-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2020; 9(2): 30-32
doi:10.5923/j.ijim.20200902.02
Received: Oct. 18, 2020; Accepted: Nov. 13, 2020; Published: Nov. 28, 2020

Persistence of Positive SARS-COV-2 RNA in Asymptomatic COVID-19: A Case Report
Alagesan Sundaram1, Amutha VP2, Ravichandran Murugan1, Shantaraman Kalyanaraman3
1Department of General Medicine, Tirunelveli Medical College & Hospital, Tirunelveli
2Department of Microbiology, Tirunelveli Medical College & Hospital, Tirunelveli
3Department of Pathology, Tirunelveli Medical College & Hospital, Tirunelveli
Correspondence to: Shantaraman Kalyanaraman, Department of Pathology, Tirunelveli Medical College & Hospital, Tirunelveli.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: The first case of COVID-19 pandemic in India was reported on 30th January 2020. As of 4th May, the Ministry of Health and Family Welfare have confirmed a total of 42,836 cases, 4762 recoveries and 1389 deaths in the country. According to ICMR1 65% of Covid patients in India were asymptomatic and 31% were symptomatic. Most of the asymptomatic cases, clearance of SARS-COV-2 RNA occur within two weeks. We report a confirmed case of COVID-19 positive asymptomatic patient whose nasopharyngeal swab test of SARS-COV-2 RNA shows persistent positivity for 40 days. This case shows the significance of active surveillance of SARS-COV-2 RNA for infectivity assessment.
Keywords: COVID-19, SARS-CoV-2, Novel corona virus, Asymptomatic, Infectivity
Cite this paper: Alagesan Sundaram, Amutha VP, Ravichandran Murugan, Shantaraman Kalyanaraman, Persistence of Positive SARS-COV-2 RNA in Asymptomatic COVID-19: A Case Report, International Journal of Internal Medicine, Vol. 9 No. 2, 2020, pp. 30-32. doi: 10.5923/j.ijim.20200902.02.
1. Background
- The COVID-19 an ongoing pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The outbreak was first reported from Wuhan, China, (December 2019) [1] followed by a World Health Organization declaration of a Public Health Emergency of International Concern (30 January 2020), and as a pandemic (11 March 2020). By mid May 2020 the pandemic has already affected more than 4.9 million people with 3.2 lakhs reported deaths, in 180 countries, the scale of infectivity being predominantly attributed to respiratory droplets and hand contact. It has been reported that 80-81% of the COVID-19 patients are asymptomatic or mildly symptomatic, 14-15% patients have severe clinical symptoms and 2-3% end with mortality. This COVID Isolation Facility in rural south India reports here a patient who presented with COVID-19, was asymptomatic through the entire course of the disease but paradoxically had persistent positivity for are positive for SARS–COV-2 RNA in RT PCR test from nasopharyngeal swabs.
2. Case Report
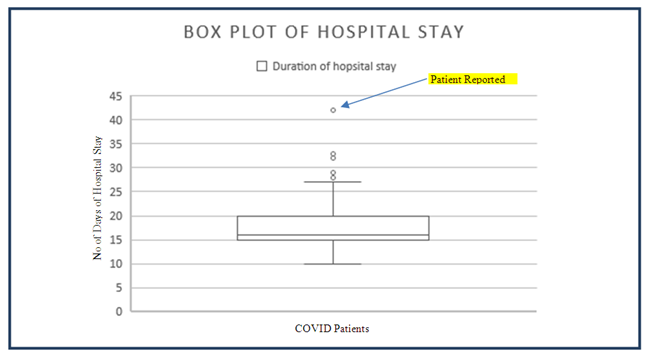
- A 60 year old man from a rural region of this district was identified as a primary contact of a COVID-19 positive patient who was admitted to this hospital. He self-disclosed his contact with the COVID-19 infected person with fever, on return from travel outside the country. He was interviewed and examined at the COVID Isolation Facility of this hospital on arrival and had no fever, sore throat, cough or shortness of breath. He had no co-morbid diseases like diabetes mellitus, systemic hypertension, coronary heart disease or cancer. He was not a smoker, nor an alcoholic. He was well nourished, normal weight for height and was a preferred non-vegetarian. He had no history of previous diseases or medication use. On examination, his vital signs including the oxygen saturation (99%) were normal. His respiratory and cardio-vascular examination were within normal limits. The nasopharngeal swab test of SARS-COV-2 RNA using qualitative real time reverse transcriptase polymerase chain reaction assay was performed in the Viral Research and Diagnostic Lab in this institute, under affiliation with the Indian Council of Medical Research, New Delhi. The standard operating procedures were as per ICMR protocols. The test confirmed the presence of COVID-19 infection.A wide set of clinical pathology and biochemistry tests were performed as per hospital protocol, including random blood glucose, renal function tests, liver function tests, CPK- MB, serum LDH, serum electrolytes and C reactive protein, D Dimer, Serum Ferritin, Serum Procalcitonin, alpha TNF and IL-6. All these tests were within the normal ranges. These tests were repeated as per standard operating procedures and were consistently normal. The X-ray and CT scan of the chest were also within normal limits. During his stay in the isolation facility he had no symptoms or clinical signs consistenly. He was under observation, was given standard hospital diet. As per the institutes protocol a nasopharngeal swab and RT-PCR was repeated on the 12th day of hospital stay, which was positive. Subsequently swab tests were done on day 16, 20, 25, 27, 31, 35, 39 and 42. He reported negative on the 42 day and was discharged.The cohort of COVID-19 patients who were admitted and treated during the same period, predominantly from the same location with similar racial and anthropological characteristics reported a median hospital stay of 16 days with a mean of 18 days and SD of 4.79. A box plot of the stay durations was evident that this patient had taken an abnormally long period of turning negative.
3. Discussion
- The COVID-19 infection, an ongoing global pandemic of novel corona virus infection caused by the SARS-COV-2, was declared as a public health emergency of international concern and later as a pandemic by the WHO. The clinical spectrum of the disease varies from asymptomatic cases, mild symptoms to life threatening ARDS and multiple organ dysfunction. It has also been reported that asymptomatic carriers, persons in incubation period and patients in convalescence may be infectious. The SARS-CoV-2 patients can replicate and shed virus in their upper respiratory tract, even if pre-symptomatic. [2] This 60 year old patient did not show any symptoms and was healthy by clinical standards all through the 42days of hospital stay.Severe COVID-19 presents with high leukocyte count, and increased levels of plasma cytokines [3]. Additionally, high values of blood C-reactive protein, erythrocyte sedimentation rate and D-dimer are also reported. [4] High blood levels of cytokines reported in these patients include IL1-β, IL1RA, IL7, IL8, IL9, IL10, basic FGF2, GCSF, GMCSF, IFNγ, IP10, MCP1, MIP1α, MIP1β, PDGFB, TNFα, and VEGFA. These high levels are seen in patients in ICU and hence are indicators of clinical severity. [5] This peculiar feature of SARS-CoV-2 infection being capable of shedding virus even when asymptomatic and lack of cytokine releases in these persons, result in an inability to make a symptom-based detection in contrast to SARS CoV-1 patients. [6,7] Our patient had normal cytokine values and all of his laboratory tests were unremarkable. His x-ray was also clear and unremarkable. Hoehl et al. (2020) reported that in 2 of 114 Germans evacuated from Hubaei province of China had no symptoms and were RT-PCR positive. These two persons were confirmed to be potentially infectivity by virus culture [8]. This indicates that our patient was potentially infective during the long period of stay of 42 days and more so testing of asymptomatic patients before release from isolation has definite benefit in the context of disease containment and prevention of community spread of disease.While all the patients who were admitted alongside this person belonged to a similar racial group and had contracted the disease from a single source in New Delhi during a religious congregation. Of 38 individuals who were identified as index and primary contacts and 14 others identified as secondary contacts, all of these persons turned negative with the same treatment regimen over a period of 15-20 days with a median of 16 days and mean of 18days. There were 2 individuals who were outliers in this group of whom one turned negative in 29 days and other in 27 days. The question that remains unanswered in this experience is what is the role of the human genome and viral genome interactions in the causation of such resistance to turn negative, and more so needs specific explanation for the paradoxical behavior of the virus in being resistant to turn negative and the individual being asymptomatic. The immunological and genomic framework of the individual in this case series hold some answers for the global pandemic in terms of preventing mortality and sever clinical disease.
ACKNOWLEDGEMENTS
- We acknowledge the residents and interns of the department for their consistent effort in managing the COVID-19 patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML