-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2019; 8(2): 17-22
doi:10.5923/j.ijim.20190802.01

Acute Exacerbations of COPD; A One Year Hospital-Based Study, Egypt
1Internal Medicine Department, Al-Azhar University, Cairo, Egypt
2Lecturer of Chest Diseases Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
Correspondence to: Hend Kotb, Internal Medicine Department, Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: acute exacerbations are frequent during the course of chronic obstructive pulmonary disease (COPD). They are associated with increased morbidity and mortality. The aim of the study: is to characterize the patients who are hospitalized for acute exacerbation of COPD and the factors related to frequent hospitalization. Patients and Methods: observational cohort study. One hundred and one patients admitted to our hospital for acute exacerbation of COPD over one year (group I) and equal number of patients with mild COPD exacerbation not requiring hospital admission (groupII) were studied. Results: We found that 101 patients admitted with acute exacerbation of COPD accounted for 10% of all admissions to medical departments and 2% of all admissions to our hospital. Group I patients had more advanced disease, high frequency of current smoking and comorbidities, frequent use of systemic steroids and home oxygen therapy. They had significant leukocytosis with neutrophilia, and higher partial pressure of carbon dioxide in arterial blood (paCO2). Significantly lower partial pressure of oxygen in arterial blood (PaO2), low 6-minute walking distance (6MWD) and more advanced COPD assessment test (CAT) score and BODE index. Severity of acute exacerbation of COPD, hypercapnia, previous ICU admission, low body mass index (BMI), low (6MWD), low PaO2, and the presence of comorbidities are the factors associated with increased frequency of hospital admission. Conclusion: COPD patients who had severe acute exacerbation, comorbidities, hypoxemia, hypercapnia, history of previous admission to ICU, low BMI, and impaired physical activity are more likely to be admitted to hospital during acute exacerbation of COPD.
Keywords: Chronic obstructive pulmonary disease, Exacerbation, Acute exacerbations of COPD, re-admission
Cite this paper: Hend Kotb, Eman Sobh, Acute Exacerbations of COPD; A One Year Hospital-Based Study, Egypt, International Journal of Internal Medicine, Vol. 8 No. 2, 2019, pp. 17-22. doi: 10.5923/j.ijim.20190802.01.
Article Outline
1. Introduction
- Chronic obstructive pulmonary disease (COPD) is one of the leading causes of death worldwide [1]. Acute exacerbations are frequent events during COPD course. Acute exacerbations are the major risk of disability and mortality. About 10% of COPD cases experience in-hospital mortality [2].Acute exacerbations of COPD are defined as acute onset events associated with a change in day to day symptoms of the disease with an increase in at least two of patient’s baseline symptoms (dyspnea, cough and sputum purulence), demanding modification of regular treatment and may require admission to the hospital [3].A common classification of the severity of an acute exacerbation include: Mild: the patient suffers an increased need for medication that can be managed at home. Moderate: sustained deterioration of respiratory condition that mandates treatment with systemic corticosteroids plus/or antibiotics. Severe: rapid worsening of respiratory condition that needs admission to hospital [4].There is a lack of literature reporting epidemiology, and behavior of COPD in Egypt and factors related to their hospital admission. The aim of this study was to assess the frequency of hospital admissions related to acute exacerbations of COPD and hence the characteristics of hospitalized patients and the factors related to readmission in a cohort of patients at our hospital within 1-year.
2. Patients and Methods
- Between January and December 2017, 202 patients with a primary diagnosis of acute exacerbation of COPD were included in this observational cohort study at Al-Zahraa University Hospital, Cairo, Egypt. The diagnosis of COPD was established based on medical history, current symptoms of cough, dyspnea or sputum production and available standard spirometry. The severity of COPD was assessed according to The Global Initiative for Chronic Obstructive Lung Disease (GOLD) classifications [post-bronchodilator FEV 1 /FVC < 70%, FEV 1 reversibility <12%), FEV1%] [3]. They were divided into two groups. Group I: included one hundred and one patients who had been consecutively admitted with sever acute exacerbation of COPD, Group II: included one hundred and one patients with mild acute exacerbation of COPD treated as outpatients without hospitalization during the study period. After history taking and physical examination, all patients completed the Arabic version of COPD Assessment Test (CAT) respiratory questionnaire [5]. The total CAT score was calculated for each individual by adding the score for each item. The scoring range of CAT starts from zero to 40. It was divided into four groups of low, medium, high and very high depends on the negative effect of disease on the general condition.BODE index: calculated for each patient according to the combination of four variables, with the following scores: calculation of body mass index (BMI) from 0 to 1 point; calculation of the intensity of airflow obstruction (FEV1% predicted post bronchodilator): from 0 to 3 points; calculation of subjective sensation of dyspnea (modified Medical Research Council scale; mMRC): from 0 to 3 points; and calculation of exercise tolerance (six minute walking distance; 6MWT): from 0 to 3 points. The net score of the BODE index ranges from 0 to 10 points; the higher the index score, the worse is the patient’s situation. [6]We recorded demographic data, history and clinical examination including signs and symptoms of COPD, associated comorbidities [hypertension (HTN), diabetes mellitus (DM), heart disease (HD), chronic liver disease, asthma, bronchiectasis, hepatitis C virus (HCV) positive, lung cancer, and chronic kidney disease (CKD)], criteria for acute exacerbations of COPD. Baseline spirometry data, 6-minute walking distance, arterial blood gases, and complete blood count (CBC), and treatment at first admission. Also we recorded length of hospital stay, ICU admission, number of hospital readmissions throughout the year for acute exacerbations of COPD. Patients who were admitted less than 2 days or with incomplete data were excluded from the study. All procedures performed in the study were in accordance with the ethical standards of the Faculty of Medicine for Girls, Al-Azhar university research committee and the Helsinki declaration and its later amendments ethical standards.
3. Statistical Analysis
- All analyses were performed using the Statistical Package for the Social Science (SPSS) program version 15 (Inc, Chicago, Illinois, USA). Data are described as mean (±standard deviation) and number (percentage). The χ2 test and the Student’s t-test were used for qualitative and quantitative data respectively. The significance level was taken at p≤0.05.
4. Results
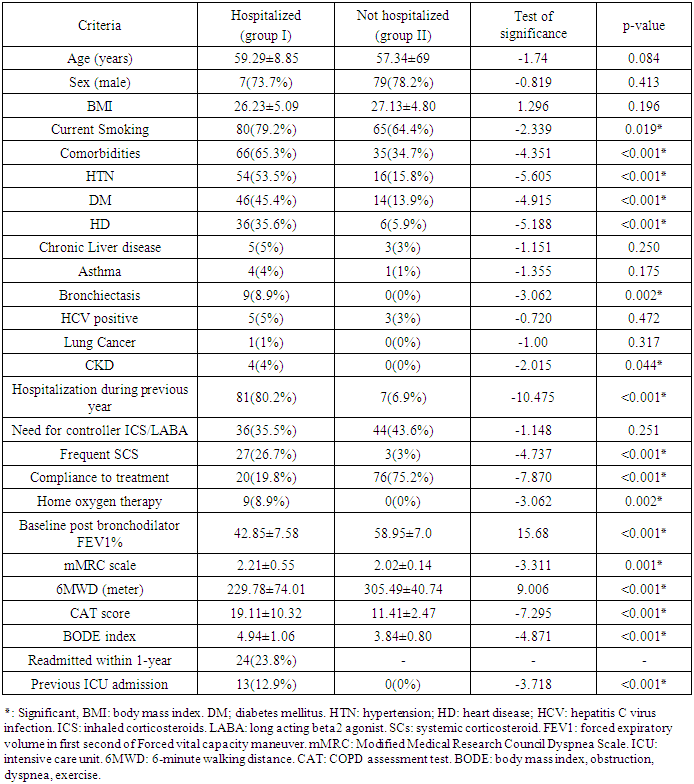
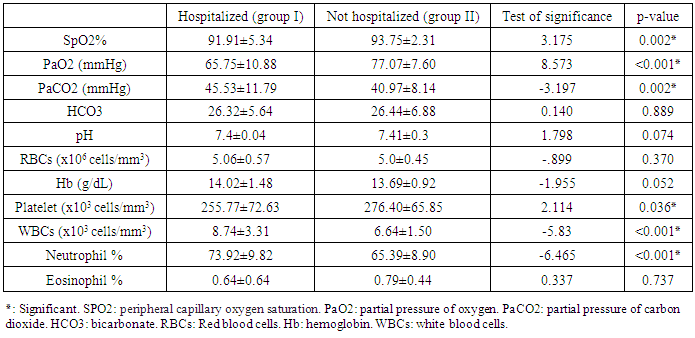
- The total admissions related to acute exacerbation of COPD were 179 times in the period of study accounting for 10 % of all admissions to medical departments and 2% of all admissions to our hospital. Twenty-four (23.8%) patients among group I patients experienced re-admission within the study year. No significant difference was observed among both groups regarding age, sex and body mass index (BMI). Group I patients were mostly smokers compared to group II (80 (79.2%) vs 65 (64.4%) (P= 0.019). Comparison of presence of comorbidities (HTN, DM, HD, chronic liver disease, asthma, bronchiectasis, HCV positive, lung cancer, and CKD), actual hospitalization during previous year and previous ICU admission between both groups revealed significant difference being more prevalent among group I. Comparison of frequent use of systemic corticosteroids (SCS), home oxygen therapy between both groups revealed significant difference being higher in group I (p< 0.001). Both groups did not differ in the need for controller inhaled steroids/Long acting beta 2 agonist (ICS/LABA). Group I patients were less compliant to treatment (20 (19.8%) vs 76 (75.2%)) (P<0.001). Group 1 patients had significantly more airflow obstruction compared to group II (Baseline post bronchodilator FEV1%= 42.85 ±7.58 vs 58.95 ±7.0) (P<0.001), had clear functional exercise intolerance (6MWD =229.78±74.01 vs 305.49±40.74 m) (P<0.001), BODE index score (P<0.001), mMRC score (P= 0.001), and CAT score were found to be significantly higher in group I patients compared to group II (P<0.001) (Table 1).
|
|
|
5. Discussion
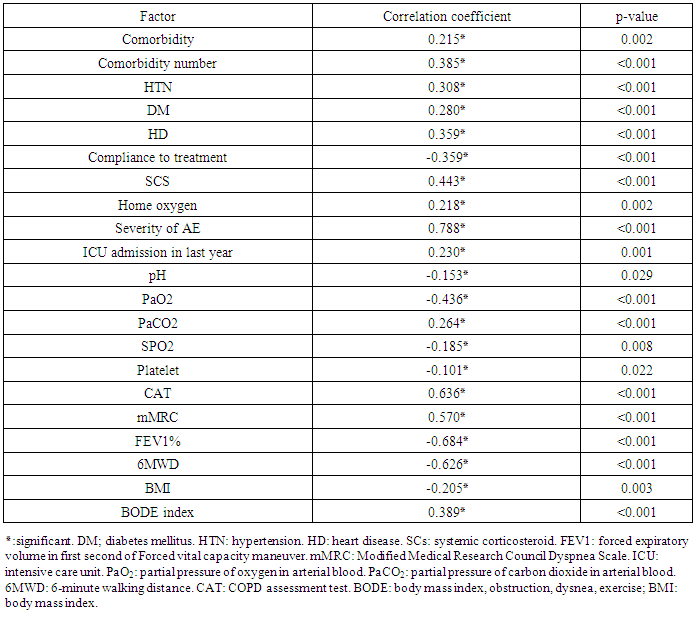
- There are 101 patients admitted respectively for acute exacerbation of COPD during the period of follow-up, 23.8% of them had recurrent hospitalization within the study year and 12.9% of them reported ICU admission and hospital admission during the previous year.The same results were reported in previous studies; Badaran et al 2012 study [7] found 18.8% of COPD patients were readmitted within a year while, ECLIPSE study reported about 15% of COPD patients reported multiple admissions [8] and among hospitalized patients with acute exacerbation of COPD (47%) had more than one exacerbation episode required hospitalization for COPD exacerbation during the first 12 months follow-up.Our study showed that mean age was (59.29±8.85 & 57.34±69) for hospitalized patients and patients treated without hospitalization respectively and men represent the majority of patients in both groups due to more prevalence of smoking in males in Egypt [9], there was no significant difference in gender or age between those who were hospitalized and those who were treated in outpatient clinic, 79.2% of the hospitalized group are currently smokers. Similar results were previously described by Badaran et al, 2012 [7] who reported 91.8% men and incidence of smokers was 26.5%. Smoking was reported to be the most common factor associated with COPD exacerbations in their study.Comorbidities have an impact on exacerbations of COPD [10] and some studies showed that the increased systemic inflammation during COPD exacerbations, high oxidative stress, plasma fibrinogen, and serum IL-6 levels [11, 12], can increase comorbidities [10].In our study; the number of comorbidities was significantly higher in hospitalized patients. Among comorbidities; hypertension, diabetes mellitus, coronary heart disease, chronic kidney disease and bronchiectasis were significantly more detected in the hospitalized group. Comorbidities are reported to be associated with frequent hospitalization [7, 8]. Comorbidities are frequent in COPD and current smoking is the most common risk factor for most of them. Comorbidities are associated with recurrent hospitalization and increased morbidity and mortality [10]. In this study there are statistical difference between group I , and group II as regard to frequency of vascular and heart disease being more prevalent in group I (P value < 0.001), these were in agreement with many studies, they reported that vascular and heart disease are the most frequent comorbidity among patients with frequent readmission [7, 8, 10]. The increased coronary risk in patients with COPD may be due to the systemic inflammatory reaction [13]. The presence of COPD could contribute to the development of cardiovascular disease through hypoxia, systemic inflammation and oxidative stress [14], smoking is a common risk factor for both COPD and coronary artery disease [10]. The increased peripheral leucocytes and neutrophil counts in the studied patients support the occurrence of systemic inflammation [10]. High neutrophil count in peripheral blood was detected in bacterial exacerbations [15]. Some studies detected a significant relationship between neutrophilia in peripheral blood, exacerbation severity and frequency of hospitalization in COPD exacerbations [16, 17].We also found that those who were hospitalized had significantly lower FEV1% and 6-minute walking distance, higher CAT score, BODE index, Lower oxygen saturation, PaO2, higher PaCO2. They also had a higher frequency of systemic steroids use, need for controller ICS/LABA, home oxygen and lower compliance to therapy.García-Sanz and his colleagues 2012 [16] reported higher frequancy of the history of prior exacerbations, COPD disease severity, use of concomitant medications such as inhaled and systemic corticosteroids, beta-blockers and antibiotics among hospitalized compared to non-hospitalized patients.Alahmari and his colleagues 2016 [18] reported that exacerbations are associated with decreased physical activity and exercise intolerance. Various contributors to muscle weakness at exacerbation have been hypothesized, including immobility, treatment with corticosteroids, nutritional deficit, oxidative stress and inflammation [19].In our study we found that frequency of hospitalization correlated positively with the presence & number of comorbidities, type of comorbidity (DM, HTN, HD), previous ICU admission, use of SCS, severity of exacerbation, CAT score, mMRC dyspnea score, BODE index, PaCo2, WBCs, and negatively with compliance to treatment, pH, PaO2, oxygen saturation, BMI, FEV1% and 6MWD. Similar results were reported in previous studies [16, 20]. Patel and his colleagues 2015 [20] reported that patients hospitalized with COPD exacerbation had a high rate of readmission within the following year, while García-Sanz his colleagues 2012 [16] reported that the factors associated with hospitalization were impaired oxygenation, increased white blood cell count and prescribed antibiotics. Frequent exacerbations were associated with greater impairment in health status and exacerbations become more frequent and more severe as the severity of underlying COPD increases and the most important determinant of frequent exacerbations is a history of exacerbations [21]. Müllerova and his colleagues 2015 reported that the strongest risk factor for future hospitalized exacerbation was a history of hospitalized exacerbations in the 12 months prior to their study; Other significant risk factors included poorer health status, severe airflow limitation, older age, a higher degree of emphysema, and an increased WBC count [8].
6. Conclusions
- Severe acute exacerbation, hypercapnia, previous ICU admission, low BMI, low 6- MWD, hypoxemia, and the presence of comorbidities were the factors affecting frequent hospital readmission. Efforts should be directed to improve health status, and early detection of patients with COPD who had risk factors for repeated readmission. Rehabilitation should be included in the management plan of those patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML