-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2019; 8(2): 23-24
doi:10.5923/j.ijim.20190802.02

Dubin Johnson Syndrome with Transaminitis: A Rare Biochemical Variant
Mehak Trikha 1, Dinesh C. Gupta 2
1Dr. D Y Patil Hospital & College, Nerul, Navi Mumbai, Maharshtra, India
2Professor, General Medicine, D Y Patil Hospital & College, Nerul, Navi Mumbai, Maharshtra, India
Correspondence to: Mehak Trikha , Dr. D Y Patil Hospital & College, Nerul, Navi Mumbai, Maharshtra, India.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Dubin Johnson syndrome (DJS) is an autosomal recessive disorder of bilirubin metabolism. It is a very rare diseases and is characterized by persistent and fluctuating jaundice. Jaundice is aggravated by stress, pregnancy, alcoholism, infections, etc. It can be mistaken for viral hepatitis. It carries an excellent prognosis with no adverse impact on life expectancy. Its early diagnosis will help in preventing undue exposure of procedures and treatment to the patients. Here we report a case of DJS which has very occurrence.
Keywords: Dubin Johnson syndrome, Bilirubin, Jaundice
Cite this paper: Mehak Trikha , Dinesh C. Gupta , Dubin Johnson Syndrome with Transaminitis: A Rare Biochemical Variant, International Journal of Internal Medicine, Vol. 8 No. 2, 2019, pp. 23-24. doi: 10.5923/j.ijim.20190802.02.
1. Introduction
- Dubin- Johnson syndrome (DJS) is defined as benevolent, reverting, genetic diseases of bilirubin metabolism. It follows autosomal recessive pattern of inheritance. [1] Biochemically, DJS manifests as abnormalities in coproporphyrin clearance, increased serum bilirubin (conjugated type), coupled with normal level of serum transaminase. The gross appearance of liver is blackish in color due to pigment accumulation. [2] It mostly affects patients in the 2nd or 3rd decade of life. Clinically, it is characterized by recurrent jaundice which is varying intensity and nearly 33% of the patients give a positive family history of similar type of jaundice in first degree relatives. [3] The prevalence of DJS is very low. Liver function tests are normal in most of the cases of DJS. Occasionally, increased direct hyperbilirubinemia can be encountered in some cases. [2] This hyperbilirubinemia can be precipitated by sue of oral contraceptives, pregnancy, any systemic illness, etc. [4] Majority of the reported cases of DJS have been associated normal liver enzymes. We report a rare case of DJS with elevated liver transaminase.
2. Case Report
- A 26 year old male came to our Out Patient Department (OPD) with chief complaints of persistent fluctuating jaundice and abdominal pain since 1-2 months. He gave history of similar pattern of jaundice since childhood. None of these episodes of jaundice had any deleterious effects, though. Abdominal pain was mild, vague and localized to right upper quadrant. The patient was feeling exhausted. No itching was present. His urine was dark yellow in color. His stools were normal in consistency and color. He gave no history of alcohol intake, or intake of any hepatotoxic drug in the recent past.His blood tests showed increased total bilirubin of 11.2 mg/dl and direct bilirubin of 7.5 mg/dl. His serum transaminases levels were raised (70 IU/L). Other serological tests were within normal limits. After follow-up, abdominal pain had subsided, but jaundice still persisted. On examining previous medical records, his bilirubin has been found to be fluctuating in between the range of 7.8-12.4 mg/dl. Viral markers were negative and other causes of jaundice were ruled out.Few days prior to his current visit to our OPD, patient had undergone a liver biopsy. It showed intact lobules structure and blood vessels. However, hepatocytes were heavily laden with brown-black pigment, which stained positively with Masson-Fontana stain and negative with other stains. This was specifically more in the area of portal tracts around the venules, with some amount of intrusion of lymphocytes. No significant fibrosis was found. (figure 1) All the above findings were consistent with clinical diagnosis of DJS.
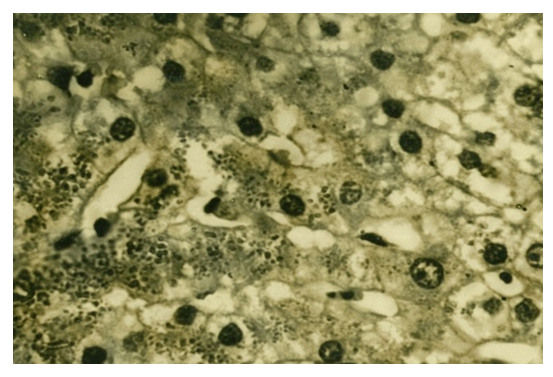 | Figure 1. Liver biopsy showing hepatocytes heavily laden with brown-black pigment |
3. Discussion
- DJS is a very rare disease. [4] The only consistent clinical and biochemical feature of DJS is presence of persistent jaundice which is of waxing and waning intensity. Frequently, this jaundice is aggravated by stress, surgery, pregnancy, alcoholism, infection, etc. [5,6] However, no such triggering factor was found in this particular case. Sometimes, associated clinical features like abdominal pain in hepatic area, nausea, etc. may lead to misdiagnosis of viral hepatitis. [3] Most common complication of DJS in jaundice and hepatomegaly in some cases. In half of the patients, prothrombin time is reduced as a result of deficiency of clotting factor VII. Gallstones and bile duct stones have been reported in some case reports in patients of DJS. [7]Diagnosis is mainly based on clinical, biochemical and liver biopsy findings. In biochemical findings, the only significant finding is conjugated hyperbilirubinemia with normal liver enzymes (fluctuating course with initial rise). [8] Hence, the most interesting feature of the present case was the presence of persistent mildly elevated serum transaminase, and this is suggestive of varying degree of hepatocellular damage. Although, rise in transaminase of such intensity can be seen in binge alcohol intake, obesity, diabetes, etc., all these factors were ruled out in the present case. It is noteworthy to mention that such mild to moderate increase in liver enzymes may be increased without evidence of hepatocellular damage on liver biopsy. Liver biopsy shows hepatocytes laden with brown-black pigment, which gives characteristic blackish appearance to liver, on gross examination. [9]The biochemical confirmatory test for DJS is urinary measurement of type of coproporphyrin. Type III coproporphyrin in normal human urine is replaced by type I variety in urine of patients of DJS. [10,11] No treatment is available for DJS, nor is it required, as DJS carries an excellent prognosis with normal life expectancy. [12]
4. Conclusions
- Dubin Johnson syndrome is very rare in occurrence. Since has excellent prognosis and a benign course, early diagnosis through a clinical suspicion in cases of persistent jaundice since childhood with normal to mildly elevated liver enzymes will prevent undue exposure to battery of tests and procedures on the patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML