-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2021; 10(1): 1-5
doi:10.5923/j.ijim.20211001.01
Received: Jan. 5, 2021; Accepted: Jan. 26, 2021; Published: Feb. 6, 2021

Impact of Birth-Defect in Heart along with Frequent Lower Airway Infection
Md. Shahariar Khan1, Manjur Hossain2, Md. Rahimullah Miah3, Tania Hussain1, Mohammad Basir Uddin1, Syed Moosa M. A. Quaium1
1Department of Paediatrics, Northeast Medical College & Hospital, Sylhet, Bangladesh
2Directorate General of Family Planning, Dhaka, Government of Peoples Republic of Bangladesh
3Department of Information Technology in Health, Northeast Medical College & Hospital Pvt. Ltd, Sylhet, Bangladesh
Correspondence to: Md. Shahariar Khan, Department of Paediatrics, Northeast Medical College & Hospital, Sylhet, Bangladesh.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Airway Tract Infections (ATIs) are one of the most common reasons for physician visits and hospitalization is associated with significant morbidity and mortality. There are many children suffering from frequent lower airway infections (FLAI). A significant number of congenital heart diseases (CHD) remain behind the FLAI but these could not be diagnosed due to lack of practices, investigation facilities, regularly follow-up and proper knowledge. The aim of the study is to identify the impact of birth-defect in heart among patients with FLAI. Methodology: This was a prospective observational study conducted in the Department of Paediatrics in Medical College Hospital over a period of 6 months. Total 50 cases of FLAI were included and data were collected in respect to history, examinations and diagnosis. Results: Out of these 36% of cases were diagnosed as CHD which are related to FLAI and 64% cases were remaining solely FLAI without any CHD. Conclusion: From the study, birth-defect in heart is an important cause of frequent lower respiratory infection. It can be prevented for earlier recognition and effective treatment. The study explores for future research trajectories for improvement of physical condition in children for proper diagnosis and prevention of recurrent attack by proper management.
Keywords: Birth-defect, Heart, Lower, Airway-infection, Frequent
Cite this paper: Md. Shahariar Khan, Manjur Hossain, Md. Rahimullah Miah, Tania Hussain, Mohammad Basir Uddin, Syed Moosa M. A. Quaium, Impact of Birth-Defect in Heart along with Frequent Lower Airway Infection, International Journal of Internal Medicine, Vol. 10 No. 1, 2021, pp. 1-5. doi: 10.5923/j.ijim.20211001.01.
Article Outline
1. Introduction
- Now a day’s child mortality is high globally. About 6.3 billion children less than 5 years die in every year all over the world [1]. Airway Tract Infections (ATI) are the major causes of childhood morbidity and mortality all over the world [2]. This is even more common in under-five age in developing countries. About the 16% of deaths of children under this age occurred due to respiratory infections which are about 50,000 in each year and around 80,000 children less than five years are admitted to hospital with this illness in each year [3]. The common acute lower respiratory infection includes pneumonia, bronchiolitis, acute bronchitis, influenza and whooping cough etc. which are the main cause of death in children over the world [4]. In most of the cases, there occurred frequent lower airway infections (FLAI), which also known as recurrent respiratory infection (RRI) can be regarded as 3 or more annual episodes of respiratory infections may merit further investigation for an underlying cause [5]. Lower respiratory infection (LRI) is too much common caused by viruses, bacteria, fungi and others [6]. There are many predisposing factors for FLAI like severe protein energy malnutrition, congenital and acquired immunodeficiency states [7]. Major manifestations include fever and dry cough and dyspnea in infants and young children [8].At present the most common type of birth-defect is congenital heart defect worldwide [9].The main causes of CHD among most children are unknown, but mother’s relevant conditions such as pre-existing diabetes and obesity are also associated to birth-defects in child [10]; [11]. Some congenital heart diseases causing increase pulmonary blood flow which is a common risk factors for pneumonia in children [12]. Ventricular septal defect atrial septal defect, patent ductus arteriosus and atrioventricular septal defect are common acyanotic CHD in children that predisposed to RRI [13]. In acyanotic congenital heart diseases because of left to right shunting of blood, via a septal defect or the arterial duct, there occurred pulmonary over circulation and pulmonary oedema leads to develop congestive cardiac failure (CCF) and become a source of infection for the lower respiratory infections. So FLAI and the CCF may be the first clinical presentations of an underlying CHD. Most previous studies have shown that CHD as an underlying cause of recurrent ARI. This is more so as the co-existence of FLAI and CHD may increase the mortality in children. The age of onset and the severity of symptoms in children with CHD are depending on the size of the defects [14]. In this study children with FLAI will go for chest X-ray, ECG and echocardiography to identify those with underlying CHD. The aim of the study is to know the impact of birth-defect in heart amongst the children with FLAI will determine.
2. Materials and Methods
- This was a prospective observational study conducted in the department of Paediatrics in Northeast Medical College Hospital (NEMCH), Sylhet between the months of May, 2020 to December, 2020 over a period of eight months. Sample size was fifty (50) in number. Data CollectionPrimary data collected from the NEMCH in Bangladesh pertaining on RRI in children from the existing ward and outpatient department. Meanwhile secondary data were collected from diverse sources like ICDDRB, NEMCH central library, Journals, daily news, books, different web pages and relevant update sources. Informal Discussion Informal discussion is integrated with the patient’s guardian like father, mother, grandmother, aunt, uncle etc. at Northeast Medical College Hospital. Some hospital data were collected through informal counseling with them to observe patient’s complication/ major problems. This discussion method was also used to be aware with them to recover from this illness.Selection Criteria a. Inclusion criteria Age group range between 2 months to 5 years, recurrent cough and cold, fever, breathing difficulties, cyanosis, anemia, normal and abnormal breath sound, heart rate, respiratory rate, normal heart sound, added sound both in lungs and heart, hepatosplenomegaly, body weight, Percent saturation of Oxygen, EGC, Echocardiography and chest x-ray.b. Exclusion criteria The exclusion criteria are associated with other diseases, viral fever, congenital anomalies other than heart.Data Compilation All general information regarding RTI, its history, clinical examination, investigation and diagnosis were compiled according to research objective.Data Analysis and InterpretationCompiled data were integrated for analysis and interpretation as findings using standard data analysis software like SPSS version 26, MS Excel 2016 and R programming version 3.5.
3. Results
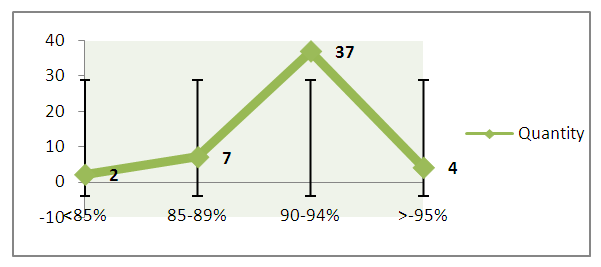
- a. Age GradationFrom survey at NEMCH, the incidence of the disease is maximum in within one year and secondly between 1 to 2 year but minimum in between 4 to 5 year which as shown in Figure 1. The figure also illustrated with Linear graph to compare with different years of occurrence of this disease in children.
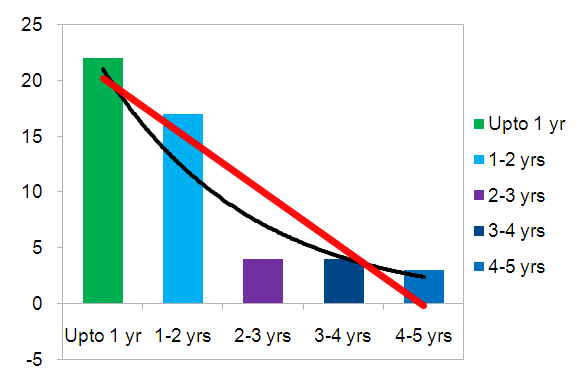 | Figure 1. Incidence of disease in different years at Department of Paediatrics of NEMCH |
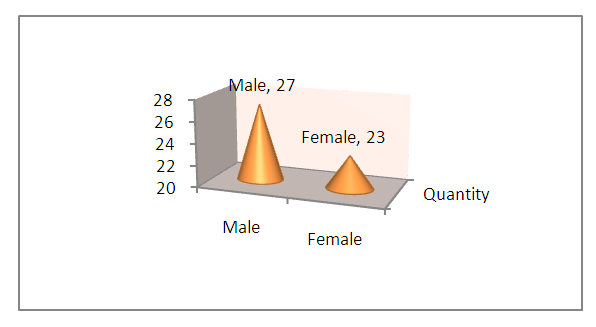 | Figure 2. Sex variations in different Patient Status at Department of Paediatrics of NEMCH |
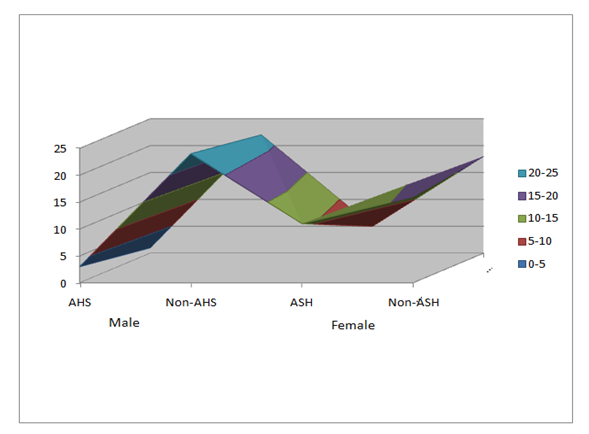 | Figure 3. The rate of normal and abnormal heart sound and also presence of added sound in the heart |
 | Figure 4. The percent saturation of Oxygen in various children admitted in Padeatric ward |
 | Figure 5. X -ray finding of heart in all Children |
 | Figure 6. Ratio of CHD and non-CHD in echocardiography |
4. Discussion
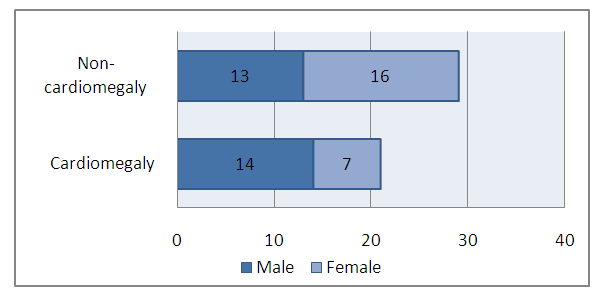
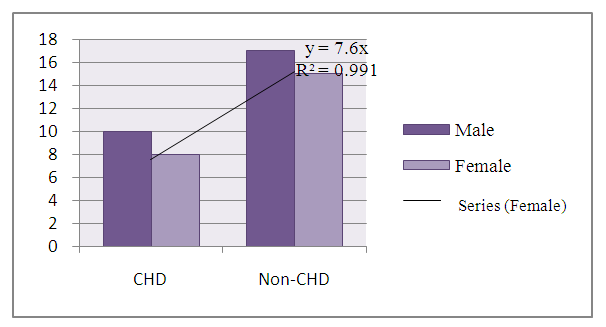
- The study illustrated on patients’ status with FLAI at the Department of Paediatrics in Northeast Medical College Hospital over a period of 8months. During this study, fifty patients were included. Cases were noted in respect to history, clinical examinations & investigations. The results were analyzed as follows: among them, the incidence of the disease is maximum in within one year and secondly between 1 to 2 years but minimum between 4 to 5 years. Males are more predominant than females. The findings exposed to the rate of abnormal heart sound of those children is very minimum which is only 8%, otherwise the normal heart sound is 92%. The added sound present in the heart is 32% and absent in 68%. From field observation, the percentage of Oxygen saturation in majority of patients remains in between the saturation level of 85 to 90%. Heart was enlarged in 42% of child and CHD was diagnosed in 36% of cases on echocardiography. Over the last 30 years there has been an increasing wakefulness regarding the significance of early referral of newborn with heart disease to special centers [15]. Most CHD are asymptomatic and diagnosed during routine neonatal checkup [16]. As it is a good number of common among major birth defect, put a significant economic burden and emotional impact on affected families and treatment is expensive, it is very significant to discover its pattern among children [17]. In the western countries pattern of CHD is well documented, but has not been studied nationwide in Bangladesh as in other western and neighboring countries [18]. It is not a standing condition; changes take place all through patient’s life end-of-life care [19]. Continuous advances in technology and training in Paediatric cardiology and pediatrics have improved long term benefit and promised better quality of life [20]. If CHD is left untreated is an important cause of morbidity and mortality in children, therefore early identification and appropriate intervention is most important [21]. As the incidence of CHD is increasing in Bangladesh, the magnitude of the problem is gradually becoming alarming in the country [18]. The present number of qualified personnel for pediatric cardiology is inadequate [22]. The purpose of this study was to screen of all the children with recurrent RTI either admitted or not in order to identify the congenital heart disease remain behind them. Early recognition of CHD is very significant for proper management purposes and so accurate clinical examination and expert echocardiography is considered a gold standard for the diagnosis of CHD [23]. Two dimensions echocardiography is also necessary for the diagnosis and special cardiac center should be established in our region in order to manage the patient successfully without delay that may affect the out- come of the disease [24]. With the advanced medication and management, children associated with CHD will live longer and lead a healthy life [9]. However, the special emphasis needs to provide for the children below 2 years to recover from birth-defect in heart.
5. Conclusions
- In case of children with FLAI, congenital heart disease is an important cause remains behind it. So, if we can remind that each and every child with FLAI should be investigated properly to search any CHD present or not. Then by giving proper treatment of CHD, FLAI can be prevented more. Parents counseling is very important to understand the evaluation of this condition. That wise we can prevent the infant and childhood mortality in our country and correlate the existing national policy in connection with Sustainable Development Goals 2030 [25]. For this purpose, the research recommends for future research trajectory.
Disclosure
- Data AvailabilityThe data are being used to support the findings of this research work are available from the corresponding author upon request. Competing InterestsThe authors declare no potential conflict of interests in this research work.
ACKNOWLEDGEMENTS
- The authors acknowledged the authority of NEMCH, Sylhet, Bangladesh for kind support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML