-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2019; 8(3): 37-41
doi:10.5923/j.ijim.20190803.01

Causative Organisms of Catheter Associated Urinary Tract Infection in Medical Wards and Intensive Care Units
Fawkia E. Zahran1, Ahmed Ibrahim2, Sawsan A. Omer3, Sameh A. Elkohafy4, Gamil K. Mohammed5
1Internal Medicine Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
2Prince Sultan Cardiac Center - Alhassa, Saudi Arabia
3Internal Medicine Department, Faculty of Medicine, University of Gezira, Sudan, KFHH, KSA
4Lecturer of Anesthesia and surgical ICU, Faculty of Medicine, Tanta University, Egypt
5Cardiothoracic Surgery, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Correspondence to: Fawkia E. Zahran, Internal Medicine Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

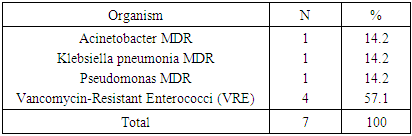
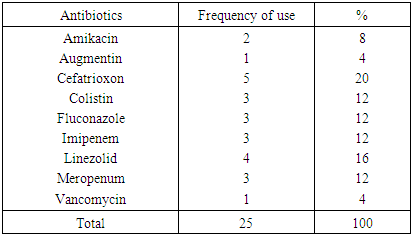
Background: Catheter associated urinary tract infection (CAUTI) is a urinary tract infection (UTI) where an indwelling catheter was in for more than two calendar days on the date of event (day one being the day of device placement). It is one of the most common hospital acquired infection and causes problems in hospitalized patients. Objectives: To review the overall occurrence of CAUTI, the demographic, clinical data and to determine the causative microorganisms of CAUTI in patients admitted in medical wards and intensive care unit (ICU) in KFHH secondary and tertiary hospital and to provide recommendations for prevention. Methods: This is cross-sectional prospective study of Catheter Associated Urinary Tract Infection (CAUTI) in medical wards and intensive care units. Only adult patients were included in this study. The data were collected from the patients ‘medical records. Results: About 30% of patients developed CAUTI; the majority of them were located in general wards. Although female had more CAUTI compared to male (33% versus 20%; P= 0.07) but the difference was not statistically significant. The most common isolated organisms among patients with CAUTI were: Candida yeasts (18%), E-coli, (3%) and pseudomonas (1%). Isolated multidrug resistant (MDR) organisms consisted about 10% of total isolated organism and most common isolated MDR organism is Vancomycin-Resistant Enterococci (VRE) 50% from total MDR. The most commonly used antibiotics for CAUTI in these patients were; ceftriaxone, linezolid, Carbepenem and Fluconazole. Conclusion: CAUTI was most common in patients admitted in wards than ICU. It was more common in females. Approximately one third of patients had CAUTI. Majority of patients had no urinary symptoms. Candida yeasts was the most common isolated microorganisms among patients with CAUTI.
Keywords: Urinary catheter, Urinary tract infection, ICU, Ward, Bacteria
Cite this paper: Fawkia E. Zahran, Ahmed Ibrahim, Sawsan A. Omer, Sameh A. Elkohafy, Gamil K. Mohammed, Causative Organisms of Catheter Associated Urinary Tract Infection in Medical Wards and Intensive Care Units, International Journal of Internal Medicine, Vol. 8 No. 3, 2019, pp. 37-41. doi: 10.5923/j.ijim.20190803.01.
Article Outline
1. Introduction
- Urinary tract infections (UTI) are the most common hospital-acquired infections in humans and are caused primarily by uropathogenic Escherichia coli (UPEC). Indwelling urinary catheters become encrusted with UPEC biofilms that are resistant to common antibiotics, resulting in catheter associated urinary tract infections, and may lead to chronic infection. [1]. Catheter can be made from rubber, plastic or silicone and there are many types of catheters like, indwelling catheter that resides in the bladder and it is also known as Foley catheter. External catheters and short term catheters are other types of catheters. It is estimated for more than 30% of infections reported by acute care hospitals [2]. CAUTI is defined as a symptomatic patient with a urinary catheter (UC) had one or more of the following symptoms or signs, with no other recognized infection: fever (temperature ≥38°C), urinary urgency, frequency, dysuria, or suprapubic tenderness, with positive urine culture with no more than two pathogens isolated. [3]. In Europe, the mortality rate of nosocomial infections is 10%; 97% of which is related to catheters. Around 80% of nosocomial urinary tract infections are associated with indwelling urinary catheters. Antimicrobial resistant CAUTI can cause recurrent and chronic infections and if untreated it may cause acute or chronic pyelonephritis, bacterial vaginosis, chronic prostaitis, bacteraemia and death [4]. Significant risk factors for CAUTI include age, diabetes requiring insulin therapy, long hospitalization and long duration of catheter insertion [5] Enterococcus species, especially Enterococcus faecalis, Methicillin resistant Staphylococcus aureus (MRSA), Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Proteus mirabilis and Staphylococcus epidermidis are the main urinary pathogens that cause biofilm related urinary tract infections [4]. The biofilm formation by pathogenic microbes that protects pathogens from host immune defence and antimicrobial agents is the leading cause for CAUTI. The use of antimicrobial coating for urinary catheters in the past few years, was demonstrated to be one of the most direct and efficient strategies to reduce infections. [6]. The impact of a UTI on the individual can vary greatly, depending on age, co-morbidities and socio-economic circumstances. CAUTIs may lead to unnecessary use of antibiotics and antimicrobial resistance and longer hospital stays [7]. Virtually CAUTI is caused by instrumentation of the urinary tract and has been associated with increased morbidity, mortality, hospital cost, and length of stay. [8] UTI associated with catheterization may be extraluminal or intraluminal. Extraluminal infection occurs via entry of bacteria into the bladder along the bioform that forms around the catheter in the urethra. Intraluminal infection occurs due to urinary stasis because of drainage failure. [9]. However, 17% and 69% of CAUTI can be prevented through implementation of evidence-based bundle for CAUTI [10]. The aim of this study was to review the overall occurrence of CAUTI, the demographic, clinical data and to determine the causative microorganisms of CAUTI in patients admitted in medical wards and intensive care unit (ICU) in King Fahad Hofuf hospital medical wards and intensive care unit during May2017 to August 2017.
2. Study Methods
2.1. Study Design
- This is cross-sectional prospective study of Catheter Associated Urinary Tract Infection (CAUTI) in medical wards and intensive care units.
2.2. Study Setting
- The study was carried out at the Medical ward in King Fahad Hofuf hospital (KFHH) from May to August 2017. The bed capacity of about 210 beds include 15 beds in adult medical ICU. Bed occupancy rate 61.2% in medical ward and 100% in medical ICU, estimated average length of stay in medical ward about 4.9 days and medical ICU 9.8 days.
2.3. Study Population
- The study included all adult patients who were admitted to medical wards or ICU during the study period with medical conditions rather than UTI and had been catheterized with Foley’s catheter. The exclusion criteria were patient admitted with community acquired UTI, Foley’s catheter and those who were transferred from other hospital with indwelling urinary catheter.
2.4. Study Tools and Data Collection
- The data were collected from the patients ‘medical records in the wards and intensive care unit. The collected data included information on the demographic, clinical data, type and cause of admission, co-morbidities, risk factors, causes of urinary catheterization, number of patients who had any type of infection at admission, duration of devices use, number of days each Foley’s catheter use, type of Foley’s catheter, date of infection, type of isolated pathogen contribute to infection, antibiogram, prescribed antibiotic, dose and duration of antibiotics, length of hospital stay and outcome of CAUTI management.
2.5. Ethical Consideration
- The study proposal was approved by Research & Ethic Committee in KFHH and written informed consents were obtained from all patients to participate in the study.
3. Results
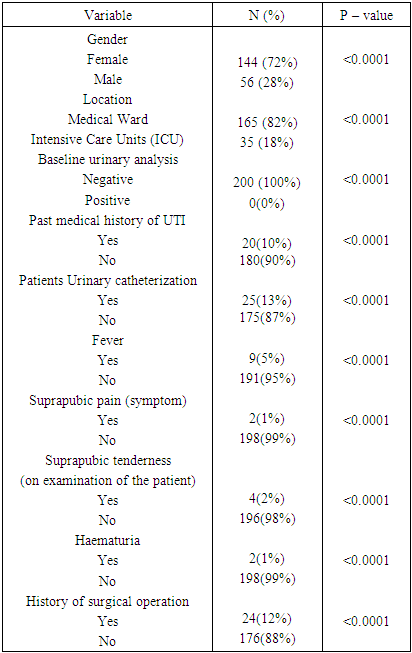
- The total number of patients in this study was 200 patients, 56 (28%) of them were males and 144 (72%) were females. The majority of the patients 165(82%) were allocated in general medical wards patients were in the while 35 (18%) patients were in intensive care unit (ICU), table 1. The mean age of the patients was 66.8 year.
|
|
|
|
4. Discussion
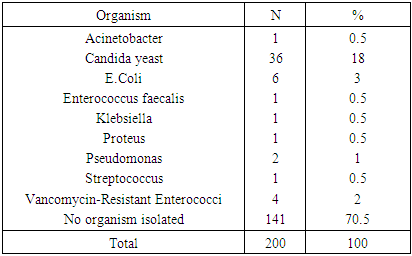
- The total number of patients in this prospective study was 200 patients, 56 were males (28%), 144 were females (72%). 165 (82%) patients were in the general medical wards while 35 patients (18%) were in intensive care unit (ICU). The mean age of the patients was 66.83 year. Past history of urinary tract (UTI) infection was found in 10% of patients. Base line urinary analysis was negative for bacteria for almost all patients. CAUTI was found in 29.55%, of patients, with the majority of them located in general wards than ICU. This may be explained by the fact that, in this study, there were large number of patients in general wards than ICU, in addition the care for catheter in ICU may be much better than in the general wards. CAUTI was significantly associated with female gender P-value 0.050. This was nearly similar to the study done in 3 Gulf Cooperation Council (GCC) countries in 6 hospitals in, Saudi Arabia, Oman, and Bahrain where they found that, the risk of CAUTI in GCC hospitals was 35%. [10]. In contrast to a study done in Abant Izzet Baysal University Hospital in Turkey were the incidence of CAUTI among143 catheterized inpatients was 13%. [11]. In another study carried out in Japan, to check the efficacy of antimicrobial catheter in CAUTI, the incidence of CAUTI was 8.8% and 8.3% in the control and antimicrobial catheter groups, respectively [12]. The significance association of CAUTI to female gender, may be explained by the fact that, the anatomic structure of females, where, a woman's urethra is closer to anus causing an easier access of the perennial flora to the bladder along the catheter as it traverses the shorter female urethra. The main symptom related to UTI, in this study was, fever, which was found in 5% of patients. This is as in the literature where, symptoms of CAUTI are not necessarily referred to the urinary tract and fever is the most common symptom. Microorganisms which were isolated from urine culture included: candida yeast in 36 patients (18%), E.coli in 6 (3%) of patients, vancomycin resistant enterococcus in 4 (2%), pseudomonas in 2 patients (1%), acentiobacter, enterococcus faecalis, klebsellia, proteus, and streptococcus, each occurred in 0.5% of patients. This is well known that prolonged catheterization can be associated with polymicrobial bacteriuria and they have easy access to the bladder via the catheter, a good example of such organisms is Candida species which almost never cause UTI in the absence of an indwelling catheter. Another explanation for cadiduria is the use of systemic antibiotics. Similarly, in a study in Egypt Candida constituted approximately 50% of isolated pathogens. [13]. The other causative pathogens isolated in this study were similar to those organisms associated with complicated UTI in general. Compared with the study carried out in Turkey Bioform producer microorganisms such as Escherichia coli, Pseudomonas aeruginosa, Klesiella pneumonia, Proteus mirabilis, were significant cause of CAUTI among catheterized patients. [11]. Compared to a study carried out in Greece where the most frequently isolated pathogen was Candida (55,5%) following by A. baumannii (16.7%) and P. aeruginosa (16.7%), this was similar to this study regarding candida as the most common isolated organism from urine culture. [14]. In Europe, the mean incidence of urinary tract infections in intensive care units is 1.1 per 1000 patient-days. Of these cases, catheter-associated urinary tract infections (CAUTI) account for 98%. [15]. Findings in this study were similar to the study done by Sandhu in India, where they found that, Candida spp. Was isolated from 7patients (41.18%), E. coli 7 (41.18%), K. pneumoniae 1 (5.88%), Citrobacter freundii 1 (5.88%), and S. aureus 1 (5.88%). [16]. In a recent investigation of CAUTIs in nursing home residents, carried out by Brauer et al. and his colleagues, they found that, Proteus mirabilis, Enterococcus species, and Escherichia coli as the three most common organisms causing CAUTI [17].
5. Conclusions
- CAUTI was most common in patients admitted in wards than ICU. CAUTI was more common in females. Approximately one third of patients had CAUTI. Majority of patients had no urinary symptoms. Candida yeast was the most common isolated microorganism among patients with CAUTI, followed by uropathogenic Escherichia coli (UPEC) biofilms.
6. Recommendations
- Avoidance of inappropriate indications for catheter placement; Good catheter management; To have catheter devices with antimicrobial properties; Reducing the duration of catheterization in order to reduce the incidence of CAUTI; Education program for all healthcare workers about hazards of use of urinary catheter in hospitalized patients for inappropriate reasons; Development of protocols and checklists on the insertion and management of indwelling urinary catheters based on the UTI prevention guidelines.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML