-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2019; 8(1): 1-5
doi:10.5923/j.ijim.20190801.01

The Impact of Nutritional Status on Patients with Pneumonia: A Retrospective Study
Sami Giryes1, Tanya Mashiach2, Jesse Lachter3, Ayelet Raz-Pasteur4, Amir Karban5, Irit Chermesh3
1Internal Medicine Department B, Rambam Health Care Campus, Haifa, Israel
2Department of Quality Control, Rambam Health Care Campus, Haifa, Israel
3Gastroenterology Department, Rambam Health Care Campus, Haifa, Israel
4Internal Medicine A, Rambam Health Care Campus, Haifa, Israel
5Internal Medicine C, Rambam Health Care Campus, Haifa, Israel
Correspondence to: Sami Giryes, Internal Medicine Department B, Rambam Health Care Campus, Haifa, Israel.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Malnutrition risk is elevated amongst patients hospitalized with pneumonia; it's relevance to patient outcome has not been fully determined. The Malnutrition Universal Screening Tool (MUST) is a well validated tool for malnutrition screening in hospitalized patients. Objectives: To assess whether malnutrition is an independent risk factor associated with mortality. Methods: The study included all patients during 2008-2011, who were hospitalized in internal medicine departments because of pneumonia and underwent screening by MUST. Data were retrieved from electronic medical records and included: MUST score, Charlson Co-Morbidity (CCI) score, in-hospital mortality and five-year mortality. Results: The trial enrolled 507 patients; 219 (43%) females, mean age of 71.4 +/-17.3 years, 34.91% at risk for malnutrition. The bivariate analysis in hospital mortality was 3.38 times (CI 2-5.73, p<0.001) higher in patients with a MUST score of 2 or more than in patients with a MUST score of less than 2 (23.2% vs. 8.2% respectively). In-hospital mortality was significantly higher in patients older than 70 years of age, with a higher CCI and lower albumin levels. On multivariate analysis: age, high MUST, CCI, and low albumin were found to be significantly associated with higher mortality rates. Patients with a MUST score of 2 or more and a CCI of 1 or 2 had significantly higher five years mortality rates (p < 0.001). Conclusions: Pneumonia patients at risk for malnutrition had higher in- hospital and five years mortality rates than patients not at increased risk for malnutrition.
Keywords: Pneumonia, Mortality, Nutrition, Malnutrition, Co-morbidity, MUST
Cite this paper: Sami Giryes, Tanya Mashiach, Jesse Lachter, Ayelet Raz-Pasteur, Amir Karban, Irit Chermesh, The Impact of Nutritional Status on Patients with Pneumonia: A Retrospective Study, International Journal of Internal Medicine, Vol. 8 No. 1, 2019, pp. 1-5. doi: 10.5923/j.ijim.20190801.01.
Article Outline
1. Introduction
- Malnutrition among hospitalized patients is a global issue of major importance.The prevalence of inpatient malnutrition has been estimated to be as high as 50% among acutely hospitalized adults, depending on the definition employed and the population assessed [1-4]. Malnutrition risk is elevated amongst patients hospitalized with pneumonia [4].The Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition pointed out that malnutrition is to be suspected if two or more of the following criteria are met: insufficient energy intake, weight loss, loss of muscle mass, loss of subcutaneous fat, localized or generalized fluid accumulation and diminished functional status as measured by hand grip strength [5].The inflammatory nature of pneumonia may cause Disease-Related Malnutrition (DRM) [6]. DRM is characterized by catabolism, tissue breakdown and anorexia; all resulting in reduced Fat Free Muscle Mass (FFMM) and a decline in function capabilities. Consequences of malnutrition have long been acknowledged; adverse outcomes such as prolonged hospitalization, increases of morbidity and mortality as well as higher hospitalization costs are all associated with malnutrition at the time of hospitalization, and with poor food intake during hospitalization [7-12]. Several nutrition screening tools have been validated and are therefore recommended for use in caring for all hospitalized patients; These include the Malnutrition Universal Screening Tool (MUST), Mini Nutritional Assessment (MNA) and Nutrition risk screening 2002 (NRS 2002) [12].The MUST is recommended for use by the European Society for Clinical Nutrition and Metabolism (ESPEN), the National Institute of Clinical Excellence (NICE), the British Association for Parental and Enteral and Nutrition (BAPEN) and the British Dietitian Association (BDA) [12-14].This tool is easy to use, well validated, and advocated for use in hospitalized patients [12, 15-16].The parameters of the MUST are: Body mass index (BMI), unintended weight loss during the 3-6 months before the day on which screening is carried out, the effect of acute disease on the patient, and the extent to which the patient's nutritional needs are met during the five days following admission. Each parameter is scored 0-2, thereafter the scores are summed. If the sum ≥ 2 the patient is defined as at high risk for malnutrition [16]. A thorough nutritional assessment and nutritional treatment plan is advocated for patients with a MUST score ≥ 2. Nutrition screening using MUST is performed routinely at our medical centre by trained qualified nurses on admission to the hospital, and is recorded on every patient's electronic medical record. Previous studies correlated the MUST score with poor clinical outcomes, prolonged hospitalization, increased mortality, and higher costs [14, 17-19]. An important conceptual issue is whether malnutrition is an independent factor, or rather one that accompanies the patient's general condition. The patient’s general condition is influenced by co morbidities. The Charlson co-morbidity index (CCI) is a tool used to predict mortality based on the presence or absence of co morbidities; the higher the CCI, the more severe the background diseases [20]. In this study, the MUST was used to screen patients for malnutrition and the CCI to assess the severity of co-morbidities. The aim of the research was to test whether patients diagnosed with pneumonia and at increased risk for malnutrition are at increased risk for mortality, when compared to patients hospitalized with pneumonia who were not found to be at increased risk for malnutrition. The authors hypothesized that malnutrition is an independent risk factor associated with mortality.
2. Material and Methods
- This retrospective study was carried out at Rambam Health Care Campus, a tertiary hospital in Northern Israel. The study period was three years, starting in 2008. All adult patients (age > 18) hospitalized in internal medicine departments during the study period, who had been diagnosed as suffering from pneumonia and undergone screening for malnutrition using the MUST on admission to the department, were included in this study. Diagnosis of pneumonia relied on one of the following criteria: pneumonia as the primary diagnosis on admission to the hospital, and/or recorded in the release letter from the hospital, and/or a primary diagnosis compatible with symptomatology of pneumonia as the primary diagnosis on admission, and pneumonia as the primary diagnosis on the release letter from the hospital. Excluded from the study were patients suffering from malignancy. Approval was obtained from the hospital's institutional review board (IRB).
2.1. Data Collection
- Data was retrieved from the electronic medical records. The data included: age, gender, MUST score, albumin, co- morbidities, hospital mortality, and five-year mortality for patients released alive from the index hospitalization. The Charlson Co-Morbidity index was calculated using the above data.
2.2. Statistical Analysis
- A bivariate analysis of association between patient characteristics and prevalence of malnutrition risk, as identified with MUST with in-hospital mortality, was performed using bivariate logistic regression. An assessment of predictors of the mortality rates was performed using multivariate stepwise logistic regression. The area under receiver operating characteristics (ROC) was used as a measure of model discrimination. The ROC curve plots the estimated sensitivity and the specificity of the prediction of mortality with the actual mortality, where a higher ROC better predicts the mortality rate. Calculation of the ROC was performed with and without the MUST score to evaluate the importance of the MUST regarding mortality estimation. A Kaplan-Meier analysis with log rank test was performed to estimate survival by CCI groups with inpatients, with and without risk for malnutrition.Two-tailed p values of 0.05 or less were considered statistically significant. All statistical analyses were performed with SPSS version 21 for Windows. The statistical analysis was performed by a biomedical statistician.
3. Results
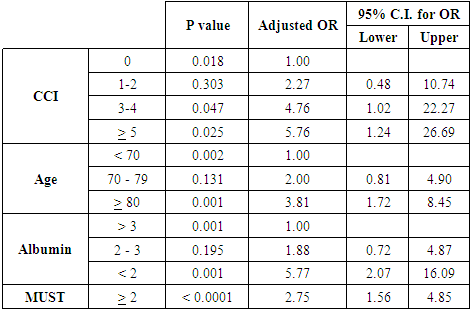
- The number of patients hospitalized with pneumonia and screened by MUST during the study period was 507; 219 were females, mean age was 71.4 +/- 17.3 years; 179 patients were younger than 70 years old, 141 patients were between 70-79 years old, and 187 were 80 years or older. One hundred seventy-seven (34.91%) patients were identified as being at high risk for malnutrition with a MUST score of 2 or more; 80 patients had a CCI of 0, 158 patients a CCI of 1-2, 136 patients a CCI of 3-4, and 133 patients a CCI of 5 or more. Of the patients with a MUST score of 2 or more; 22.5% had a CCI of 0, 39.9% a CCI 1-2, 32.4% a CCI of 3-4 and 39.1% a CCI of 5 or more. The in-hospital mortality rate was 13.4% (68). On bivariate analysis, in-hospital mortality was significantly higher in patients older than 70 years of age, and with a MUST score of 2 or more, a higher CCI and lower albumin levels. Mortality was 3.38 times (CI 2-5.73; p<0.001) higher in patients with a MUST score of 2 or more than in patients with a MUST score less than 2 (23.2% vs. 8.2% respectively). Mortality for patients older than 70 years of age was higher than for patients younger than 70 (OR 2.59 CI 1.12-6 p<0.05; OR 5.47 CI 2.58-11.62 p<0.001 for patients aged 70-79 and patients aged 80 or more respectively). Albumin levels of less than 30 g/L were associated with higher mortality (OR 2.98 CI 1.2-7.41 p=0.02; OR 8.74 CI 3.29-23.25 p<0.001 for patients with an albumin level of 20-30 g/L and <20 g/L respectively). The higher the CCI the higher the mortality rates, with the difference reaching statistical significance for patients with a CCI of 3 or more compared to a CCI of 0.On multivariate analysis: a MUST score of 2 or more; age, high CCI and low albumin were found to be significantly associated with higher mortality rates. Table 1 presents the results of the multivariate analysis. In hospital mortality rates in patients with a MUST score of 2 or more were higher than in patients with a MUST score of less than 2 (OR = 2.75, CI 1.56-4.85; p < 0.0001). The model is illustrated in Fig. 1.
|
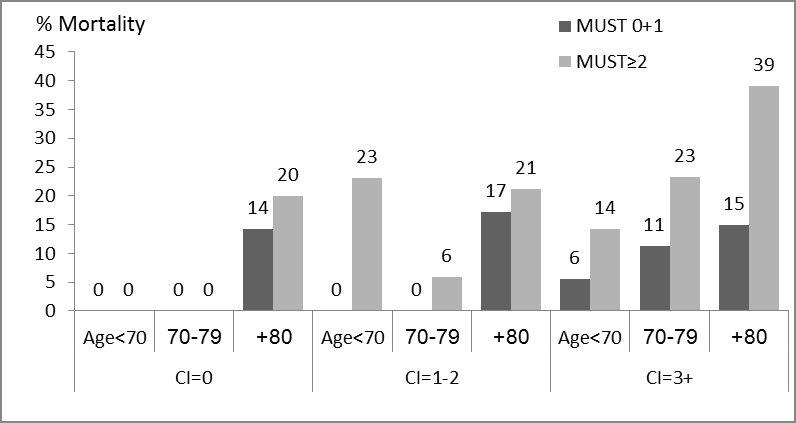 | Figure 1. In-hospital mortality stratified by age and CCI of patients with MUST score of ≥ 2 and MUST score < 2 |
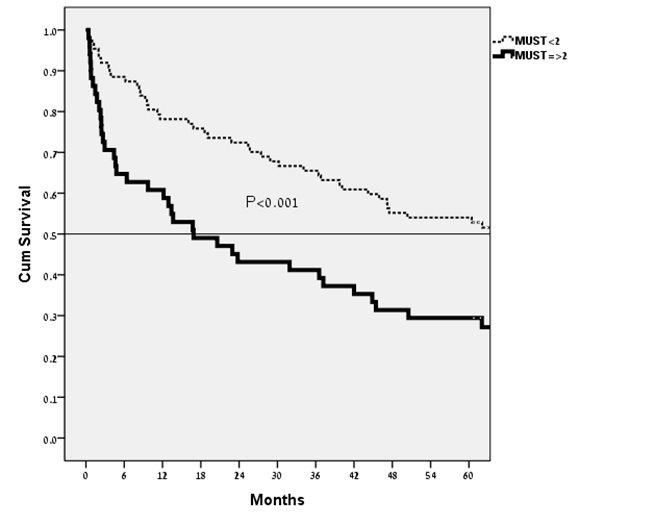 | Figure 2. Kaplan-Meier survival curve of patients with a MUST score of < 2 and a MUST score of ≥ 2, with a CCI of 1 or 2 |
4. Discussion
- The association of nutritional status and infections is bidirectional; malnourished patients are more prone to having severe infections due to impaired immunity [21]. Specifically, regarding pneumonia, malnutrition causes decline of muscle mass with ensuing weakness, which can lead to inability to cough efficiently, aspiration pneumonia, and difficulty in recovering from pneumonia. Conversely, the inflammatory catabolic nature of pneumonia along with its tendency to cause loss of appetite worsens the nutritional state.It is highly important that the severity of pneumonia and the probability of mortality of a patient suffering from pneumonia be assessed. Various tools were developed to assess the level of risk for pneumonia patients; however, these tools do not take into account the nutritional status of the patient. An example of this is the pneumonia severity index (PSI) developed by the Pneumonia Patient Outcomes Research Team (PORT) [22, 23]. The PSI includes 20 demographic and clinical variables, none of which directly reflect the nutritional status of the patients.Results of the study herein presented are that screening by MUST identifies patients suffering from pneumonia with a high risk for in-hospital mortality independent of age, albumin levels, and co-morbidities as reflected by the CCI. The MUST significantly add to the prediction ability as depicted by the ROC, with and without the MUST.The high mortality of patients with a high MUST score persists during the five years following the index hospitalization and is significantly greater for patients with a CCI of one or two. The absence of significance for five-year mortality for patients in the lowest and highest CCI groups might reflect the fact that patients belonging to the lowest CCI group are robust individuals and their measured risk of malnutrition is more directly connected with their current illness. Once they overcome pneumonia, their risk for mortality is not different from other patients that belong to the lowest CCI group. With regards to the patients that belong to the highest CCI group - the opposite is true. These are ill frail individuals for whom primary cause of death would be their co-morbidities and complications of these; therefore, malnutrition plays a relatively lesser role after recovery from the index pneumonia.A large study by Deutz et al. included 652 hospitalized patients at high risk for malnutrition who were assigned randomly to treatment by protocol with special artificial nutrition or a placebo [24]. All patients underwent assessment by a dietician and received additional treatment as recommended. The treatment group had a significantly lower mortality rate than the placebo group (4.8% vs. 9.7% respectively). Taking into account the study by Deutz et al. and the known data regarding malnutrition and pneumonia, nutritional treatment by protocol should be considered based on the screening results.The MUST is a low-cost screening tool easily accomplished by the nursing staff, requiring barely two minutes, which can serve as a life-saver, in addition to being a valuable research tool. Screening patients for malnutrition on admission is highly recommended. We recommend that patients who are found to be at high risk for malnutrition be favourably considered for supplemental nutritional treatment using a defined protocol along with a complete nutritional assessment and specific nutritional treatment.The study limitations are its retrospective design, not all patients underwent screening for malnutrition, different comorbidities were taken into consideration by calculating CCI for each patient without to check each comorbidity alone, and the fact that the patients could not be stratified by the severity of their pneumonia. All of the patients included are hospitalized patients, therefore, taking into consideration the criteria for hospitalization, they are considered to be high risk patients. The strength of this study is the large number of patients with accurate data recorded for multiple variables.
5. Conclusions
- Patients with pneumonia identified at high risk for malnutrition have a higher rate of mortality compared to patients who not at high risk. Early recognition of high-risk patients is a critical step for development of comprehensive care which should include nutritional treatment. Nutritional care may ameliorate the devastating results of the pneumonia – malnutrition viscous cycle.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML