiazepine intoxication—a systematic review with meta-analyses of randomised trials. Basic Clin Pharmacol Toxicol., 118:3744. |
| [326] | Hiller DB, Gregorio GD, Ripper R, et al. (2009). Epinephrine impairs lipid resuscitation from bupivacaine overdose: a threshold effect. Anesthesiology, 111:498505. |
| [327] | Carreiro S, Blum J, Jay G, Hack JB. (2013). Intravenous lipid emulsion alters the hemodynamic response to epinephrine in a rat model. J Med Toxicol., 9:2205. |
| [328] | Litz Rj, Popp M, Stehr Sn, Koch T. (2006). Successful resuscitation of a patient with ropivacaine-induced asystole after axillary plexus block using lipid infusion. Anaesthesia, 61:8001. |
| [329] | Evans CC, Petersen A, Meier EN, et al. (2016). Prehospital traumatic cardiac arrest: management and outcomes from the resuscitation outcomes consortium epistry-trauma and PROPHET registries. J Trauma Acute Care Surg., 81:28593. |
| [330] | Rosenblatt Ma, Abel M, Fischer Gw, Itzkovich Cj, Eisenkraft Jb. (2006). Successful use of a 20% lipid emulsion to resuscitate a patient after a presumed bupivacaine-related cardiac arrest. Anesthesiology, 105:2178. |
| [331] | Ludot H, Tharin JY, Belouadah M, Mazoit JX, Malinovsky JM. (2008). Successful resuscitation after ropivacaine and lidocaine-induced ventricular arrhythmia following posterior lumbar plexus block in a child. Anesth Analg., 106:15724 table of contents. |
| [332] | American College of Medical Toxicology. (2011). ACMT position statement: interim guidance for the use of lipid resuscitation therapy. J Med Toxicol., 7:812. |
| [333] | Hicks SD, Salcido DD, Logue ES, et al. (2009). Lipid emulsion combined with epinephrine and vasopressin does not improve survival in a swine model of bupivacaine-induced cardiac arrest. Anesthesiology, 111:13846. |
| [334] | Chou R, Korthuis PT, McCarty D, et al. (2017). Management of suspected opioid overdose with naloxone in out-of-hospital settings: a systematic review. Ann Intern Med., 167:86775. |
| [335] | Gufford BT, Ainslie GR, White Jr JR, et al. (2017). Comparison of a new intranasal naloxone formulation to intramuscular naloxone: results from hypothesis-generating small clinical studies. Clin Transl Sci., 10:3806. |
| [336] | Honderick T, Williams D, Seaberg D, Wears R. (2003). A prospective, randomized, controlled trial of benzodiazepines and nitroglycerine or nitroglycerine alone in the treatment of cocaine-associated acute coronary syndromes. Am J Emerg Med., 21:3942. |
| [337] | Saland KE, Hillis LD, Lange RA, Cigarroa JE. (2002). Influence of morphine sulfate on cocaine-induced coronary vasoconstriction. Am J Cardiol., 90:8101. |
| [338] | Lange RA, Cigarroa RG, Yancy Jr CW, et al. (1989). Cocaine-induced coronary-artery vasoconstriction. N Engl J Med., 321:155762. |
| [339] | Negus BH, Willard JE, Hillis LD, et al. (1994). Alleviation of cocaine-induced coronary vasoconstriction with intravenous verapamil. Am J Cardiol., 73:5103. |
| [340] | Barnard E, Yates D, Edwards A, et al. (2017). Epidemiology and aetiology of traumatic cardiac arrest in England and Wales—a retrospective database analysis. Resuscitation, 110:904. |
| [341] | Baumann BM, Perrone J, Hornig SE, Shofer FS, Hollander JE. (2000). Randomized, double-blind, placebo-controlled trial of diazepam, nitroglycerin, or both for treatment of patients with potential cocaine-associated acute coronary syndromes. Acad Emerg Med., 7:87885. |
| [342] | Hollander JE, Hoffman RS, Gennis P, et al. (1994). Nitroglycerin in the treatment of cocaine associated chest pain—clinical safety and efficacy. J Toxicol Clin Toxicol., 32:24356. |
| [343] | Pham D, Addison D, Kayani W, et al. (2018). Outcomes of beta blocker use in cocaine-associated chest pain: a meta-analysis. Emerg Med., 35:55963. |
| [344] | Richards JR, Garber D, Laurin EG, et al. (2016). Treatment of cocaine cardiovascular toxicity: a systematic review. Clin Toxicol., (Phila), 54:34564. |
| [345] | King A, Dimovska M, Bisoski L. (2018). Sympathomimetic toxidromes and other pharmacological causes of acute hypertension. Curr Hypertens Rep., 20:8. |
| [346] | Graudins A, Stearman A, Chan B. (1998). Treatment of the serotonin syndrome with cyproheptadine. J Emerg Med., 16:6159. |
| [347] | Mason PJ, Morris VA, Balcezak TJ. (2000). Serotonin syndrome. Presentation of 2 cases and review of the literature. Medicine (Baltimore), 79:2019. |
| [348] | Gillman PK. (1997). Serotonin syndrome treated with chlorpromazine. J Clin Psychopharmacol., 17:1289. |
| [349] | Richelson E, Souder T. (2000). Binding of antipsychotic drugs to human brain receptors focus on newer generation compounds. Life Sci., 68:2939. |
| [350] | Fortin JL, Desmettre T, Manzon C, et al. (2010). Cyanide poisoning and cardiac disorders: 161 cases. J Emerg Med., 38:46776. |
| [351] | Zwingmann J, Lefering R, Feucht M, et al. (2016). Outcome and predictors for successful resuscitation in the emergency room of adult patients in traumatic cardiorespiratory arrest. Crit Care, 20:282. |
| [352] | BebartaVS, Tanen DA, Lairet J, et al. (2010). Hydroxocobalamin and sodium thiosulfate versus sodium nitrite and sodium thiosulfate in the treatment of acute cyanide toxicity in a swine (Sus scrofa) model. Ann Emerg Med., 55:34551. |
| [353] | MacLennan L, Moiemen N. (2015). Management of cyanide toxicity in patients with burns. Burns, 41:1824. |
| [354] | Hall AH, Kulig KW, Rumack BH. (1989). Suspected cyanide poisoning in smoke inhalation: complications of sodium nitrite therapy. J Toxicol Clin Exp., 9:39. |
| [355] | Kirk MA, Gerace R, Kulig KW. (1993). Cyanide and methemoglobin kinetics in smoke inhalation victims treated with the cyanide antidote kit. Ann Emerg Med., 22:14138. |
| [356] | Weaver LK. (2009). Clinical practice. Carbon monoxide poisoning. N Engl J Med., 360:121725. |
| [357] | Betterman K, Patel S. (2014). Neurologic complications of carbon monoxide intoxication. Handb Clin Neurol., 120:9719. |
| [358] | Lin CH, Su WH, Chen YC, et al. (2018). Treatment with normobaric or hyperbaric oxygen and its effect on neuropsychometric dysfunction after carbon monoxide poisoning: a systematic review and metaanalysis of randomized controlled trials. Medicine (Baltimore), 97: e12456. |
| [359] | Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJ. (2011). Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev., CD002041. |
| [360] | Dries DJ, Endorf FW. (2013). Inhalation injury: epidemiology, pathology, treatment strategies. Scand J Trauma Resusc Emerg Med., 21:31. |
| [361] | Roderique JD, Josef CS, Feldman MJ, Spiess BD. (2015). A modern literature review of carbon monoxide poisoning theories, therapies, and potential targets for therapy advancement. Toxicology, 334:4558. |
| [362] | Spahn DR, Bouillon B, Cerny V, et al. (2019). The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care, 23:98. |
| [363] | Hoidal CR, Hall AH, Robinson MD, Kulig K, Rumack BH. (1986). Hydrogen sulfide poisoning from toxic inhalations of roofing asphalt fumes. Ann Emerg Med., 15:82630. |
| [364] | Hall AH, Rumack BH. (1997). Hydrogen sulfide poisoning: an antidotal role for sodium nitrite? Vet Hum Toxicol., 39:1524. |
| [365] | Cronican AA, Frawley KL, Ahmed H, Pearce LL, Peterson J. (2015). Antagonism of acute sulfide poisoning in mice by nitrite anion without methemoglobinemia. Chem Res Toxicol., 28: 1398408. |
| [366] | Bebarta VS, Garrett N, Brenner M, et al. (2017). Efficacy of intravenous cobinamide versus hydroxocobalamin or saline for treatment of severe hydrogen sulfide toxicity in a swine (Sus scrofa) model. Acad Emerg Med., 24:108898. |
| [367] | Rumbeiha W, Whitley E, Anantharam P, Kim DS, Kanthasamy A. (2016). Acute hydrogen sulfide-induced neuropathology and neurological sequelae: challenges for translational neuroprotective research. Ann N Y Acad Sci., 1378:516. |
| [368] | Rendell R, Fairhall S, Graham S, et al. (2018). Assessment of Nacetylcysteine as a therapy for phosgene-induced acute lung injury. Toxicol Lett., 290:14552. |
| [369] | Tormoehlen LM, Tekulve KJ, Nanagas KA. (2014). Hydrocarbon toxicity: a review. Clin Toxicol (Phila), 52:47989. |
| [370] | Dell’Aglio DM, Sutter ME, Schwartz MD, et al. (2010). Acute chloroform ingestion successfully treated with intravenously administered Nacetylcysteine. J Med Toxicol., 6:1436. |
| [371] | Robinson RF, Nahata MC. (2003). Management of botulism. Ann Pharmacother 2003; 37: 12731. |
| [372] | Sobel J. (2009). Diagnosis and treatment of botulism: a century later, clinical suspicion remains the cornerstone. Clin Infect Dis., 48:16745. |
| [373] | Cera SM, Mostafa G, Sing RF, et al. (2003). Physiologic predictors of survival in post-traumatic arrest. Am Surg., 69:1404. |
| [374] | Gerardo CJ, Quackenbush E, Lewis B, et al. (2017). the efficacy of crotalidae polyvalent immune fab (ovine) antivenom versus placebo plus optional rescue therapy on recovery from copperhead snake envenomation: a randomized, double-blind, placebo-controlled, clinical trial. Ann Emerg Med., 70: 233-44 e3. |
| [375] | Currie BJ, Jacups SP. (2005). Prospective study of Chironex fleckeri and other box jellyfish stings in the "top end" of Australia’s Northern Territory. Med J Aust., 183:6316. |
| [376] | Hinkelbein J, Andres J, Thies KC, DE Robertis E. (2017). Perioperative cardiac arrest in the operating room environment: a review of the literature. Minerva Anestesiol., 83:11908. |
| [377] | Hur M, Lee HC, Lee KH, et al. (2017). The incidence and characteristics of 3- month mortality after intraoperative cardiac arrest in adults. Acta Anaesthesiol Scand., 61:1095104. |
| [378] | Zuercher M, Ummenhofer W. (2008). Cardiac arrest during anesthesia. Curr Opin Crit Care, 14:26974. |
| [379] | Kaiser HA, Saied NN, Kokoefer AS, et al. (2020). Incidence and prediction of intraoperative and postoperative cardiac arrest requiring cardiopulmonary resuscitation and 30-day mortality in non-cardiac surgical patients. PLoS One, 15:e0225939. |
| [380] | Andres J, Hinkelbein J, Bottiger BW. (2013). The stepchild of emergency medicine: sudden unexpected cardiac arrest during anaesthesia— do we need anaesthesia-centred advanced life support guidelines? Eur J Anaesthesiol., 30:956. |
| [381] | Moitra VK, Gabrielli A, Maccioli GA, O’Connor MF. (2012). Anesthesia advanced circulatory life support. Can J Anaesth., 59:586603. |
| [382] | Moitra VK, Einav S, Thies KC, et al. (2018). Cardiac arrest in the operating room: resuscitation and management for the anesthesiologist: part 1. Anesth Analg., 126:87688. |
| [383] | Brown J, Rogers J, Soar J. (2001). Cardiac arrest during surgery and ventilation in the prone position: a case report and systematic review. Resuscitation, 50:2338. |
| [384] | Perkins GD, Graesner JT, Semeraro F, et al. (2021). European Resuscitation Council Guidelines 2021 — executive summary. Resuscitation, 161. |
| [385] | Stratton SJ, Brickett K, Crammer T. (1998). Prehospital pulseless, unconscious penetrating trauma victims: field assessments associated with survival. J Trauma., 45:96100. |
| [386] | Atkinson MC. (2000). The efficacy of cardiopulmonary resuscitation in the prone position. Crit Care Resusc., 2:18890. |
| [387] | Mertes PM, Tajima K, Regnier-Kimmoun MA, et al. (2010). Perioperative anaphylaxis. Med Clin North Am., 94:76189 xi. |
| [388] | Wolfe JW, Butterworth JF. (2011). Local anesthetic systemic toxicity: update on mechanisms and treatment. Curr Opin Anaesthesiol., 24:5616. |
| [389] | Waring WS. (2012). Intravenous lipid administration for drug-induced toxicity: a critical review of the existing data. Expert Rev Clin Pharmacol., 5:43744. |
| [390] | Neal JM, Mulroy MF, Weinberg GL, American Society of Regional A, Pain M.. (2012). American Society of Regional Anesthesia and Pain Medicine checklist for managing local anesthetic systemic toxicity: 2012 version. Reg Anesth Pain Med., 37:168. |
| [391] | Cave G, Harvey MG. (2014). Should we consider the infusion of lipid emulsion in the resuscitation of poisoned patients? Crit Care, 18:457. |
| [392] | Ozcan MS, Weinberg G. (2014). Intravenous lipid emulsion for the treatment of drug toxicity. J Intensive Care Med., 5970. |
| [393] | Meaney PA, Bobrow BJ, Mancini ME, et al. (2013). Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation, 128:41735. |
| [394] | Cingi EC, McMahon LA, Prielipp RC. (2016). Novel resuscitation devices facilitate complete neurologic recovery after prolonged cardiac arrest in postanesthesia care unit. J Clin Anesth., 35:5305. |
| [395] | Adam Z, Adam S, Everngam RL, et al. (2009). Resuscitation after cardiac surgery: results of an international survey. Eur J Cardiothorac Surg., 36:2934. |
| [396] | Chen YC, Wu KH, Hsiao KY, et al. (2019). Factors associated with outcomes in traumatic cardiac arrest patients without prehospital return of spontaneous circulation. Injury, 50:49. |
| [397] | LaPar DJ, Ghanta RK, Kern JA, et al. (2014). Hospital variation in mortality from cardiac arrest after cardiac surgery: an opportunity for improvement? Ann Thorac Surg., 98:5349 discussion 9-40. |
| [398] | Vakil K, Kealhofer JV, Alraies MC, et al. (2016)., Long-term outcomes of patients who had cardiac arrest after cardiac operations. Ann Thorac Surg., 102:5127. |
| [399] | Gupta P, Rettiganti M, Jeffries HE, et al. (2016). Risk factors and outcomes of in-hospital cardiac arrest following pediatric heart operations of varying complexity. Resuscitation, 105:17. |
| [400] | Soar J, Donnino MW, Maconochie I, et al. (2018). 2018 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations Summary. Resuscitation, 133:194206. |
| [401] | Clark Sc, Dunning J, Alfieri Or, et al. (2012). EACTS guidelines for the use of patient safety checklists. Eur J Cardiothorac Surg., 41: 9931004. |
| [402] | Dunning J, Fabbri A, Kolh PH, et al. (2009). Guideline for resuscitation in cardiac arrest after cardiac surgery. Eur J Cardiothorac Surg., 36:328. |
| [403] | Society of Thoracic Surgeons Task Force on Resuscitation After Cardiac S. (2017). The Society of Thoracic Surgeons expert consensus for the resuscitation of patients who arrest after cardiac surgery. Ann Thorac Surg., 103:100520. |
| [404] | Dunning J, Nandi J, Ariffin S, et al. (2006). The cardiac surgery advanced life support course (CALS): delivering significant improvements in emergency cardiothoracic care. Ann ThoracSurg., 81:176772. |
| [405] | Haynes AB, Weiser TG, Berry WR, et al. (2009). A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med., 360:4919. |
| [406] | Lomivorotov VV, Efremov SM, Kirov MY, Fominskiy EV, Karaskov AM. (2017). Low-cardiac-output syndrome after cardiac surgery. J Cardiothorac Vasc Anesth., 31:291308. |
| [407] | Seamon Mj, Haut Er, Van Arendonk K, et al. (2015). An evidence-based approach to patient selection for emergency department thoracotomy: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg., 79:15973. |
| [408] | Pagano D, Milojevic M, Meesters Mi, et al. (2018). 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery. Eur J Cardiothorac Surg., 53: 79111. |
| [409] | Brand J, McDonald A, Dunning J. (2018). Management of cardiac arrest following cardiac surgery. BJA Educ., 18:1622. |
| [410] | Flachskampf FA, Wouters, PF,EdvardsenT, et al. (2014). Recommendations for transoesophageal echocardiography: EACVI update 2014. Eur Heart J Cardiovasc Imaging., 15:35365. |
| [411] | Peretto G, Durante A, Limite LR, Cianflone D. (2014). Postoperative arrhythmias after cardiac surgery: incidence, risk factors, and therapeutic management. Cardiol Res Pract., 2014: 615987. |
| [412] | Lockowandt U, Levine A, Strang T, Dunning J. (2008). If a patient arrests after cardiac surgery is it acceptable to delay cardiopulmonary resuscitation until you have attempted either defibrillation or pacing? Interact Cardiovasc Thorac Surg., 7:87885. |
| [413] | Richardson L, Dissanayake A, Dunning J. (2007). What cardioversion protocol for ventricular fibrillation should be followed for patients who arrest shortly post-cardiac surgery? Interact Cardiovasc Thorac Surg., 6:799805. |
| [414] | International Consensus on Cardiopulmonary Resuscitation and Emergency. (2005). Cardiovascular Care Science with Treatment Recommendations. Part 4: advanced life support. Resuscitation, 67:21347. |
| [415] | Twomey D, Das M, Subramanian H, Dunning J. (2008). Is internal massage superior to external massage for patients suffering a cardiac arrest after cardiac surgery? Interact Cardiovasc Thorac Surg., 7:1516. |
| [416] | Tsagkataki M, Levine A, Strang T, Dunning J. (2008). Should adrenaline be routinely used by the resuscitation team if a patient suffers a cardiac arrest shortly after cardiac surgery? Interact Cardiovasc Thorac Surg., 7:45762. |
| [417] | Holmberg MJ, Issa MS, MoskowitzA, et al. (2019). Vasopressors during adult cardiac arrest: a systematic review and meta-analysis. Resuscitation, 139:10621. |
| [418] | Djarv T, Axelsson C, Herlitz J, et al. (2018). Traumatic cardiac arrest in Sweden 1990-2016—a population-based national cohort study. Scand J Trauma Resusc Emerg Med., 26:30. |
| [419] | Charalambous CP, Zipitis CS, Keenan DJ. (2006). Chest reexploration in the intensive care unit after cardiac surgery: a safe alternative to returning to the operating theater. Ann Thorac Surg., 81:1914. |
| [420] | Mackay JH, Powell SJ, Osgathorp J, Rozario CJ. (2002). Six-year prospective audit of chest reopening after cardiac arrest. Eur J Cardiothorac Surg., 22:4215. |
| [421] | Zhao Y, Xing J, Du Z, et al. (2015). Extracorporeal cardiopulmonary resuscitation for adult patients who underwent post-cardiac surgery. Eur J Med Res., 20:83. |
| [422] | Addala S, Kahn JK, Moccia TF, et al. (2005). Outcome of ventricular fibrillation developing during percutaneous coronary interventions in 19,497 patients without cardiogenic shock. Am J Cardiol., 96:7645. |
| [423] | Mehta RH, Starr AZ, Lopes RD, et al. (2009). Incidence of and outcomes associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention. JAMA, 301:177989. |
| [424] | Finn JC, Bhanji F, Lockey A, et al. (2015). Part 8: education, implementation, and teams: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation, 95:e20324. |
| [425] | Olasveengen TM, de Caen AR, Mancini ME, et al. (2017). 2017 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations Summary. Resuscitation, 121:20114. |
| [426] | Van de WalleS, LermanA, ChevalierB, et al. (2008). Constructing a checklist for the prevention of complications during percutaneous coronary intervention. EuroIntervention, 4:18992. |
| [427] | Naidu SS, Aronow HD, Box LC, et al. (2016). SCAI expert consensus statement: 2016 best practices in the cardiac catheterization laboratory: (endorsed by the Cardiological Society of India, and Sociedad Latino Americana de Cardiologia intervencionista; affirmation of value by the Canadian Association of Interventional Cardiology-Association canadienne de cardiologie d’intervention). Catheter Cardiovasc Interv., 88:40723. |
| [428] | Abrams D, Garan AR, Abdelbary A, et al. (2018). Position paper for the organization of ECMO programs for cardiac failure in adults. Intensive Care Med., 44:71729. |
| [429] | Israr S, Cook AD, Chapple KM, et al. (2019). Pulseless electrical activity following traumatic cardiac arrest: sign of life or death? Injury, 50:150710. |
| [430] | Cahill Tj, Clarke Sc, Simpson Ia, Stables Rh. (2015). A patient safety checklist for the cardiac catheterisation laboratory. Heart, 101:913. |
| [431] | Lindsay AC, Bishop J, Harron K, Davies S, Haxby E. (2018). Use of a safe procedure checklist in the cardiac catheterisation laboratory. BMJ Open Qual., 7:e000074. |
| [432] | Clattenburg EJ, Wroe PC, Gardner K, et al. (2018). Implementation of the Cardiac Arrest Sonographic Assessment (CASA) protocol for patients with cardiac arrest is associated with shorter CPR pulse checks. Resuscitation, 131:6973. |
| [433] | Lien WC, Hsu SH, Chong KM, et al. (2018). US-CAB protocol for ultrasonographic evaluation during cardiopulmonary resuscitation: validation and potential impact. Resuscitation, 127:12531. |
| [434] | Huis In’t Veld MA, Allison MG, Bostick DS, et al. (2017). Ultrasound use during cardiopulmonary resuscitation is associated with delays in chest compressions. Resuscitation, 119:958. |
| [435] | Parker BK, Salerno A, Euerle BD. (2019). The use of transesophageal echocardiography during cardiac arrest resuscitation: a literature review. J Ultrasound Med., 38:114151. |
| [436] | Fair J, Mallin M, Mallemat H, et al. (2018). Transesophageal echocardiography: guidelines for point-of-care applications in cardiac arrest resuscitation. Ann Emerg Med., 71:2017. |
| [437] | Vase H, Christensen S, Christiansen A, et al. (2017). The impella CP device for acute mechanical circulatory support in refractory cardiac arrest. Resuscitation, 112:704. |
| [438] | Garcia-Carreno J, Sousa-Casasnovas I, Devesa-Cordero C, et al. (2019). Cardiopulmonary resuscitation with percutaneous ECMO in refractory in-hospital cardiac arrest: a single-center experience. Rev Esp Cardiol (Engl Ed), 72:8802. |
| [439] | Arlt M, Philipp A, Voelkel S, et al. (2012). Early experiences with miniaturized extracorporeal life-support in the catheterization laboratory. Eur J Cardiothorac Surg., 42:85863. |
| [440] | Millin MG, Galvagno SM, Khandker SR, et al. (2013). Withholding and termination of resuscitation of adult cardiopulmonary arrest secondary to trauma: resource document to the joint NAEMSPACSCOT position statements. J Trauma Acute Care Surg., 75:45967. |
| [441] | Guglin M, Zucker MJ, Bazan VM, et al. (2019). Venoarterial ECMO for adults: JACC scientific expert panel. J Am Coll Cardiol., 73:698716. |
| [442] | D’Arrigo S, Cacciola S, Dennis M, et al. (2017). Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and metaanalysis. Resuscitation, 121:6270. |
| [443] | Makar MS, Pun PH. (2017). Sudden cardiac death among hemodialysis patients. Am J Kidney Dis., 69:68495. |
| [444] | Karnik JA, Young BS, Lew NL, et al. (2001). Cardiac arrest and sudden death in dialysis units. Kidney Int., 60:3507. |
| [445] | Davis, TR, Young, BA., Eisenberg, MS., et al.(2008). Outcome of cardiac arrests attended by emergency medical services staff at community outpatient dialysis centers. Kidney Int., 73:9339. |
| [446] | Lafrance JP, Nolin L, Senecal L, Leblanc M. (2006). Predictors and outcome of cardiopulmonary resuscitation (CPR) calls in a large haemodialysis unit over a seven-year period. Nephrol DialTransplant., 21:100612. |
| [447] | Bleyer AJ, Hartman J, Brannon PC, et al. (2006). Characteristics of sudden death in hemodialysis patients. Kidney Int., 69:226873. |
| [448] | Pun PH, Lehrich RW, Honeycutt EF, Herzog CA, Middleton JP. (2011). Modifiable risk factors associated with sudden cardiac arrest within hemodialysis clinics. Kidney Int., 79:21827. |
| [449] | Starks MA, Wu J, Peterson ED, et al. (2020). In-hospital cardiac arrest resuscitation practices and outcomes in maintenance dialysis patients. Clin J Am Soc Nephrol., 15:21927. |
| [450] | Bander Sj, Walters Ba. (1998). Hemodialysis morbidity and mortality: links to patient non-compliance. Curr Opin Nephrol Hypertens., 7:64953. |
| [451] | Luna, GK., Pavlin, EG., Kirkman T, Copass MK, Rice CL. (1989). Hemodynamic effects of external cardiac massage in trauma shock. J Trauma, 29:14303. |
| [452] | Kovesdy CP, Regidor DL, Mehrotra R, et al. (2007). Serum and dialysate potassium concentrations and survival in hemodialysis patients. Clin J Am Soc Nephrol., 2:9991007. |
| [453] | Foley RN, Gilbertson DT, Murray T, Collins AJ. (2011). Long interdialytic interval and mortality among patients receiving hemodialysis. N Engl J Med., 365:1099107. |
| [454] | Moss AH, Holley JL, Upton MB. (1992). Outcomes of cardiopulmonary resuscitation in dialysis patients. JAm Soc Nephrol., 3:123843. |
| [455] | Wong SP, Kreuter W, Curtis JR, Hall YN, O’Hare AM. (2015). Trends in inhospital cardiopulmonary resuscitation and survival in adults receiving maintenance dialysis. JAMA Intern Med., 175:102835. |
| [456] | Saeed F, Adil MM, Malik AA, Schold JD, Holley JL. (2015). Outcomes of inhospital cardiopulmonary resuscitation in maintenance dialysis patients. J Am Soc Nephrol., 26:3093101. |
| [457] | Jadoul M, Thumma J, Fuller DS, et al. (2012). Modifiable practices associated with sudden death among hemodialysis patients in the dialysis outcomes and practice patterns study. Clin J Am Soc Nephrol., 7:76574. |
| [458] | Lehrich RW, Pun PH, Tanenbaum ND, Smith SR, Middleton JP. (2007). Automated external defibrillators and survival from cardiac arrest in the outpatient hemodialysis clinic. J Am Soc Nephrol., 18:31220. |
| [459] | Muller MP, Hansel M, Stehr SN, Weber S, Koch T. (2008). A state-wide survey of medical emergency management in dental practices: incidence of emergencies and training experience. Emerg Med., 25:296300. |
| [460] | Arsati F, Montalli VA, Florio FM, et al. (2010). Brazilian dentists’ attitudes about medical emergencies during dental treatment. J Dent Educ., 74:6616. |
| [461] | Girdler NM, Smith DG. (1999). Prevalence of emergency events in British dental practice and emergency management skills of British dentists. Resuscitation, 41:15967. |
| [462] | Jeffcoach DR, Gallegos JJ, Jesty SA, et al. (2016). Use of CPR in hemorrhagic shock, a dog model. J Trauma Acute Care Surg., 81:2733. |
| [463] | Chapman Pj, Penkeyman Hw. (2002). Successful defibrillation of a dental patient in cardiac arrest. Aust Dent J., 47:1767. |
| [464] | Absi EG. (1987). A cardiac arrest in the dental chair. Br Dent J., 163: 199200. |
| [465] | Yokoyama T, Yoshida K, Suwa K. (2008). Efficacy of external cardiac compression in a dental chair. Resuscitation, 79:1756. |
| [466] | Fujino H, Yokoyama T, Yoshida K, Suwa K. (2010). Using a stool for stabilization of a dental chair when CPR is required. Resuscitation, 81:502. |
| [467] | Laurent F, Segal N, Augustin P. (2010). Chest compression: not as effective on dental chair as on the floor. Resuscitation, 81:1729 author reply 30. |
| [468] | Lepere AJ, Finn J, Jacobs I. (2003). Efficacy of cardiopulmonary resuscitation performed in a dental chair. Aust Dent J., 48: 2447. |
| [469] | Awata N, Hitosugi T, Miki Y, et al. (2019). Usefulness of a stool to stabilize dental chairs for cardiopulmonary resuscitation (CPR). BMC Emerg Med., 19:46. |
| [470] | Meechan JG, Skelly AM. (1997). Problems complicating dental treatment with local anaesthesia or sedation: prevention and management. Dent Update, 24:27883. |
| [471] | Jowett NI, Cabot LB. (2000). Patients with cardiac disease: considerations for the dental practitioner. Br Dent J., 189:297302. |
| [472] | Handley AJ, Handley JA. (2004). Performing chest compressions in a confined space. Resuscitation, 61:5561. |
| [473] | Watts S, Smith JE, Gwyther R, Kirkman E. (2019). Closed chest compressions reduce survival in an animal model of haemorrhageinduced traumatic cardiac arrest. Resuscitation, 140: 3742. |
| [474] | Perkins GD, Stephenson BT, Smith CM, Gao F. (2004). A comparison between over-the-head and standard cardiopulmonary resuscitation. Resuscitation, 61:15561. |
| [475] | Rosenberg M. (2010). Preparing for medical emergencies: the essential drugs and equipment for the dental office. J Am Dent Assoc., 141:14S9S. |
| [476] | Laurent F, Augustin P, Zak C, Maman L, Segal N. (2011). Preparedness of dental practices to treat cardiac arrest: availability of defibrillators. Resuscitation, 82:14689. |
| [477] | Kandray DP, Pieren JA, Benner RW. (2007). Attitudes of Ohio dentists and dental hygienists on the use of automated external defibrillators. J Dent Educ., 71:4806. |
| [478] | Breuer G, Knipfer C, Huber T, et al. (2016). Competency in managing cardiac arrest: a scenario-based evaluation of dental students. Acta Odontol Scand, 74:2419. |
| [479] | Chapman PJ. (1995). A questionnaire survey of dentists regarding knowledge and perceived competence in resuscitation and occurrence of resuscitation emergencies. Aust Dent J., 40: 98103. |
| [480] | Atherton GJ, Pemberton MN, Thornhill MH. (2000). Medical emergencies: the experience of staff of a UK dental teaching hospital. Br Dent J., 188:3204. |
| [481] | Graf J, Stuben U, Pump S. (2012). In-flight medical emergencies. Dtsch Arztebl Int., 109:591601 quiz 2. |
| [482] | Hinkelbein J. (2015). Significant more research required: no further progress without sound medical data and valid denominators for in-flight medical emergencies. J Travel Med., 22:3556. |
| [483] | Hinkelbein J, Neuhaus C, Wetsch WA, et al. (2014). Emergency medical equipment on boardGerman airliners. JTravel Med., 21:31823. |
| [484] | Endo A, Kojima M, Hong ZJ, Otomo Y, Coimbra R. (2020). Open-chest versus closed-chest cardiopulmonary resuscitation in trauma patients with signs of life upon hospital arrival: a retrospective multicenter study. Crit Care, 24:541. |
| [485] | Peterson DC, Martin-Gill C, Guyette FX, et al. (2013). Outcomes of medical emergencies on commercial airline flights. N Engl J Med., 368:207583. |
| [486] | Hinkelbein J, Neuhaus C. (2019). In-flight cardiac arrest and in-flight cardiopulmonary resuscitation during commercial air travel: consensus statement and supplementary treatment guideline from the German society of aerospace medicine (DGLRM): reply. Intern Emerg Med., 14:62930. |
| [487] | Charles RA. (2011). Cardiac arrest in the skies. Singapore Med J., 52:5825. |
| [488] | Hinkelbein J, Bohm L, Braunecker S, et al. (2018). In-flight cardiac arrest and in-flight cardiopulmonary resuscitation during commercial air travel: consensus statement and supplementary treatment guideline from the German Society of Aerospace Medicine (DGLRM). Intern Emerg Med., 13:130522. |
| [489] | Mahony, PH, Griffiths RF, Larsen, P, Powell D. (2008). Retention of knowledge and skills in first aid and resuscitation by airline cabin crew. Resuscitation, 76:4138. |
| [490] | Brown AM, Rittenberger JC, Ammon CM, Harrington S, Guyette FX. (2010). In-flight automated external defibrillator use and consultation patterns. Prehosp Emerg Care, 14: 2359. |
| [491] | Skogvoll E, Bjelland E, Thorarinsson B. (2000). Helicopter emergency medical service in out-of-hospital cardiac arrest — a 10-year population-based study. Acta Anaesthesiol Scand., 44:9729. |
| [492] | Lyon RM, Nelson MJ. (2013). Helicopter emergency medical services (HEMS) response to out-of-hospital cardiac arrest. Scand J Trauma Resusc Emerg Med., 21:1. |
| [493] | Hinkelbein J, Schmitz J, Glaser E. (2019). Pressure but not the fraction of oxygen is altered in the aircraft cabin. Anaesth Intensive Care, 47:209. |
| [494] | Verjee MA, Crone R, Ostrovskiy G. (2018). Medical issues in flight and updating the emergency medical kit. Open Access Emerg Med., 10:4751. |
| [495] | Brown DJ, Brugger H, Boyd J, Paal P. (2012). Accidental hypothermia. N Engl J Med., 367:19308. |
| [496] | Sperry JL, Guyette FX, Brown JB, et al. (2018). Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock. N Engl J Med., 379:31526. |
| [497] | Rauch S, Strapazzon G, Brodmann M, et al. (2018). Implementation of a mechanical CPR device in a physician staffed HEMS—a prospective observational study. Scand J Trauma Resusc Emerg Med., 26:36. |
| [498] | McIntosh SE, Swanson ER, McKeone A, Barton ED. (2008). Location of airway management in air medical transport. Prehosp Emerg Care, 12:43842. |
| [499] | Das A, Majumdar S, Mukherjee A, et al. (2014). i-gel in ambulatory surgery: a comparison with LMA-ProSeal in paralyzed anaesthetized patients. J Clin Diagn Res., 8:804. |
| [500] | Ley SJ. (2015). Standards for resuscitation after cardiac surgery. Crit Care Nurse, 35:307 quiz 8. |
| [501] | Paal P, Ellerton J, Sumann G, et al. (2007). Basic life support ventilation in mountain rescue. Official recommendations of the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). High Alt Med Biol., 8:14754. |
| [502] | Elsensohn F, Soteras I, Resiten O, et al. (2011). Equipment of medical backpacks in mountain rescue. High Alt Med Biol., 12:3437. |
| [503] | Doan TN, Schultz BV, Rashford S, Bosley E. (2020). Surviving out-ofhospital cardiac arrest: the important role of bystander interventions. Australas Emerg Care, 23:4754. |
| [504] | Carron M, Emeyriat N, Levraut J, Blondeau N. (2018). Cruise ship pathologies in remote regions. Int Marit Health, 69:7583. |
| [505] | Alves PM, Leigh R, Bartos G, et al. (2010). Cardiovascular events on board commercial maritime vessels: a two-year review. Int Marit Health, 62:13742. |
| [506] | Marijon E, Bougouin W, Karam N, et al. (2015). Survival from sports-related sudden cardiac arrest: in sports facilities versus outside of sports facilities. Am Heart J., 170: 33945 e1. |
| [507] | Guyette FX, Sperry JL, Peitzman AB, et al. (2019). Prehospital blood product and crystalloid resuscitation in the severely injured patient: a secondary analysis of the prehospital air medical plasma trial. Ann Surg 2019. |
| [508] | Ackerman M, Atkins DL, Triedman JK. (2016). Sudden cardiac death in the young. Circulation, 133:100626. 511. Finocchiaro G, Papadakis M, Robertus JL, et al. (2016). Etiology of sudden death in sports: insights from a United Kingdom Regional Registry. J Am Coll Cardiol., 67:210815. |
| [509] | Landry CH, Allan KS, Connelly KA, et al. (2017). Sudden cardiac arrest during participation in competitive sports. N Engl J Med., 377:194353. |
| [510] | Northcote RJ, Flannigan C, Ballantyne D. (1986). Sudden death and vigorous exercise—a study of 60 deaths associated with squash. Br Heart J., 55:198203. |
| [511] | Burtscher M, Pachinger O, Mittleman MA, Ulmer H. (2000). Prior myocardial infarction is the major risk factor associated with sudden cardiac death during downhill skiing. Int J Sports Med., 21:6135. |
| [512] | Kim JH, Malhotra R, Chiampas G, et al. (2012). Cardiac arrest during long distance running races. N Engl J Med., 366:13040. |
| [513] | Harris KM, Creswell LL, Haas TS, et al. (2017). Death and cardiac arrest in U. S. triathlon participants, 1985 to 2016: a case series. Ann Intern Med., 167:52935. |
| [514] | Link MS, Estes 3rd NA. (2012). Sudden cardiac death in the athlete: bridging the gaps between evidence, policy, and practice. Circulation, 125:25116. |
| [515] | Franklin BA, Thompson PD, Al-Zaiti SS, et al. (2020). Exercise-related acute cardiovascular events and potential deleterious adaptations following long-term exercise training: placing the risks into perspective-an update: a scientific statement from the American Heart Association. Circulation, 141: e705e36. |
| [516] | Albert CM, Mittleman MA, Chae CU, et al. (2000). Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med., 343:135561. |
| [517] | Singletary EM, Zideman DA, Bendall JC, et al. (2020). International Consensus on First Aid Science with Treatment Recommendations. Resuscitation, 156: A240A82. |
| [518] | Marijon E, Bougouin W, Jouven X. (2015). Sports-related sudden death: lessons from the French registry. Rev Prat., 65:91923. |
| [519] | Kiyohara K, Nishiyama C, Kiguchi T, et al. (2017). Exercise-related out-of-hospital cardiac arrest among the general population in the era of public-access defibrillation: a population-based observation in Japan. J Am Heart Assoc 6. |
| [520] | Berdowski J, de Beus MF, Blom M, et al. (2013). Exercise-related out-ofhospital cardiac arrest in the general population: incidence and prognosis. Eur Heart J., 34:361623. |
| [521] | Drezner JA, Toresdahl, BG, Rao, AL, Huszti, E, Harmon, KG.(2013). Outcomes from sudden cardiac arrest in US high schools: a 2-year prospective study from the National Registry for AED use in sports. Br J Sports Med., 47:117983. |
| [522] | Mont L, Pelliccia A, Sharma S, et al. (2017). Pre-participation cardiovascular evaluation for athletic participants to prevent sudden death: position paper from the EHRA and the EACPR, branches of the ESC. Endorsed by APHRS, HRS, and SOLAECE. Eur J Prev Cardiol., 24:4169. |
| [523] | Maron BJ, Friedman RA, Kligfield P, et al. (2014). Assessment of the 12-lead ECG as a screening test for detection of cardiovascular disease in healthy general populations of young people (12-25 years of age): a scientific statement from the American Heart Association and the American College of Cardiology. Circulation, 130: 130334. |
| [524] | Wilson MG, Chatard JC, Carre F, et al. Prevalence of electrocardiographic abnormalities in West-Asian and African male Athletes. Br J Sports Med., 46:341–7. |
| [525] | Sharma S. (2016). IOC manual of sports cardiology. London: Wiley; 2016. |
| [526] | Armstrong M, Paternostro-Bayles M, Conroy MB, et al. (2018). Preparticipation screening prior to physical activity in community lifestyle interventions. Transl J Am Coll Sports Med., 3:17680. |
| [527] | Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. (2009). Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 19802006. Circulation, 119:108592. |
| [528] | Yue JK, Tsolinas RE, Burke JF, et al. (2019). Vasopressor support in managing acute spinal cord injury: current knowledge. J Neurosurg Sci., 63:30817. |
| [529] | Maron BJ, Gohman TE, Kyle SB, Estes 3rd NA, Link MS. (2002). Clinical profile and spectrum of commotio cordis. JAMA, 287:11426. |
| [530] | Maron BJ, Haas TS, Ahluwalia A, et al. (2013). Increasing survival rate from commotio cordis. Heart Rhythm, 10:21923. |
| [531] | Seguin C, Blaquiere G, Loundou A, Michelet P, Markarian T. (2018). Unmanned aerial vehicles (drones) to prevent drowning. Resuscitation, 127:637. |
| [532] | Claesson A, Svensson L, Nordberg P, et al. (2017). Drones may be used to save lives in out of hospital cardiac arrest due to drowning. Resuscitation, 114:1526. |
| [533] | Claesson A, Schierbeck S, Hollenberg J, et al. (2020). The use of drones and a machine-learning model for recognition of simulated drowning victims—a feasibility study. Resuscitation, 156:196201. |
| [534] | Griffiths MJD, McAuley DF, Perkins GD, et al. (2019). Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir Res., 6: e000420. |
| [535] | El Sayed M, Tamim H, Mann NC. (2015). Description of procedures performed on patients by emergency medical services during mass casualty incidents in the United States. Am J Emerg Med., 33:10306. |
| [536] | Schenk E, Wijetunge G, Mann NC, et al. (2014). Epidemiology of mass casualty incidents in the United States. Prehosp Emerg Care, 18:40816. |
| [537] | Turner CD, Lockey DJ, Rehn M. (2016). Pre-hospital management of mass casualty civilian shootings: a systematic literature review. Crit Care, 20:362. |
| [538] | Jain T, Sibley, A, Stryhn, H, Hubloue, I. (2018). Comparison of unmanned aerial vehicle technology-assisted triage versus standard practice in triaging casualties by paramedic students in a mass-casualty incident scenario. Prehosp Disaster Med., 33:37580. |
| [539] | Atkinson JL. (2000). The neglected prehospital phase of head injury: apnea and catecholamine surge. Mayo Clin Proc., 75:3747. |
| [540] | Nolan JP, Monsieurs KG, Bossaert, L, et al. (2020). European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation, 153:4555. |
| [541] | Castle N, Pillay Y, Spencer N. (2011). Comparison of six different intubation aids for use while wearing CBRN-PPE: a manikin study. Resuscitation, 82:154852. |
| [542] | Lamhaut L, Dagron C, Apriotesei R, et al. (2010). Comparison of intravenous and intraosseous access by pre-hospital medical emergency personnel with and without CBRN protective equipment. Resuscitation, 81:658. |
| [543] | Castle N, Bowen J, Spencer N. (2010). Does wearing CBRN-PPE adversely affect the ability for clinicians to accurately, safely, and speedily draw up drugs? Clin Toxicol (Phila), 48:5227. |
| [544] | Tokuda Y, Kikuchi M, Takahashi O, Stein GH. (2006). Prehospital management of sarin nerve gas terrorism in urban settings: 10 years of progress after the Tokyo subway sarin attack. Resuscitation, 68:193202. |
| [545] | Cross KP, Petry MJ, Cicero MX. (2015). A better START for low-acuity victims: data-driven refinement of mass casualty triage. Prehosp Emerg Care, 19:2728. |
| [546] | ACEP. (2008). SALT mass casualty triage: concept endorsed by the American College of Emergency Physicians, American College of Surgeons Committee on Trauma, American Trauma Society, National Association of EMS Physicians, National Disaster Life Support Education Consortium, and State and Territorial Injury Prevention Directors Association. Disaster Med Public Health Prep., 2:2456. |
| [547] | Cone DC, Serra J, Burns K, et al. (2009). Pilot test of the SALT mass casualty triage system. Prehosp Emerg Care, 13:53640. |
| [548] | Streckbein S, Kohlmann T, Luxen J, Birkholz T, Pruckner S. (2016). Triage protocols for mass casualty incidents: an overview 30 years after START. Unfallchirurg, 119:62031. |
| [549] | Jones N, White ML, Tofil N, et al. (2014). Randomized trial comparing two mass casualty triage systems (JumpSTART versus SALT) in a pediatric simulated mass casualty event. Prehosp Emerg Care, 18:41723. |
| [550] | Wilson MH, Hinds J, Grier G, et al. (2016). Impact brain apnoea—a forgotten cause of cardiovascular collapse in trauma. Resuscitation, 105:528. |
| [551] | Broach J, Hart A, Griswold M, et al. (2018). Usability and reliability of smart glasses for secondary triage during mass casualty incidents. Proc Annu Hawaii Int Conf Syst Sci., 2018:141622. |
| [552] | Risavi BL, Terrell MA, Lee W, Holsten Jr DL. (2013). Prehospital mass casualty triage training-written versus moulage scenarios: how much do EMS providers retain? Prehosp Disaster Med., 28:2516. |
| [553] | Knight JF, Carley S, Tregunna B, et al. (2010). Serious gaming technology in major incident triage training: a pragmatic controlled trial. Resuscitation, 81:11759. |
| [554] | Franklin C, Samuel J, Hu T-C. (1994). Life-threatening hypotension associated with emergency intubation and the initiation of mechanical ventilation. Am J Emerg Med., 12:4258. |
| [555] | Lemaitre RN, Siscovick DS, Psaty BM, et al. (2002). Inhaled beta-2 adrenergic receptor agonists and primary cardiac arrest. Am J Med., 113:7116. |
| [556] | Boucher A, Payen C, Garayt C, et al. (2011). Salbutamol misuse or abuse with fatal outcome: a case-report. Hum Exp Toxicol., 30:186971. |
| [557] | van den Berg ME, Stricker BH, Brusselle GG, Lahousse L. (2016). Chronic obstructive pulmonary disease and sudden cardiac death: a systematic review. Trends Cardiovasc Med., 26:60613. |
| [558] | Salpeter SR, Ormiston TM, Salpeter EE. (2004). Cardiovascular effects of beta-agonists in patients with asthma and COPD: a meta-analysis. Chest, 125:230921. |
| [559] | Rosero SZ, Zareba W, Moss AJ, et al. (1999). Asthma and the risk of cardiac events in the Long QT syndrome. Long QT Syndrome Investigative Group. Am J Cardiol., 84:140611. |
| [560] | Granfeldt A, Wissenberg M, Hansen SM, et al. (2018). Severity of chronic obstructive pulmonary disease and presenting rhythm in patients with out-of-hospital cardiac arrest. Resuscitation, 126:1117. |
| [561] | Hudson AJ, Strandenes G, Bjerkvig CK, Svanevik M, Glassberg E. (2018). Airway and ventilation management strategies for hemorrhagic shock. To tube, or not to tube, that is the question!. J Trauma Acute Care Surg., 84: S7782. |
| [562] | Herlitz J, Rosenfelt M, Bang A, et al. (1996). Prognosis among patients with out-of-hospital cardiac arrest judged as being caused by deterioration of obstructive pulmonary disease. Resuscitation, 32:17784. |
| [563] | Leatherman JW, McArthur C, Shapiro RS. (2004). Effect of prolongation of expiratory time on dynamic hyperinflation in mechanically ventilated patients with severe asthma. Crit Care Med., 32: 15425. |
| [564] | Hostetler MA, Davis CO. (1999). Bilateral localized tension pneumothoraces refractory to needle decompression. Pediatr Emerg Care, 15:3224. |
| [565] | Williams-Johnson J, Williams EW, Hart N, et al. (2008). Simultaneous spontaneous bilateral pneumothoraces in an asthmatic. West Indian Med J., 57:50810. |
| [566] | Komasawa N, Ueki R, Kusuyama K, et al. (2010). Case of tension pneumothorax associated with asthma attack during general anesthesia. Masui., 59:6147. |
| [567] | Robert J, Derkenne C, Jost D, Tourtier JP. (2017). Out-of-hospital cardiac arrest: an underlying reversible cause. Circulation, 135:25646. |
| [568] | Burdett-Smith P, Jaffey L. (1996). Tension pneumoperitoneum. J Accid Emerg Med., 13:2201. |
| [569] | Castle N, Tagg A, Owen R. (2005). Bilateral tension pneumothorax. Resuscitation, 65:1035. |
| [570] | Martens P, Vandekerckhove Y, Mullie A. (1993). Restoration of spontaneous circulation after cessation of cardiopulmonary resuscitation. Lancet, 341:841. |
| [571] | Lapinsky SE, Leung RS. (1996). Auto-PEEP and electromechanical dissociation. N Engl J Med., 335:674. |
| [572] | El-Sayed AA, Arafa SK, El-Demerdash AM. (2019). Pressure-controlled ventilation could decrease intraoperative blood loss and improve airway pressure measures during lumbar discectomy in the prone position: a comparison with volume-controlled ventilation mode. J Anaesthesiol Clin Pharmacol., 35:46874. |
| [573] | Rogers PL, Schlichtig R, Miro A, Pinsky M. (1991). Auto-PEEP during CPR. An "occult" cause of electromechanical dissociation? Chest, 99:4923. |
| [574] | Rosengarten Pl, Tuxen Dv, Dziukas L, et al. (1991). Circulatory arrest induced by intermittent positive pressure ventilation in a patient with severe asthma. Anaesth Intensive Care., 19:11821. |
| [575] | Sprung J, Hunter K, Barnas GM, Bourke DL. (1994). Abdominal distention is not always a sign of esophageal intubation: cardiac arrest due to "auto-PEEP". Anesth Analg., 78:8014. |
| [576] | Harrison R. (2010). Chest compression first aid for respiratory arrest due to acute asphyxic asthma. Emerg Med., 27:5961. |
| [577] | Fisher MM, Whaley AP, Pye RR. (2001). External chest compression in the management of acute severe asthma—a technique in search of evidence. Prehosp Disaster Med., 16:1247. |
| [578] | Eason J, Tayler D, Cottam S, et al. (1991). Manual chest compression for total bronchospasm. Lancet, 337: 366. |
| [579] | Fisher MM, Bowey CJ, Ladd-Hudson K. (1989). External chest compression in acute asthma: a preliminary study. Crit Care Med., 17:6867. |
| [580] | Myles PS, Weeks AM. (1993). Cardiopulmonary resuscitation in obstructive airways disease. Lancet, 341: 1217. |
| [581] | Perkins GD, Ji C, Deakin CD, et al. (2018). A randomized trial of epinephrine in out-of-hospital cardiac arrest. N Engl J Med., 379:71121. |
| [582] | Smith D, Riel J, Tilles I, et al. (2003). Intravenous epinephrine in lifethreatening asthma. Ann Emerg Med., 41:70611. |
| [583] | Pepe PE, Roppolo LP, Fowler RL. (2005). The detrimental effects of ventilation during low-blood-flow states. Curr Opin Crit Care, 11:2128. |
| [584] | Putland M, Kerr D, Kelly AM. (2006). Adverse events associated with the use of intravenous epinephrine in emergency department patients presenting with severe asthma. Ann Emerg Med., 47: 55963. |
| [585] | Yeo HJ, Kim D, Jeon D, et al. (2017). Extracorporeal membrane oxygenation for life-threatening asthma refractory to mechanical ventilation: analysis of the Extracorporeal Life Support Organization registry. Crit Care, 21:297. |
| [586] | Mikkelsen ME, Woo YJ, Sager JS, Fuchs BD, Christie JD. (2009). Outcomes using extracorporeal life support for adult respiratory failure due to status asthmaticus. ASAIO J., 55:4752. |
| [587] | Hubner P, Meron G, Kurkciyan I, et al. (2014). Neurologic causes of cardiac arrest and outcomes. J Emerg Med., 47:6607. |
| [588] | Kim AS, Moffatt E, Ursell PC, et al. (2016). Sudden neurologic death masquerading as out-of-hospital sudden cardiac death. Neurology, 87:166973. |
| [589] | Sandroni C, Dell’Anna AM. (2015). Out-of-hospital cardiac arrest from neurologic cause: recognition and outcome. Crit Care Med., 43:5089. |
| [590] | Arnaout M, Mongardon N, Deye N, et al. (2015). Out-of-hospital cardiac arrest from brain cause: epidemiology, clinical features, and outcome in a multicenter cohort. Crit Care Med., 43:45360. |
| [591] | Petek BJ, Erley CL, Kudenchuk PJ, et al. (2019). Diagnostic yield of noninvasive imaging in patients following non-traumatic out-of-hospital sudden cardiac arrest: a systematic review. Resuscitation, 135:18390. |
| [592] | Skrifvars MB, Parr MJ. (2012). Incidence, predisposing factors, management and survival following cardiac arrest due to subarachnoid haemorrhage: a review of the literature. Scand J Trauma Resusc Emerg Med., 20:75. |
| [593] | Inamasu J, Miyatake S, Tomioka H, et al. (2009). Subarachnoid haemorrhage as a cause of out-of-hospital cardiac arrest: a prospective computed tomography study. Resuscitation, 80:97780. |
| [594] | Deakin CD, Davies G, Wilson A. (1995). Simple thoracostomy avoids chest drain insertion in prehospital trauma. J Trauma, 39: 3734. |
| [595] | Shin J, Kim K, Lim YS, et al. (2016). Incidence and clinical features of intracranial hemorrhage causing out-of-hospital cardiac arrest: a multicenter retrospective study. Am J Emerg Med., 34: 232630. |
| [596] | Legriel S, Bougouin W, Chocron R, et al. (2018). Early in-hospital management of cardiac arrest from neurological cause: diagnostic pitfalls and treatment issues. Resuscitation, 132:14755. |
| [597] | Mitsuma W, Ito M, Kodama M, et al. (2011). Clinical and cardiac features of patients with subarachnoid haemorrhage presenting with out-ofhospital cardiac arrest. Resuscitation, 82:12947. |
| [598] | Park I, Kim YJ, Ahn S, et al. (2015). Subarachnoid hemorrhage mimicking ST-segment elevation myocardial infarction after return of spontaneous circulation. Clin Exp Emerg Med., 2:2603. |
| [599] | Zachariah J, Stanich JA, Braksick SA, et al. (2017). Indicators of subarachnoid hemorrhage as a cause of sudden cardiac arrest. Clin Pract Cases Emerg Med., 1:1325. |
| [600] | Noritomi DT, de Cleva R, Beer I, et al. (2006). Doctors awareness of spontaneous subarachnoid haemorrhage as a cause of cardiopulmonary arrest. Resuscitation, 71:1234. |
| [601] | Morris NA, Robinson D, Schmidt JM, et al. (2018). Hunt-Hess 5 subarachnoid haemorrhage presenting with cardiac arrest is associated with larger volume bleeds. Resuscitation, 123:716. |
| [602] | Thurman DJ, Hesdorffer DC, French JA. (2014). Sudden unexpected death in epilepsy: assessing the public health burden. Epilepsia, 55:147985. |
| [603] | Maguire MJ, Jackson CF, Marson AG, Nevitt SJ. (2020). Treatments for the prevention of Sudden Unexpected Death in Epilepsy (SUDEP). Cochrane Database Syst Rev., 4: CD011792. |
| [604] | Joundi RA, Rabinstein AA, Nikneshan D, et al. (2016). Cardiac arrest in acute ischemic stroke: incidence, predisposing factors, and clinical outcomes. J Stroke Cerebrovasc Dis., 25:164452. |
| [605] | Paal P, Gordon L, Strapazzon G, et al. (2016). Accidental hypothermia-an update: the content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). Scand J Trauma Resusc Emerg Med., 24:111. |
| [606] | Escott ME, Gleisberg GR, Kimmel K, et al. (2014). Simple thoracostomy. Moving beyong needle decompression in traumatic cardiac arrest. JEMS, 39:2632. |
| [607] | Fukuda T, Ohashi-Fukuda N, Kondo Y, et al. (2016). Epidemiology, risk factors, and outcomes of out-of-hospital cardiac arrest caused by stroke: a population-based study. Medicine (Baltimore), 95: e3107. |
| [608] | Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. (2016). Trends in obesity among adults in the United States, 2005 to 2014. JAMA, 315:228491. |
| [609] | Koliaki C, Liatis S, Kokkinos A. (2019). Obesity and cardiovascular disease: revisiting an old relationship. Metabolism., 92:98107. |
| [610] | Romero-Corral A, Montori VM, Somers VK, et al. (2006). Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet, 368:66678. |
| [611] | Adabag S, Huxley RR, Lopez FL, et al. (2015). Obesity related risk of sudden cardiac death in the atherosclerosis risk in communities’ study. Heart, 101:21521. |
| [612] | Kakavas S, Georgiopoulos G, Oikonomou D, et al. (2018). The impact of body mass index on post resuscitation survival after cardiac arrest: a meta-analysis. Clin Nutr ESPEN, 24:4753. |
| [613] | Ma Y, Huang L, Zhang L, Yu H, Liu B. (2018). Association between body mass index and clinical outcomes of patients after cardiac arrest and resuscitation: a meta-analysis. Am J Emerg Med., 36:12709. |
| [614] | Lee H, Oh J, Lee J, et al. (2019). Retrospective study using computed tomography to compare sufficient chest compression depth for cardiopulmonary resuscitation in obese patients. J Am Heart Assoc., 8:e013948. |
| [615] | Jain R, Nallamothu BK, Chan PS. (2010). American Heart Association National Registry of Cardiopulmonary Resuscitation i. Body mass index and survival after in-hospital cardiac arrest. Circ Cardiovasc Qual Outcomes, 3:4907. |
| [616] | Nishisaki A, Maltese MR, Niles DE, et al. (2012). Backboards are important when chest compressions are provided on a soft mattress. Resuscitation, 83:101320. |
| [617] | Clemency BM, Tanski CT, Rosenberg M, et al. (2015). Sufficient catheter length for pneumothorax needle decompression: a meta-analysis. Prehosp Disaster Med., 30:24953. |
| [618] | Holt J, Ward A, Mohamed TY, et al. (2020). The optimal surface for delivery of CPR: a systematic review and meta-analysis. Resuscitation, 155:15964. |
| [619] | Bunch TJ, White RD, Lopez-Jimenez F, Thomas RJ. (2008). Association of body weight with total mortality and with ICD shocks among survivors of ventricular fibrillation in out-of-hospital cardiac arrest. Resuscitation, 77:3515. |
| [620] | White RD, Blackwell TH, Russell JK, Jorgenson DB. (2004). Body weight does not affect defibrillation, resuscitation, or survival in patients with out-of-hospital cardiac arrest treated with a nonescalating biphasic waveform defibrillator. Crit Care Med., 32:S38792. |
| [621] | Voskoboinik A, Moskovitch J, Plunkett G, et al. (2019). Cardioversion of atrial fibrillation in obese patients: results from the cardioversion-BMI randomized controlled trial. J Cardiovasc Electrophysiol., 30:15561. |
| [622] | Sugerman H, Windsor A, Bessos M, Wolfe L.(1997). Intra-abdominal pressure, sagittal abdominal diameter and obesity comorbidity. J Intern Med., 241:719. |
| [623] | Schnittker R, Marshall Sd, Berecki-Gisolf J. (2020). Patient and surgery factors associated with the incidence of failed and difficult intubation. Anaesthesia, 75:75666. |
| [624] | Holmberg TJ, Bowman SM, Warner KJ, et al. (2011). The association between obesity and difficult prehospital tracheal intubation. Anesth Analg., 112:11328. |
| [625] | Cook TM, Woodall N, Frerk C. (2011). Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth., 106:61731. |
| [626] | Timmermann A, Nickel EA, Puhringer F. (2015). Second generation laryngeal masks: expanded indications. Anaesthesist., 64: 715. |
| [627] | Zoremba M, Aust H, Eberhart L, Braunecker S, Wulf H. (2009). Comparison between intubation and the laryngeal mask airway in moderately obese adults. Acta Anaesthesiol Scand., 53:43642. |
| [628] | Hecker M, Hegenscheid K, Volzke H, et al. (2016). Needle decompression of tension pneumothorax: population-based epidemiologic approach to adequate needle length in healthy volunteers in Northeast Germany. J Trauma Acute Care Surg., 80:11924. |
| [629] | Reminiac F, Jouan Y, Cazals X, et al. (2014). Risks associated with obese patient handling in emergency prehospital care. Prehosp Emerg Care, 18:5557. |
| [630] | Kruska P, Kappus S, Kerner T. (2012). Obesity in prehospital emergency care. Anasthesiol Intensivmed Notfallmed Schmerzther., 47: 55662. |
| [631] | Beckett VA, Knight M, Sharpe P. (2017). The CAPS study: incidence, management and outcomes of cardiac arrest in pregnancy in the UK: a prospective, descriptive study. BJOG., 124: 13741381. |
| [632] | Jeejeebhoy FM, Zelop CM, Lipman S, et al. (2015). Cardiac arrest in pregnancy: a scientific statement from the American Heart Association. Circulation, 132:174773. |
| [633] | Chu J, Johnston TA, Geoghegan J, Royal College of O, Gynaecologists. (2020). Maternal collapse in pregnancy and the puerperium: green-top guideline no. 56. BJOG., 127: e1452. |
| [634] | Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. (2018). 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J., 39:3165241. |
| [635] | UK M-UMaBRRtAaCEat. (2019). MBRRACE-UK perinatal mortality surveillance report. UK perinatal deaths for births from January to December 2017. London: MBRRACE-UK; 2019. |
| [636] | Chesnutt AN. (2004). Physiology of normal pregnancy. Crit Care Clin., 20:60915. |
| [637] | Page-Rodriguez A, Gonzalez-Sanchez JA. (1999). Perimortem cesarean section of twin pregnancy: case report and review of the literature. Acad Emerg Med., 6:10724. |
| [638] | Cardosi RJ, Porter KB. (1998). Cesarean delivery of twins during maternal cardiopulmonary arrest. Obstet Gynecol., 92:6957. |
| [639] | Flaris AN, Simms ER, Prat N, et al. (2015). Clamshell incision versus left anterolateral thoracotomy. Which one is faster when performing a resuscitative thoracotomy? The tortoise and the hare revisited. World J Surg., 39:130611. |
| [640] | Humphries A, Mirjalili SA, Tarr GP, Thompson JMD, Stone P. (2019). The effect of supine positioning on maternal hemodynamics during late pregnancy. J Matern Fetal Neonatal Med., 32:392330. |
| [641] | Kundra P, Khanna S, Habeebullah S, Ravishankar M. (2007). Manual displacement of the uterus during caesarean section. Anaesthesia, 62:4605. |
| [642] | Mendonca C, Griffiths J, Ateleanu B, Collis RE. (2003). Hypotension following combined spinal-epidural anaesthesia for caesarean section. Left lateral position vs. tilted supine position. Anaesthesia, 58:42831. |
| [643] | Rees SG, Thurlow JA, Gardner IC, Scrutton MJ, Kinsella SM. (2002). Maternal cardiovascular consequences of positioning after spinal anaesthesia for caesarean section: left 15 degree table tilt vs. left lateral. Anaesthesia, 57:1520. |
| [644] | Bamber JH, Dresner M. (2003). Aortocaval compression in pregnancy: the effect of changing the degree and direction of lateral tilt on maternal cardiac output. Anesth Analg., 97:2568 table of contents. |
| [645] | Kinsella SM. (2003). Lateral tilt for pregnant women: why 15 degrees? Anaesthesia, 58:8356. |
| [646] | Rees GA, Willis BA. (1988). Resuscitation in late pregnancy. Anaesthesia, 43:3479. |
| [647] | Holmes S, Kirkpatrick ID, Zelop CM, Jassal DS. (2015). MRI evaluation of maternal cardiac displacement in pregnancy: implications for cardiopulmonary resuscitation. Am J Obstet Gynecol., 213: 401 e15. |
| [648] | Delgado C, Dawson K, Schwaegler B, et al. (2020). Hand placement during chest compressions in parturients: a pilot study to identify the location of the left ventricle using transthoracic echocardiography. Int Jf Obstet Anesth., 43:315. |
| [649] | Einav S, Kaufman N, Sela HY. (2012). Maternal cardiac arrest and perimortem caesarean delivery: evidence or expert-based? Resuscitation, 83:1191200. |
| [650] | Wise D, Davies G, Coats T, et al. (2005). Emergency thoracotomy:"how to do it". Emerg Med., 22:224. |
| [651] | Benson MD, Padovano A, Bourjeily G, Zhou Y. (2016). Maternal collapse: challenging the four-minute rule. EBioMedicine, 6:2537. |
| [652] | Ramanathan K, Tan CS, Rycus P, et al. (2020). Extracorporeal membrane oxygenation in pregnancy: an analysis of the Extracorporeal Life Support Organization Registry. Crit Care Med., 48: 696703. |
| [653] | Nanson J, Elcock D, Williams M, Deakin CD. (2001). Do physiological changes in pregnancy change defibrillation energy requirements? Br J Anaesth., 87:2379. |
| [654] | Mushambi MC, Athanassoglou V, Kinsella SM. (2020). Anticipated difficult airway during obstetric general anaesthesia: narrative literature review and management recommendations. Anaesthesia, 75:94561. |
| [655] | Mushambi MC, Kinsella SM. (2015). Obstetric Anaesthetists’ Association/ Difficult Airway Society difficult and failed tracheal intubation guidelines—the way forward for the obstetric airway. Br J Anaesth., 115:8158. |
| [656] | Kinsella SM, Winton AL, Mushambi MC, et al. (2015). Failed tracheal intubation during obstetric general anaesthesia: a literature review. Int J Obstet Anesth., 24:35674. |
| [657] | Say L, Chou D, Gemmill A, et al. (2014). Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health, 2:e32333. |
| [658] | Lewis G. (2007). The Confidential Enquiry into Maternal and Child Health (CEMACH). Saving mothers’ lives: Reviewing maternal deaths to make motherhood safer 20032005. The seventh report of the confidential enquiries into maternal deaths in the United Kingdom. London: CEMACH; 2007. |
| [659] | Jauniaux E, Alfirevic Z, Bhide AG, et al. (2019). Vasa praevia: diagnosis and management: green-top guideline no. 27b. BJOG., 126: e4961. |
| [660] | Gynaecologists RCoOa. (2016). Postpartum Haemorrhage, Prevention and Management (Green-top Guideline No. 52). London; 2016. |
| [661] | Rhee PM, Acosta J, Bridgeman A, et al. (2000). Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg., 190: 28898. |
| [662] | Collaborators WT. (2017). Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with postpartum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet, 389:210516. |
| [663] | Ahearn GS, Hadjiliadis D, Govert JA, TapsonVF. (2002). Massive pulmonary embolism during pregnancy successfully treated with recombinant tissue plasminogen activator: a case report and review of treatment options. Arch Intern Med., 162:12217. |
| [664] | Excellence NIfHaC. (2019). Hypertension in pregnancy: diagnosis and management NICE guideline NG133. London: National Institute for Health and Care Excellence; 2019. |
| [665] | Conde-Agudelo A, Romero R. (2009). Amniotic fluid embolism: an evidencebased review. Am J Obstet Gynecol., 201: 445 e113. |
| [666] | Fitzpatrick KE, Tuffnell D, Kurinczuk JJ, Knight M. (2016). Incidence, risk factors, management and outcomes of amniotic-fluid embolism: a population-based cohort and nested case-control study. BJOG., 123:1009. |
| [667] | Rittenberger JC, Kelly E, Jang D, Greer K, Heffner A. (2008). Successful outcome utilizing hypothermia after cardiac arrest in pregnancy: a case report. Crit Care Med., 36:13546. |
| [668] | Song KH, Lee BK, Jeung KW, Lee SM. (2015). Safely completed therapeutic hypothermia in postpartum cardiac arrest survivors.Am JEmerg Med., 33: 861 e56. |
| [669] | Merien AE, van de Ven J, Mol BW, Houterman S, Oei SG. (2010). Multidisciplinary team training in a simulation setting for acute obstetric emergencies: a systematic review. Obstet Gynecol., 115:102131. |
| [670] | Leonardsen AL, Svendsen EJ, Heitmann GB, et al. (2020). Development and validation of a questionnaire to assess healthcare personnel competence in cardiac arrest and resuscitation in pregnancy. PLoS One, 15:e0232984. |
| [671] | MerrielA, Ficquet J,BarnardK, et al. (2019). The effects of interactive training of healthcare providers on the management of life-threatening emergencies in hospital. Cochrane Database Syst Rev., 9: CD012177. |
| [672] | Burlew CC, Moore EE, Moore FA, et al. (2012). Western Trauma Association critical decisions in trauma: resuscitative thoracotomy. J Trauma Acute Care Surg., 73:135963. |
| [673] | Paulich S, Lockey D. (2020). Resuscitative thoracotomy. BJA Educ., 20:2428. |
| [674] | National Institute for Clinical Excellence. (2004). Pre-hospital initiation of fluid replacement therapy for trauma. Technology appraisal guidance. London: National Institute for Clinical Excellence; 2004. |
| [675] | Harris T, Thomas GO, Brohi K. (2012). Early fluid resuscitation in severe trauma. BMJ, 345: e5752. |
| [676] | Paal P, Milani M, Brown D, Boyd J, Ellerton J. (2012). Termination of cardiopulmonary resuscitation in mountain rescue. HighAltitude Med Biol., 13:2008. |
| [677] | Jansen JO, Thomas R, Loudon MA, Brooks A. (2009). Damage control resuscitation for patients with major trauma. BMJ., 338: b1778. |
| [678] | Holcomb JB, Tilley BC, Baraniuk S, et al. (2015). Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA, 313:47182. |
| [679] | Cannon JW, Khan MA, Raja AS, et al. (2017). Damage control resuscitation in patients with severe traumatic hemorrhage: a practice management guideline from the Eastern Association for the surgery of trauma. J Trauma Acute Care Surg., 82:60517. |
| [680] | Collaborators C, Roberts I, Shakur H, et al. (2011). The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet, 377:1096101 101 e12. |
| [681] | Ferrada P, Wolfe L, Anand RJ, et al. (2014). Use of limited transthoracic echocardiography in patients with traumatic cardiac arrest decreases the rate of nontherapeutic thoracotomy and hospital costs. J Ultrasound Med., 33:182932. |
| [682] | Sampson HA, Munoz-Furlong A, Campbell RL, et al. (2006). Second symposium on the definition and management of anaphylaxis: summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol., 117:3917. |
| [683] | TurnerPJ, Campbell DE, Motosue MS, Campbell RL. (2020). Global trends in anaphylaxis epidemiology and clinical implications. J Allergy Clin Immunol Pract., 8:116976. |
| [684] | Anagnostou K, Turner PJ. (2019). Myths, facts and controversies in the diagnosis and management of anaphylaxis. Arch Dis Child., 104:8390. |
| [685] | Simons FE, Ebisawa M, Sanchez-Borges M, et al. (2015). 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. World Allergy Organ J., 8:32. |
| [686] | Shaker MS, Wallace DV, Golden DBK, et al. (2020). Anaphylaxis—a 2020 practice parameter update, systematic review, and grading of recommendations, assessment, development and evaluation (GRADE) analysis. J Allergy Clin Immunol., 145:1082123. |
| [687] | Gordon L, Paal P, Ellerton JA, et al. (2015). Delayed and intermittent CPR for severe accidental hypothermia. Resuscitation, 90:469. |
| [688] | Garvey LH, Dewachter P, Hepner DL, et al. (2019). Management of suspected immediate perioperative allergic reactions: an international overview and consensus recommendations. Br J Anaesth., 123:e5064. |
| [689] | Harper NJN, Cook TM, Garcez T, et al. (2018). Anaesthesia, surgery, and life-threatening allergic reactions: management and outcomes in the 6th National Audit Project (NAP6). Br J Anaesth., 121: 17288. |
| [690] | Ebo DG, Clarke RC, Mertes PM, et al. (2019). Molecular mechanisms and pathophysiology of perioperative hypersensitivity and anaphylaxis: a narrative review. Br J Anaesth., 123:e3849. |
| [691] | Dhami S, Panesar SS, Roberts G, et al. (2014). Management of anaphylaxis: a systematic review. Allergy, 69:16875. |
| [692] | Truhlar A, Deakin CD, Soar J, et al. (2015). European Resuscitation Council Guidelines for resuscitation 2015: section 4. Cardiac arrest in special circumstances. Resuscitation, 95:148201. |
| [693] | Visscher PK, Vetter RS, Camazine S. (1996). Removing bee stings. Lancet, 348:3012. |
| [694] | Lee JA, Singletary E, Charlton N. (2020). Methods of honey bee stinger removal: a systematic review of the literature. Cureus, 12: e8078. |
| [695] | Sheikh A, Shehata YA, Brown SG, Simons FE. (2009). Adrenaline for the treatment of anaphylaxis: cochrane systematic review. Allergy, 64:20412. |
| [696] | Singletary EM, Zideman DA, De Buck ED, et al. (2015). Part 9: first aid: 2015 International Consensus on First Aid Science with Treatment Recommendations. Circulation, 132: S269311. |
| [697] | Kelso JM. (2006). A second dose of epinephrine for anaphylaxis: how often needed and how to carry. J Allergy Clin Immunol., 117:4645. |
| [698] | Safar P, Paradis NA, Weil MH. Asphyxial cardiac arrest. In: Paradis NA, Halperin HR, Kern KB, Wenzel V, Chamberlain DA. [editors]. (2007). Cardiac arrest—the science and practice of resuscitation medicine. Cambridge: Cambride University Press, 96993. |
| [699] | Gabrielli S, Clarke A, Morris J, et al. (2019). Evaluation of prehospital management in a canadian emergency department anaphylaxis cohort. J Allergy Clin Immunol Pract., 7: 2232-8 e3. |
| [700] | Pumphrey RSH. (2003). Fatal posture in anaphylactic shock. J Allergy Clin Immunol., 112:4512. |
| [701] | Rhodes A, Evans LE, Alhazzani W, et al. (2017). Surviving sepsis campaign: International Guidelines for management of sepsis and septic shock: 2016. Intensive Care Med., 43:30477. |
| [702] | Padhi S, Bullock I, Li L, et al. (2013). Intravenous fluid therapy for adults in hospital: summary of NICE guidance. BMJ., 347: f7073. |
| [703] | Ruiz-Garcia M, Bartra J, Alvarez O, et al. (2020). Cardiovascular changes during peanut-induced allergic reactions in human subjects. J Allergy Clin Immunol., 2020. |
| [704] | O’Driscoll BR, Howard LS, Earis J, et al. (2017). BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax., 72: ii1ii90. |
| [705] | Liyanage CK, Galappatthy P, Seneviratne SL. (2017). Corticosteroids in management of anaphylaxis; a systematic review of evidence. Eur Ann Allergy Clin Immunol., 49:196207. |
| [706] | Nurmatov UB, Rhatigan E, Simons FE, Sheikh A. (2014). H2-antihistamines for the treatment of anaphylaxis with and without shock: a systematic review. Ann Allergy Asthma Immunol., 112:12631. |
| [707] | Choo KJ, Simons E, Sheikh A. (2010). Glucocorticoids for the treatment of anaphylaxis: cochrane systematic review. Allergy, 65: 1205–11. |
| [708] | Alqurashi W, Ellis AK. (2017). Do corticosteroids prevent biphasic anaphylaxis? J Allergy Clin Immunol Pract., 5:1194–205. |
| [709] | Nolan, J. P., Berg, R. A., Callaway, C. W., Morrison, L. J., Nadkarni, V., Perkins, G. D., Sandroni, C., Skrifvars, M.B., Soar, J., Sunde, K. and Cariou, A. (2018). The present and future of cardiac arrest care: international experts reach out to caregivers and healthcare authorities. Intensive Care Medicine, 44(6), 823–832. doi:10.1007/s00134-018-5230-9. |
| [710] | Nolan JP, Berg RA, Bernard S et al (2017) Intensive care medicine research agenda on cardiac arrest. Intensive Care Med., 43:1282–1293. |
| [711] | Kleinman ME, Perkins GD, Bhanji F et al (2018) ILCOR scientific knowledge gaps and clinical research priorities for cardiopulmonary resuscitation and emergency cardiovascular care: a consensus statement. Resuscitation, 127:132–146. |
| [712] | Coute RA, Panchal AR, Mader TJ, Neumar RW (2017) National institutes of health-funded cardiac arrest research: a 10-year trend analysis. J Am Heart Assoc., 6:e005239. |
| [713] | Buick JE, Drennan IR, Scales DC et al (2018) Improving temporal trends in survival and neurological outcomes after out-of-hospital cardiac arrest. Circ Cardiovasc Qual Outcomes, 11: e003561. |
| [714] | van Belle G, Mentzelopoulos SD, Aufderheide T, May S, Nichol G (2015) International variation in policies and practices related to informed consent in acute cardiovascular research: results from a 44-country survey. Resuscitation, 91:76–83. |
| [715] | Mentzelopoulos SD, Bossaert L, Raffay V et al (2016) A survey of key opinion leaders on ethical resuscitation practices in 31 European countries. Resuscitation, 100: 11–17. |
| [716] | Nichol G, Powell J, van Ottingham L et al (2006) Consent in resuscitation trials: benefit or harm for patients and society? Resuscitation, 70:360–368. |
| [717] | Nichol G, Leroux B, Wang H et al (2015) Trial of continuous or interrupted chest compressions during CPR. N Engl J Med., 373:2203–2214. |
| [718] | Flight L, Julious SA, Goodacre S (2017) Can emergency medicine research benefit from adaptive design clinical trials? Emerg Med J., 34:243–248. |
| [719] | Emerson SS, Fleming TR (2010) Adaptive methods: telling “the rest of the story”. J. Biopharm Stat., 20:1150–1165. |
| [720] | Laptook AR, Shankaran S, Tyson JE et al (2017) Effect of therapeutic hypothermia initiated after 6 hours of age on death or disability among newborns with hypoxic-ischemic encephalopathy: a randomized clinical trial. JAMA, 318:1550–1560. |
| [721] | Frobert O, Lagerqvist B, Olivecrona GK et al (2013) Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med 369:1587–1597. |
| [722] | James S, Rao SV, Granger CB (2015) Registry-based randomized clinical trials—a new clinical trial paradigm. Nat Rev. Cardiol., 12:312–316. |
| [723] | Lauer MS, D’Agostino RB Sr (2013) The randomized registry trial the next disruptive technology in clinical research? N Engl J Med., 369:1579–1581. |
| [724] | Nichol G, Brown SP, Perkins GD et al (2016) What change in outcomes after cardiac arrest is necessary to change practice? Results of an international survey. Resuscitation, 107:115–120. |
| [725] | Booth CM, Eisenhauer EA (2012) Progression-free survival: meaningful or simply measurable? J Clin Oncol 30: 1030–1033. |
| [726] | Dancey JE, Dodd LE, Ford R et al. (2009) Recommendations for the assessment of progression in randomised cancer treatment trials. Eur J Cancer, 45:281–289. |
| [727] | Gaudry S, Messika J, Ricard JD et al (2017) Patient-important outcomes in randomized controlled trials in critically ill patients: a systematic review. Ann Intensive Care, 7:28. |
| [728] | Haywood K, Whitehead L, Nadkarni VM et al. (2018) COSCA (Core Outcome Set for Cardiac Arrest) in adults an advisory statement from the International Liaison Committee on resuscitation. Resuscitation, 127:147–163. |
| [729] | Ji C, Lall R, Quinn T et al (2017) Post-admission outcomes of participants in the PARAMEDIC trial: a cluster randomised trial of mechanical or manual chest compressions. Resuscitation, 118:82–88. |
| [730] | Agarwal S, Presciutti A, Roth W et al (2018) Determinants of long-term neurological recovery patterns relative to hospital discharge among cardiac arrest survivors. Crit. Care Med., 46: e141–e150. |
| [731] | Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE (2012) Knowledge translation of research findings. Implement Sci., 7:50. |
| [732] | Perkins GD, Neumar R, Monsieurs KG et al. (2017) The International Liaison Committee on resuscitation—review of the last 25 years and vision for the future. Resuscitation, 121:104–116. |
| [733] | Norton WE, McCannon CJ, Schall MW, Mittman BS (2012) A stakeholder driven agenda for advancing the science and practice of scale-up and spread in health. Implement Sci., 7:118. |
| [734] | Sawyer, K. N., Camp-Rogers, T. R., Kotini-Shah, P., Del Rios, M., Gossip, M. R., … Moitra, V. K. (2020). Sudden Cardiac Arrest Survivorship: A Scientific Statement from the American Heart Association. Circulation, 141, e1-e32. doi:10.1161/cir.0000000000000747. |
| [735] | Woolcott, O. O., Reinier, K., Uy-Evanado, A., Nichols, G. A., Stecker, E. C., Jui, J., & Chugh, S. S. (2020). Sudden Cardiac Arrest with Shockable Rhythm in Patients with Heart Failure. Heart Rhythm. 1672-1678. doi:10.1016/j.hrthm.2020.05.038. |
| [736] | Miah, M.R., Hasan, M.M., Parisa, J.T., Alam, M.S., Akhtar, F., Begum, M., Shahriar, C.S., Sayok, A.K., Abdullah, F., Shamsuddin, M.A.S., Rahman, M.S., Sharif, M.A., Rahman, A.A.M.S., Alam, M.S., Uddin, M.B. and Chowdhury, S.H. (2021). Unexpected Effects of Advanced Wireless Sensor Technology on Climate Change, World Environment, 11(2), 41-82. doi: 10.5923/j.env.20211102.01. url: http://article.sapub.org/10.5923.j.env.20211102.01.html. |



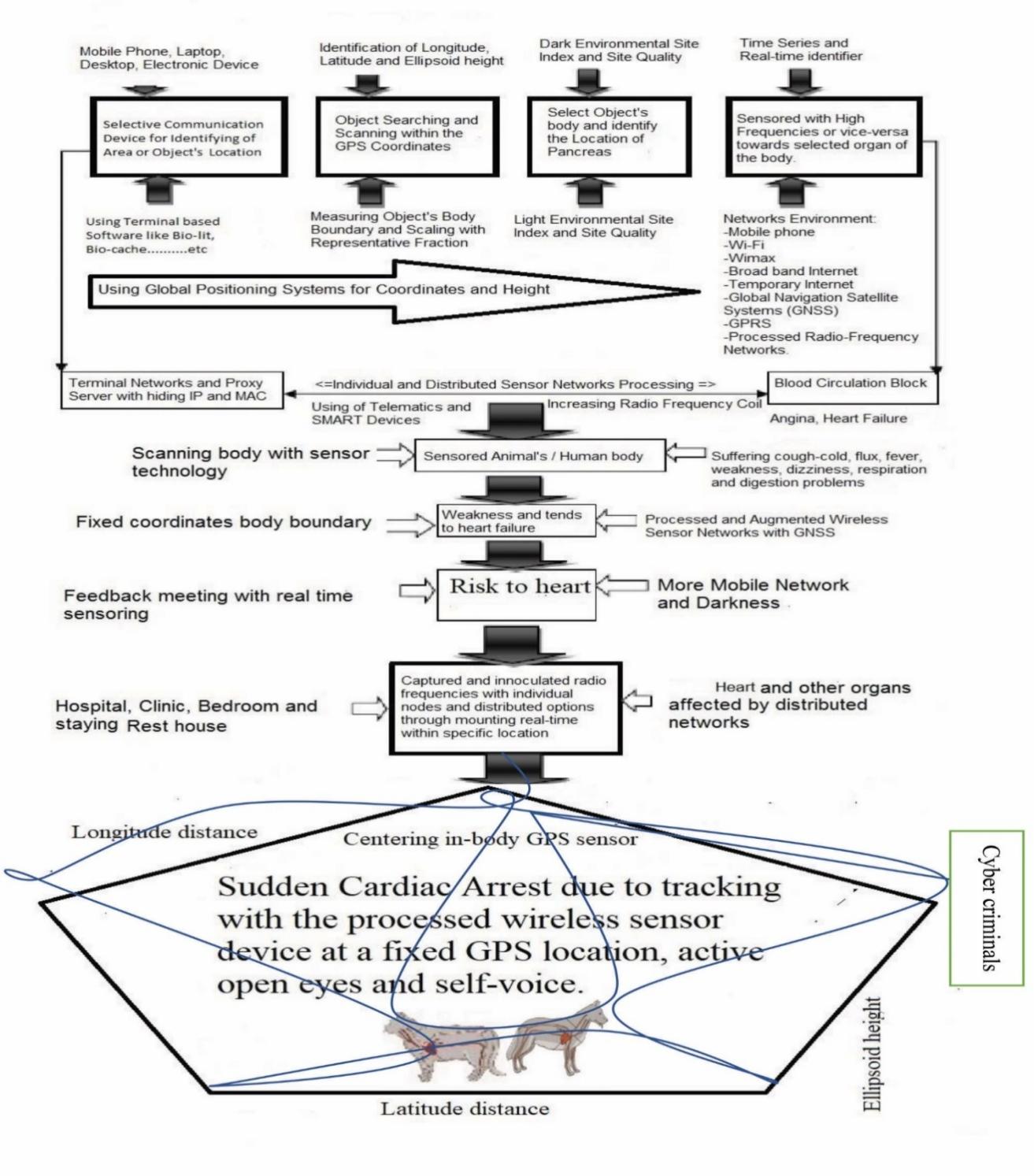
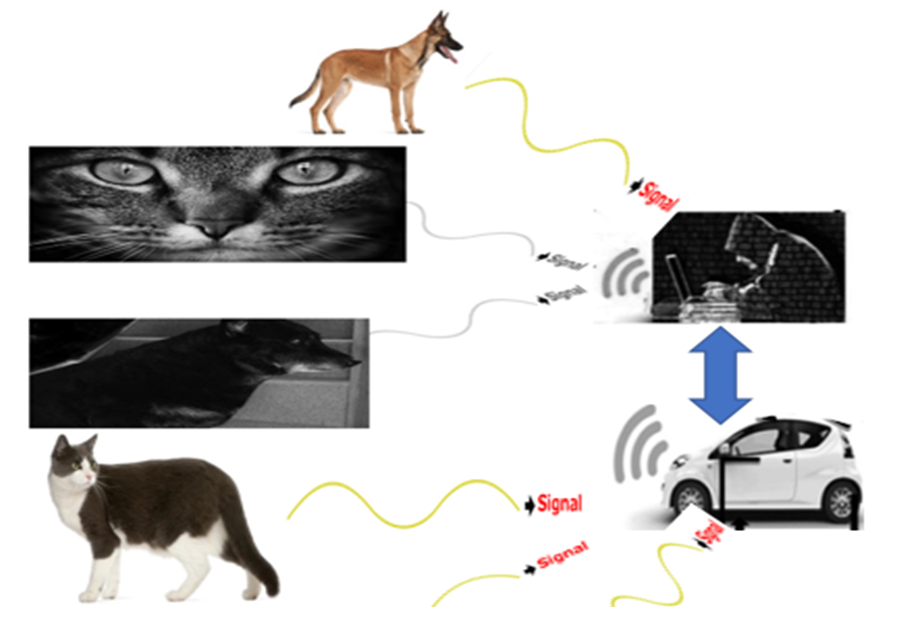
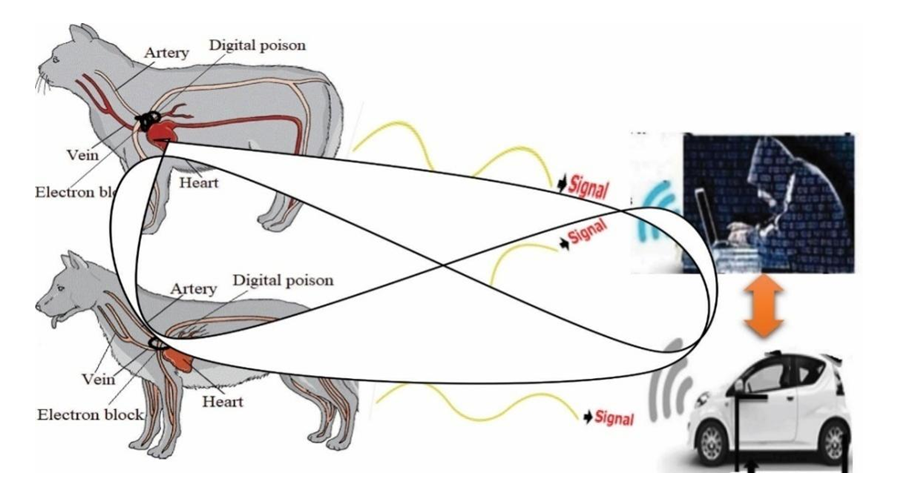
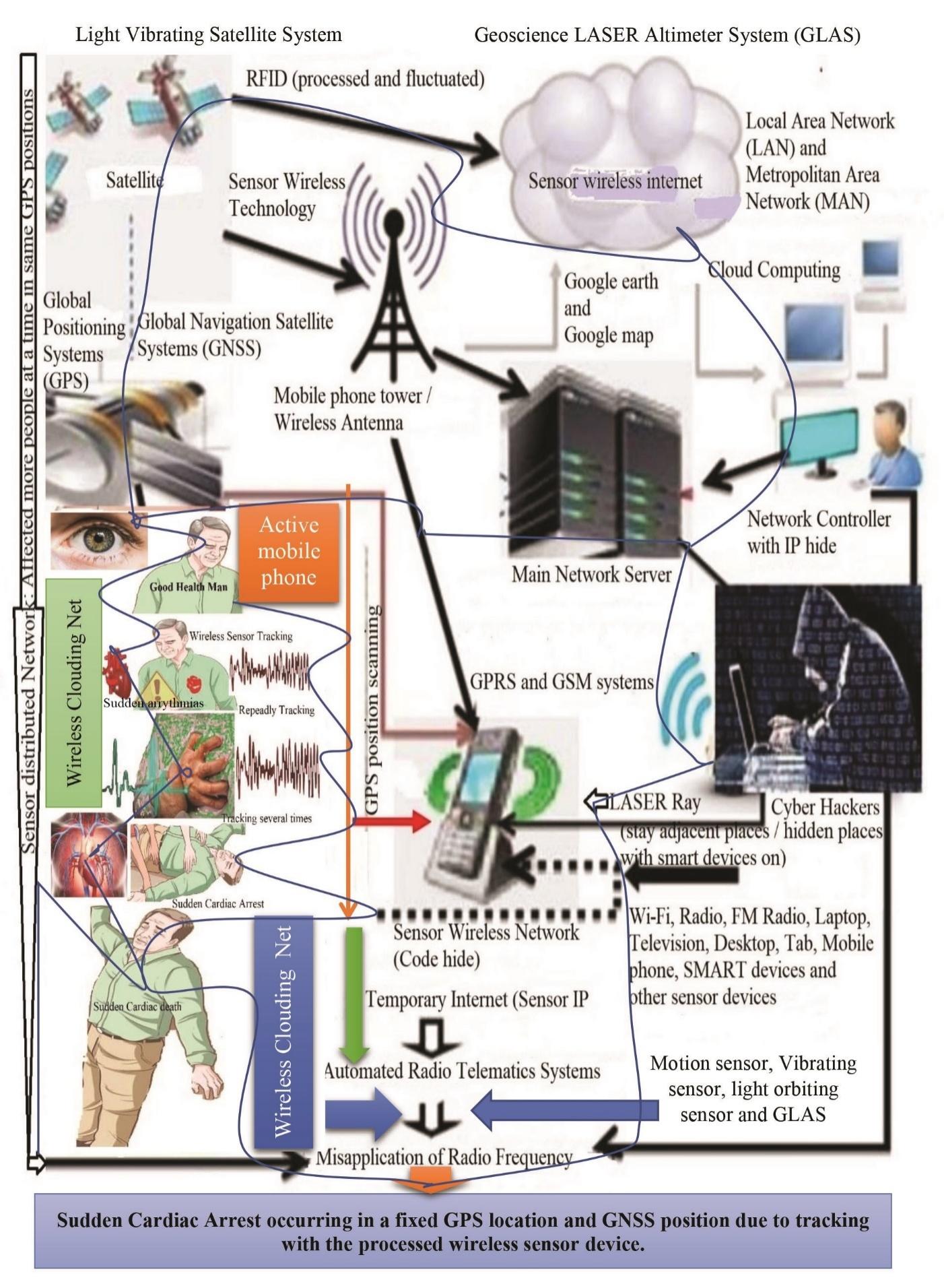
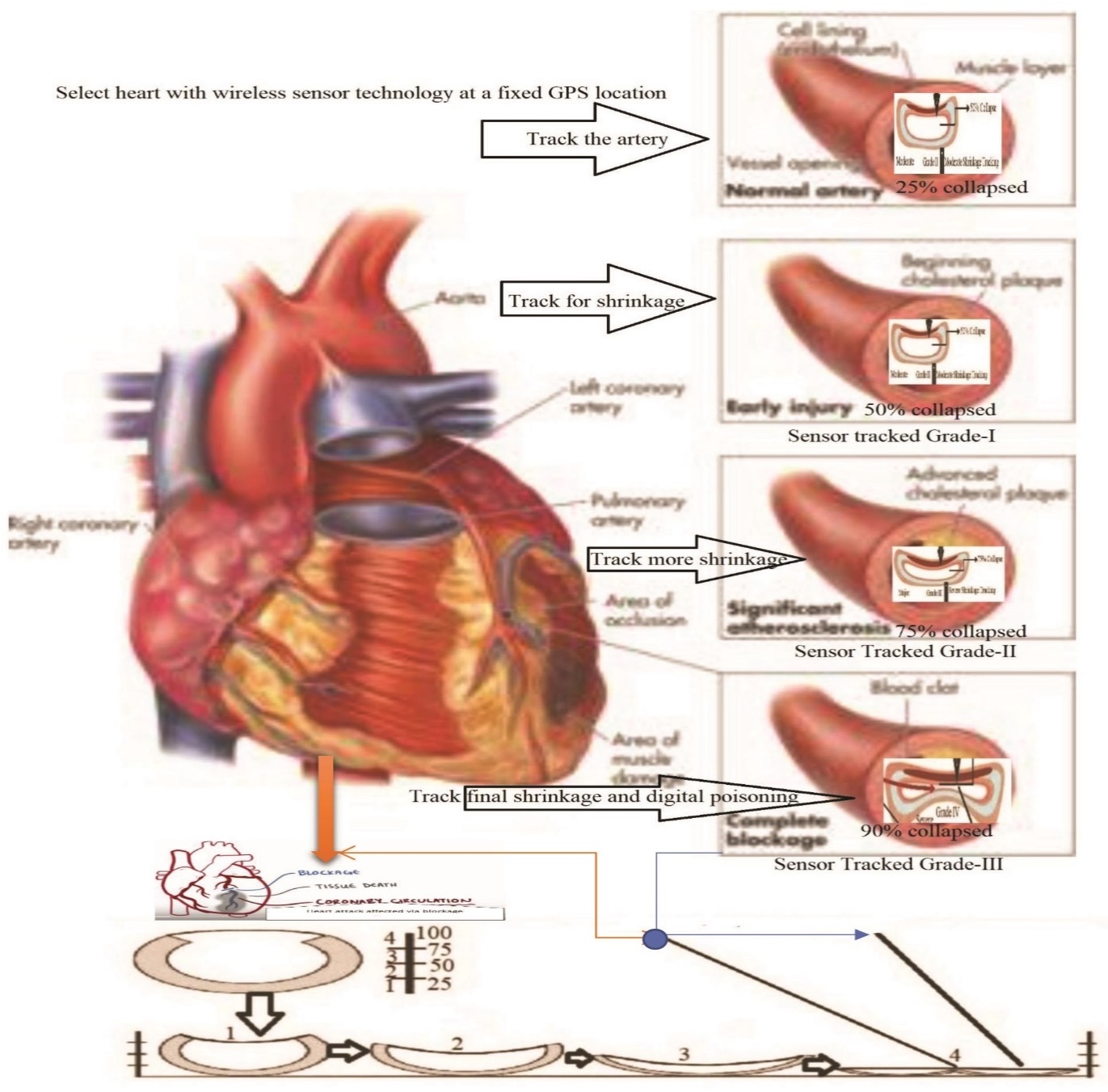
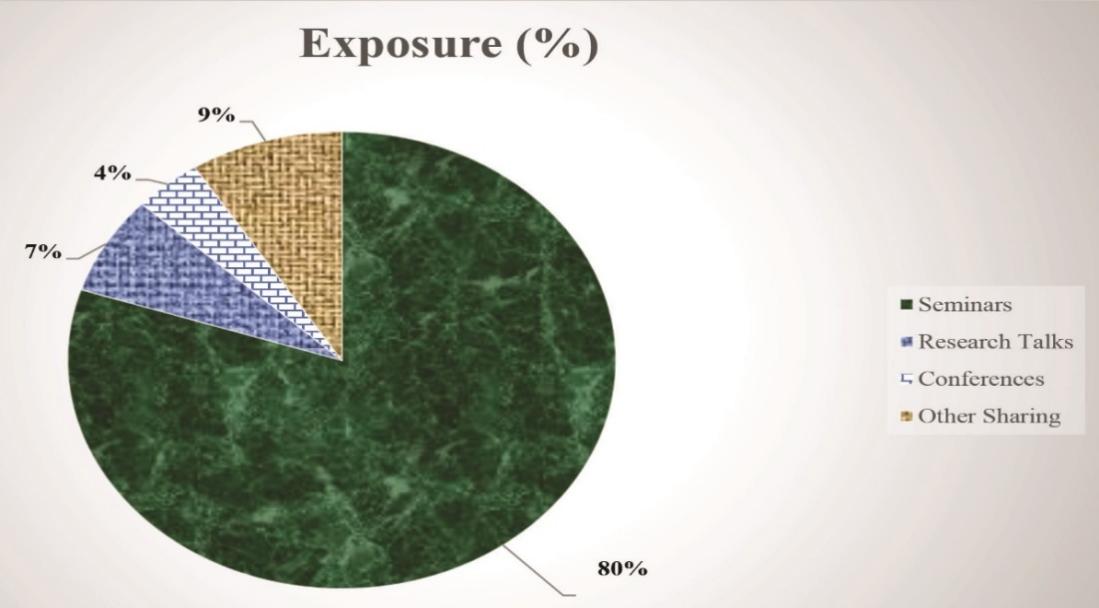
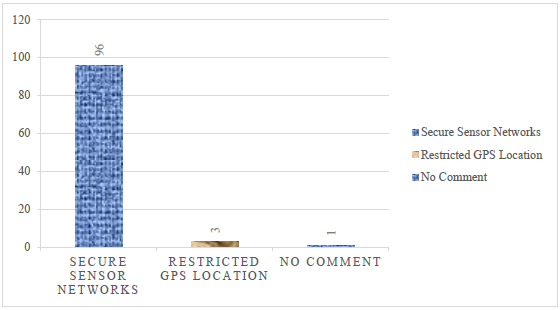
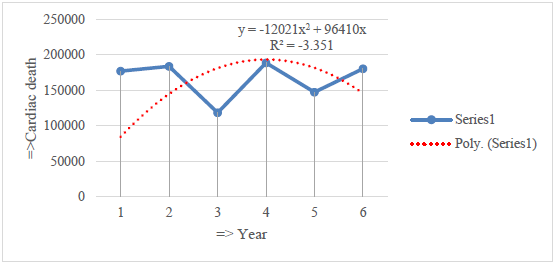
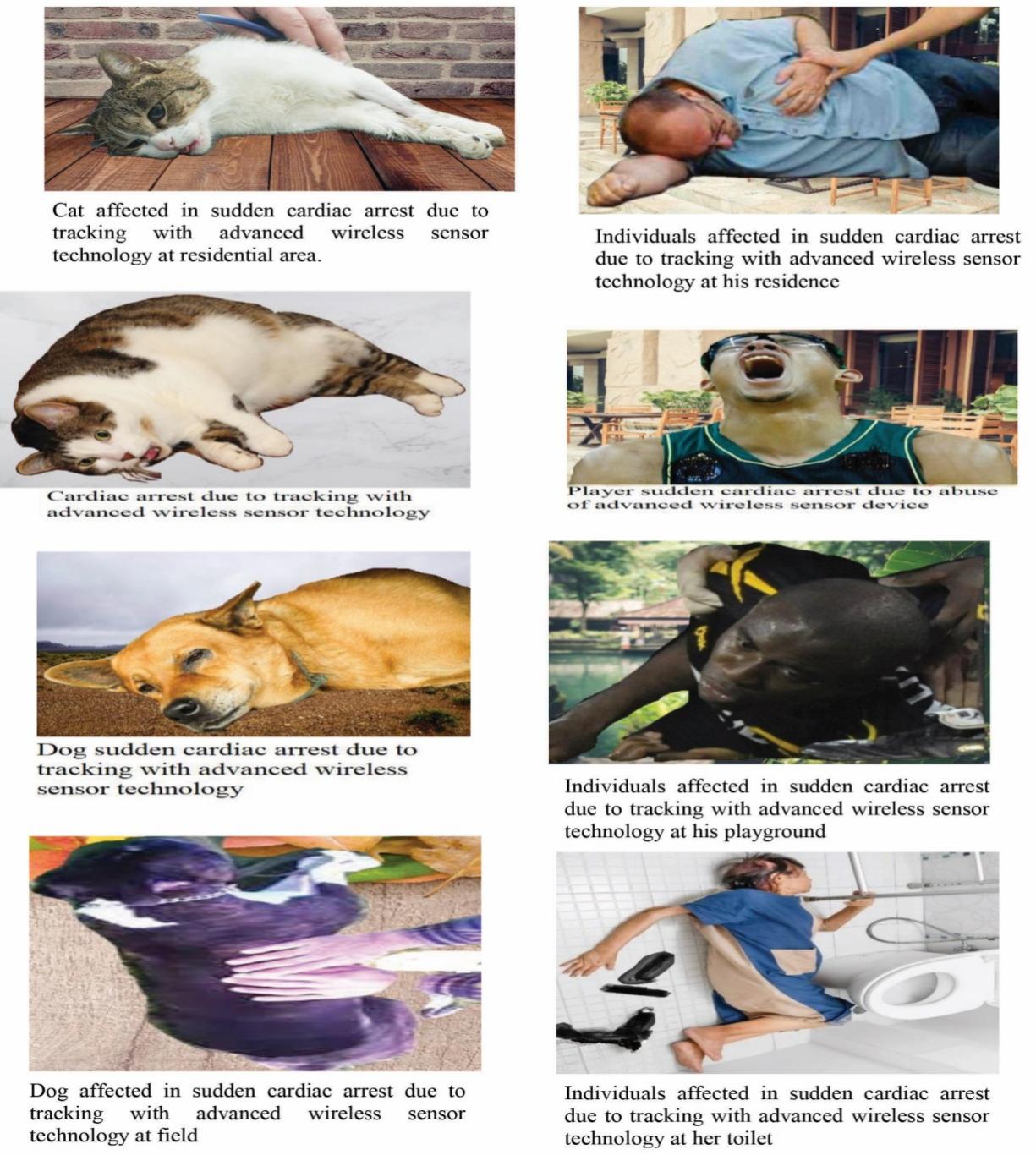
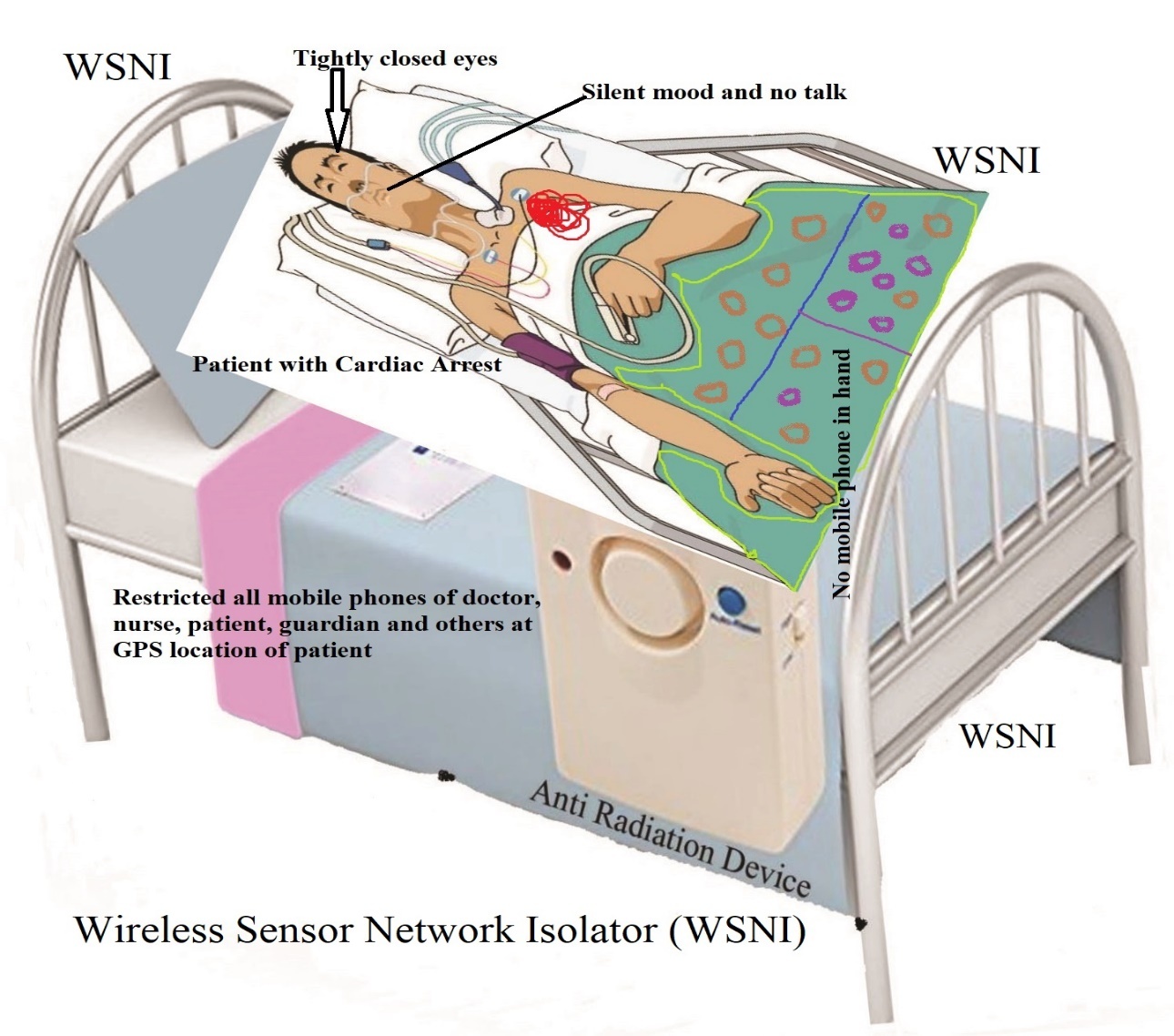
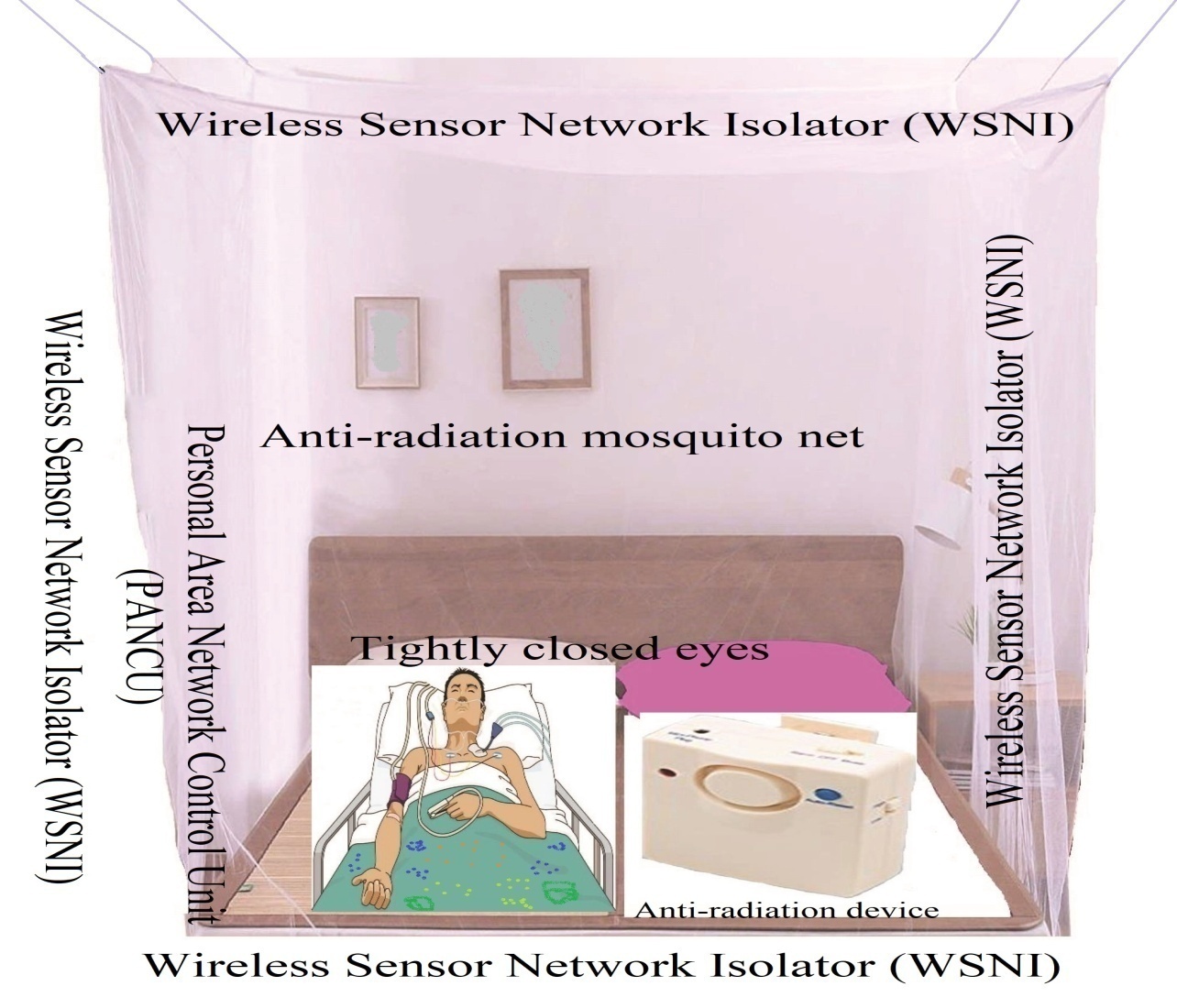
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML