-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2018; 7(4): 54-59
doi:10.5923/j.ijim.20180704.02

Prevalence of Malnutrition among Hospitalized Medical Intensive Care Unit Patients in a University Hospital, Cairo, Egypt: Hospital Based Survey
Doaa S. D. Zaki1, Doaa M. Zakaria1, Heba M. Abd El-Galil2
1Department of Internal Medicine, Al-Zahraa University Hospital, Al-Azhar University, Cairo, Egypt
2Department of Community Medicine and Occupational Health, Al-Azhar University, Cairo, Egypt
Correspondence to: Doaa S. D. Zaki, Department of Internal Medicine, Al-Zahraa University Hospital, Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

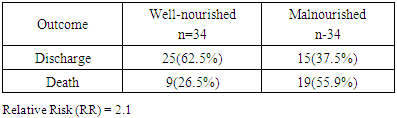
Background/Aims: Malnutrition in critically ill adults in the intensive care unit (ICU) is a serious public health problem that has been associated with a significantly elevated risk of infectious and non-infectious complications. This study aimed to estimate the prevalence of malnutrition among adult patients admitted to medical ICU. Methods: This was a hospital based prospective cross-sectional study carried out for 3 months in medical ICU of the internal medicine ward in AL-Zahra University hospital, Cairo, Egypt. Patients were evaluated for the nutritional status by using subjective global assessment (SGA) within the first 24 hours of admission. Results: A total of 68 patients were participated in the study (61.1±13.3 years; 54.4% females). According to SGA, 50% of ICU patients were malnourished either mild/moderate (35.3%) or severely malnourished (14.7%). Malnourished patients had a mortality rate of (55.9%) versus well-nourished group (26.5%). Conclusions: Malnutrition was highly prevalent among critically ill patients in medical ICU and increased the risk of mortality. Nutritional screening is mandatory in ICU sitting to initiate timely nutritional therapy.
Keywords: Malnutrition, Critical illness, Mortality, ICU
Cite this paper: Doaa S. D. Zaki, Doaa M. Zakaria, Heba M. Abd El-Galil, Prevalence of Malnutrition among Hospitalized Medical Intensive Care Unit Patients in a University Hospital, Cairo, Egypt: Hospital Based Survey, International Journal of Internal Medicine, Vol. 7 No. 4, 2018, pp. 54-59. doi: 10.5923/j.ijim.20180704.02.
Article Outline
1. Introduction
- Malnutrition refers to a state of under-nutrition (due to insufficient intake or impaired utilization), or over-nutrition (from excessive calorie intake and/or inadequate physical activity) of macronutrients elements or specific micronutrient needs, which are critical to tissues [1]. Malnutrition in hospitalized patients within the critical care setting is a global health problem where prevalence is 78.1% and 50.8% in developing and developed countries respectively [2]. It is frequently associated with significant clinical and economic consequences, including increased risk of complications, infections, prolonged hospital stay, poor quality of life and more frequent readmission especially among elderly people [3]. Patients admitted to (ICU) may already present with malnutrition or are at high risk of becoming malnourished [4]. In critically ill patients, systemic inflammatory response to critical illness induces a catabolic state that increases the metabolic demands and accelerates the development of malnutrition [5]. Because of lack of appropriate screening, assessment, and treatment protocols in addition to physicians’ inadequate nutrition training; malnutrition is usually unable to be diagnosed and treated in up to 70% of patients admitted to hospital [6, 7]. Furthermore, about 70–80% of the admitted malnourished patients enter and leave the hospital without receiving any nutritional support and the diagnosis of malnutrition does not appear on their discharge sheet [8]. Identifying malnourished patients on admission to ICU will help in assessing the level of treatment required, anticipating complications, preventing the associated negative clinical outcomes of malnutrition and allocating limited resources where it is most needed. [9, 10]. During critical illness, anthropometric markers such as weight becomes less reliable due to influences of hydration in addition, biochemical markers such as albumin is affected by various factors such as disease severity and inflammation hence it is not a valid indicator of nutritional status [11, 12]. Therefore, there are various screening tools and scoring methods that provide a quick and simple approach to identify malnutrition in the community and hospitals [13].Subjective global assessment (SGA) has been used in a wide variety of health-care settings including critical care units as a well-validated tool for assessment of the nutritional status [2]. To our knowledge, there are no reports for prevalence of malnutrition in the ICU sitting from Egypt. The aim of the present study was to estimate the prevalence of malnutrition in the medical ICU using (SGA) and to determine the value of SGA in predicting mortality in critically ill patients.
2. Patients and Methods
2.1. Study Participants
- This hospital based prospective cross-sectional study was conducted at Al-Zahraa University Hospital, Cairo, Egypt. The ICU of internal medicine ward contains 10 beds and functions as a closed unit that provides support to the medical patients. The study was carried out over a period of three months; from February to April 2018. Patients who had >24 h ICU-length of stay (ICU-LOS) were enrolled in the study and only data obtained at their first ICU admission within the same hospitalization were included in the study. The patients were followed up until they were dismissed from ICU by discharge to the general ward or death.The sample size was calculated by using equation in the Raosoft software package. Considering the prevalence of malnutrition among hospitalized patients 78.1% [2] with accepted margin of error 5% and the confidence level 95% and according to annual flow on internal ICU ward. Informed consents were obtained from all patients or their corresponding relative who agreed to participate in the study. All patients with terminal cancer or re-admitted within the study period were excluded from the study. All procedures were performed in accordance with the guidelines in the Declaration of Helsinki and approved by Research Ethics Committee of Faculty of Medicine for Girls, Al-Azhar University.
2.2. Study Tools
- Eligible patients were subjected to the completion of pre-designed semi structured sheet for patients' demographic data with emphasis on gender, age, marital status, living arrangements, medical history, primary causes of admission, ICU-LOS and clinical outcomes. The nutritional status of studied patients was assessed within 24 hours of admission to the ICU using SGA. It assesses nutrition status of the patient via a questionnaire which includes data on weight change, dietary intake change, gastrointestinal symptoms, changes in functional capacity and comorbidities in relation to malnutrition as well as assessment of fat and muscle stores and the presence of oedema and ascites [14]. The patients were classified according to SGA into: A—well-nourished; B—mildly/moderately malnourished; or C—severely malnourished. Middle upper arm circumference (MUAC) was measured at point on the arm halfway between the acromion and olecranon [15]. Abdominal skin fold (ASF) were measured using Care touch skin fold caliper (Care Touch Medical Equipment Inc., Lakworth, Florida).Biochemical and hematological parameters including hemoglobin (g/L), albumin (g/L), lymphocyte count (× 109/L), calcium (mg/L), cholesterol (mg/dl) were obtained from patient’s chart and recorded for analysis.
2.3. Statistical Analysis
- Data collected was reviewed, coded and statistically analyzed using Statistical Package for the Social Science (SPSS) program version 18 (Inc, Chicago, Illinois, USA). Data was described in terms of mean ± standard deviation (±SD) (for continuous variables) and percentage (for categorical variables). Chi square-test (χ2) was used for the comparison of qualitative data. Student’s T test and one-way analysis of variance (ANOVA) were used to compare between quantitative data with post hoc test for significant results. The Relative Risk (RR) was calculated to determine the risk, or likelihood, of being malnourished and becoming die. Binary logistic regression was carried out to identify some predictors for mortality. Significance level was taken at p value≤ 0.05.
3. Results
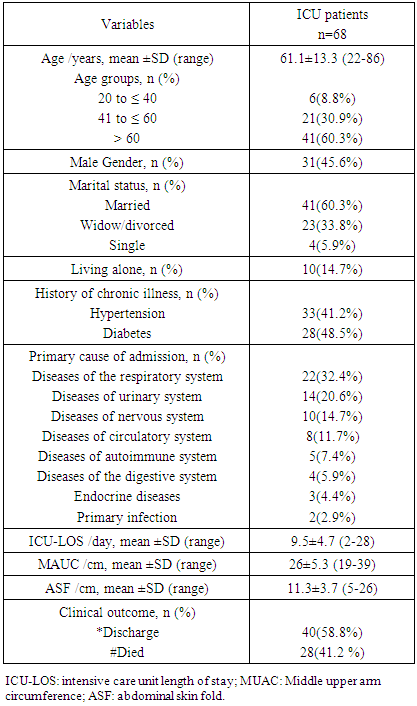
- A total of 68 patients admitted to medical ICU of internal medicine ward during a period of 3 months met the selection criteria. Their age ranged between 22 and 86 years with mean ± SD 61.1 ± 13.3 years; nearly two thirds (60.3%) of them were above 60 years old. Females constituted more than half (54.4%) of them. Majority (85.3%) of patients were living with their family and about (60.3%) married. Most of patients were diagnosed previously with chronic diseases either hypertension or diabetes (41.2% & 48.5% respectively). The most common primary diagnosis of the participants for ICU admission were diseases of the respiratory system (32.4%). The mean duration of stay in ICU was 9.5 ± 4.7 days; ranged from 2 and 28days (Table 1).
|
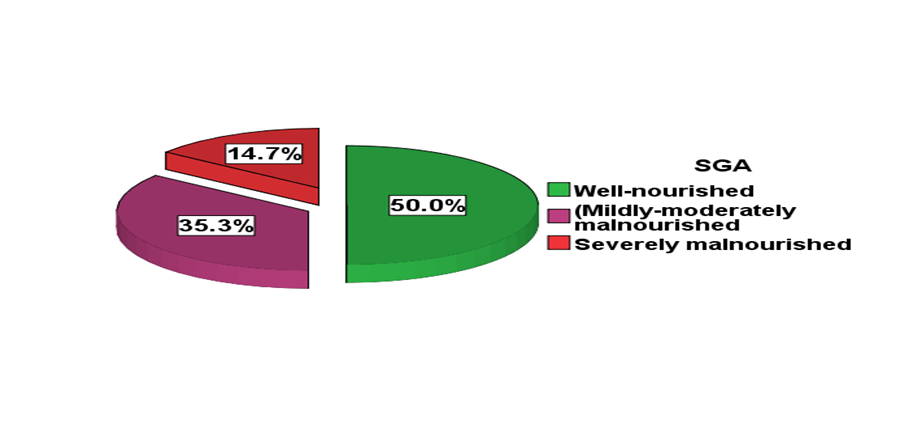 | Figure 1. Nutritional status of the studied medical ICU patients according to SGA |
|
|
|
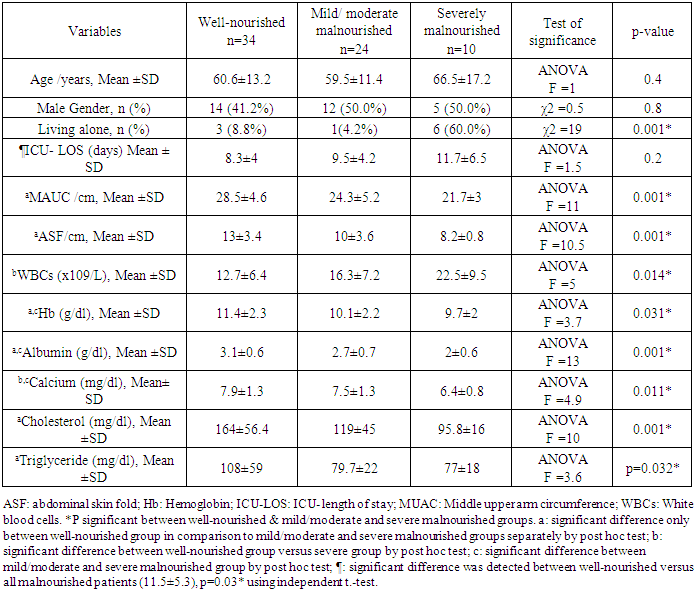
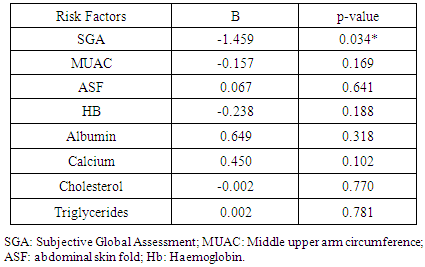
4. Discussion
- Malnutrition is common in the ICU sitting and associated with increased risk of infectious complications, multi-organ dysfunction, and mortality [16]. It has been reported that internal medicine patients are more prone to malnutrition because of their comorbidities [17]. There are few researches which studied the prevalence of malnutrition among ICU patients in Arab world and to our knowledge; this is the first one dealing with this issue in Egypt.In the present study; the prevalence of malnutrition among the medical ICU patients was 50.0% (35.3% & 14.7% were mildly-moderately and severely malnourished respectively). This finding was comparable to another study done by Trakya University on ICU patients staying for more than 24 hours as they reported malnutrition in about half of patients (42.2% were mild-to-moderate and 8% were severely malnourished respectively) [18]. Similarly, Fontes et al., 2014 reported malnutrition in 54% of critically ill patients by using SGA tool [19]. Moreover, higher rate of malnutrition (70%) was detected by Vallejo et al., 2017 [20]. On the contrary, a prospective cohort study in an ICU of a Singapore tertiary hospital reported malnutrition in 28% (mildly-moderately malnourished: 25% and severely malnourished: 3%) using SGA [2]. Differences in the rate of malnutrition depend on type of ICU (medical or surgical) and country (developing or developed). The high prevalence of malnutrition in the current research could be attributed to poor health of studied patients resulting from age related coexisting medical illness mainly hypertension (41.2%) and diabetes (48.5%) which have negative influence on their nutritional status as 60.3% of the study patients were elderly; as well as polypharmacy which is common in older people that can be an iatrogenic cause of malnutrition [21, 22]. Social factors may also play a role as nearly one fifth of malnourished patients were living alone versus only 8.8% of well-nourished patients. Social isolation and financial deprivation with inability to prepare food are important contributors of malnutrition especially in older population [23]. It is widely reported in the literature that malnutrition is associated with an increased length of hospital stay [24, 25]. In the present study; it was found that malnourished patients had a significantly longer length of stay than their well-nourished counterparts. Nutrition plays an important role in patient recovery [26, 27]. On the other hand, Lew et al., 2018, reported no association between malnutrition and ICU-LOS. They attributed this to patients' short stay at ICU which leads to difficult establishment of any association with malnutrition or other parameters [28].Regarding the anthropometric measures, MUAC measurements can be used for assessing adult malnutrition in emergencies [29]. The present study revealed that the mean MUAC and ASF were significantly lower among both mild/moderate or severe groups versus well-nourished patients. These were in agreement to, Gultekin et al., 2016 who detected that triceps skin fold measurement during admission was lower significantly in mild-to-moderate and severe malnourished groups than well-feed group [18]. However, anthropometric measurements have their limitation as they often do not have ethnic specific references and hence has limited generalizability and applicability. Serum proteins have been used as markers of nutritional status, with serum albumin being the most widely adopted because of its ability to predict outcomes in ICU patients [30]. In the present study, it was found that malnourished patients (mild or severe) had a significant lower serum albumin levels versus well-nourished group. Low albumin levels in hospitalized patients was associated with longer periods of hospital stays and increased the risk of being readmitted to the hospital within one year [31]. Malnutrition is also associated with negative outcomes for patients in the term of increased morbidity and mortality [21]. In the present study; it was reported that the overall mortality rate was 41.2%, and it was significantly lower in well-nourished group 26.5% compared to (55.9%) in malnourished group. By performing binary logistic regression; lower nutritional status detected by SGA was the only significant independent predictor negatively for mortality. Also, it was demonstrated the probability of death was about 2 times higher for a patient who is malnourished versus well-nourished patient. These findings were congruent with other studies that reported increase in overall mortality rate among ICU malnourished patients compared with well-nourished patients [19, 26, 32]. On the contrary, Atalay et al, 2008 found no relationship between malnutrition and adverse outcomes including mortality among elderly patients [33]. One centre study and a small sample has been considered as a limitation in this research.
5. Conclusions
- Malnutrition was highly prevalent among medical ICU patients and was associated with increased mortality. Hence; there is a need for adequate nutritional screening and assessment early at admission to ICU for appropriate nutritional plan to minimize the consequences of malnutrition on the patients and health care system. SGA appears to be a good predictor of clinical outcome. Awareness is needed among health care personnel about SGA as a well-validated, feasible, inexpensive and non-invasive nutritional assessment tool for evaluation of the nutritional status routinely in critically ill patients. Social support is crucial to ICU patients especially the elderly, as they are often unable to serve themselves. Further studies are recommended to evaluate this possible association between malnutrition and length of stay in ICU on a larger scale.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML