-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2018; 7(3): 41-43
doi:10.5923/j.ijim.20180703.02

Malignancies Presenting as Disseminated Intravascular Coagulation (DIC)
Ather Pasha, Wasay Kabir
General Medicine, Deccan College of Medical Sciences, Hyderabad, Telangana, India
Correspondence to: Wasay Kabir, General Medicine, Deccan College of Medical Sciences, Hyderabad, Telangana, India.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

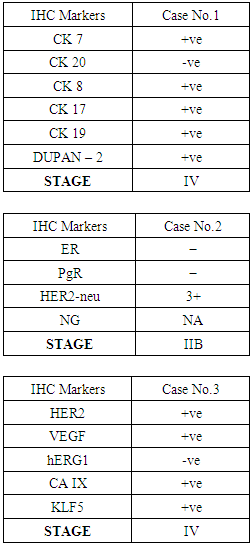
The objective of this study was to describe malignancies presenting as Disseminated Intravascular Coagulation (DIC). The prognosis of Disseminated Carcinomatosis of the Bone Marrow (DCBM) caused by solid tumors which is often accompanied by Disseminated Intravascular Coagulation (DIC is generally very poor. The diagnostic procedures to find the underlying cause of DIC ended up in the discovery of metastatic cancer. Disseminated Carcinomatosis of Bone Marrow (DCBM) is a condition in which the tumour cells metastases diffusely invade the bone marrow, and is frequently accompanied by Disseminated Intravascular Coagulation (DIC). While prostate, lung, breast and stomach malignancies are the most prevalent non-hematological malignancies to metastasize frequently to the bone marrow, pancreatic cancer is a malignancy that rarely metastasizes to the bone marrow. The present study describes 3 patients with DCBM one with pancreatic cancer, second with breast cancer and a third one with gastric cancer. Their laboratory workup confirmed the presence of chronic DIC. Bone marrow biopsies were done which revealed metastatic adenocarcinoma. So PET-CT scans were done which showed metabolically active multiple skeletal lesions. IHC of bone marrow cells was sent for finding primary which showed likely involvement of primary (pancreatobiliary, breast, gastric) system. DCBM derived from solid cancer with DIC has a very poor prognosis and despite all treatments these patients will die soon. In conclusion, malignancies should be considered in cases of DIC, especially in elderly men in whom no underlying cause can be found to explain it. We recommend doing routine investigations before taking patient for any simple procedures in today’s evidence based practice.
Keywords: Malignancy,Disseminated Carcinomatosis of Bone Marrow (DCBM), Disseminated Intravascular Coagulation (DIC), Pancreaticobiliary system cancer, Pancreatic cancer, Breast cancer and stomach cancer
Cite this paper: Ather Pasha, Wasay Kabir, Malignancies Presenting as Disseminated Intravascular Coagulation (DIC), International Journal of Internal Medicine, Vol. 7 No. 3, 2018, pp. 41-43. doi: 10.5923/j.ijim.20180703.02.
Article Outline
1. Introduction
- DIC: Disseminated Intravascular Coagulation is an acute or chronic disorder causing thrombosis or hemorrhage, which occurs as a secondary complication of an underlying disease [9]. It is characterized by consumption of coagulation factors caused by intravascular activation of the coagulation sequence, which leads to the formation of thrombi throughout the microcirculation of the body, and secondarily, activation of fibrinolysis. DIC occurs because of aberrant activation of the clotting cascade, leading to fibrin deposition in small vessels, combined with activation of fibrinolytic mechanisms, leading to bleeding. DIC is usually a common final hemostatic disorder caused by other conditions such as sepsis, pancreatitis, or trauma. Because they are consumed by the ongoing prothrombotic and fibrinolytic processes, coagulation proteins and platelets can become depleted, leading to bleeding. Thus, in DIC, hemorrhage and thrombosis can occur simultaneously. DIC can be an acute or a chronic disorder, and the latter is seen mostly in obstetric and oncology patients. The prognosis of pancreatic cancer improved significantly due to the advances in the treatment. Intra-hepatic metastasis is the most common site of metastasis of pancreatic cancer. The most common sites are lung, intra-abdominal lymph nodes, bone, and adrenal gland. Although bone is one of the common sites for metastasis, the bone marrow is a rare site for metastasis [1]. Bone marrow metastasis is another poor prognostic factor and usually occurs in advanced or terminal stage in cancer treatment. For breast cancer, chances for survival vary by stage of breast cancer. Non-invasive (stage 0) and early stage invasive breast cancers (stages I and II) have a better prognosis than later stage cancers (stages III and IV) [2]. Cancer that has not spread beyond the breast has a better prognosis than cancer that has spread to the lymph nodes. The poorest prognosis is for metastatic breast cancer (stage IV), when the cancer has spread beyond the lymph nodes to other parts of the body [3]. The prognosis of patients with gastric cancer is related to tumor extent and includes both nodal involvement and direct tumor extension beyond the gastric wall. Tumor grade may also provide some prognostic information [4]. Disseminated Carcinomatosis of the Bone Marrow (DCBM) is characterized by diffuse infiltrative growth of tumor cells in the bone marrow and is associated with systemic hematological disorders [5]. Occult cancer cells in the bone marrow have been reported to occur frequently. However, whether the presence of isolated tumor cells in the bone marrow has prognostic significance remains controversial [6]. Furthermore, the association between isolated tumor cells in the bone marrow and clinically symptomatic bone marrow metastasis has not been fully elucidated, whereas clinically evident bone marrow metastasis is relatively common and often progresses to DCBM [7]. When metastasis to the bone marrow progresses to DCBM, a hematological disorder, such as Disseminated Intravascular Coagulation (DIC), is manifested. Therefore, prompt diagnosis and treatment are required to prevent the development of a life-threatening hematological disorder [8].
2. Patients and Methods
- Study design: This is a hospital based prospective observational study.Approval: This study received approval from college ethical committee.Setting: Owaisi Hospital, Hyderabd.Participants: Three patients admitted in Owaisi Hospital.Study period: March 2016 – December 2017
3. Observations and Results
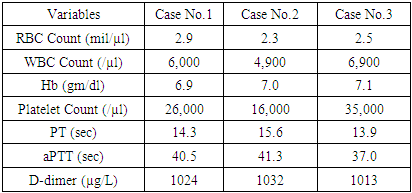
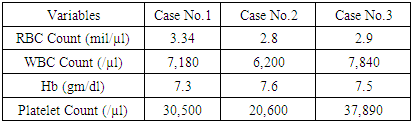
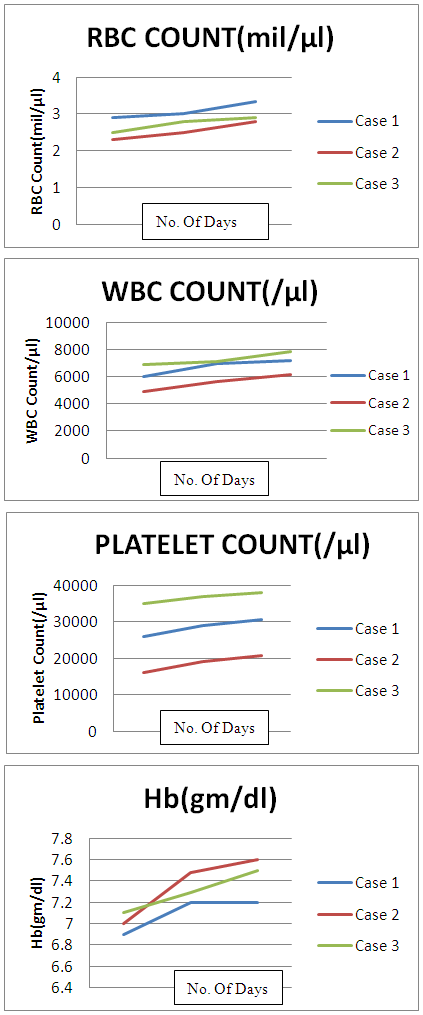
- All the patients had anemia and thrombocytopenia. Their laboratory workup confirmed the presence of chronic DIC. The known risk factors making patients more susceptible to DIC include: older age, advanced tumor stage, and primary tumor necrosis. Considering these risk factors our patients were at great risk of DIC. Our patients had bicytopenia, which we thought would be due to Prostatis/ complicated UTI / post procedure state leading to sepsis / indegenous medicines causing B.M suppression. So we gave initial treatment with antibiotics, PRBC transfusion & insulin infusion. There was partial response to this treatment, so we thought of some other cause.
|
|
 | Figure 1 |
4. Discussion
- All the patients had anemia and thrombocytopenia. Their laboratory workup confirmed the presence of chronic DIC. Our patients had bicytopenia, which we thought would be due to Prostatis/ complicated UTI / post procedure state leading to sepsis / indegenous medicines causing B.M suppression. So we gave initial treatment with antibiotics, PRBC transfusion & insulin infusion. There was partial response to this treatment, so we thought of some other cause. With partial response to antibiotics, continuous fever & fall in platelets, PET-CT was done which showed metabolically active multiple skeletal lesions. Bone marrow biopsy revealed metastatic adenocarcinoma cells. IHC of bone marrow cells was sent for confirmation which showed likely involvement of pancreaticobiliary system, breast and stomach cancer. The patients final diagnosis was metastatic cancer with diffuse bone metastases with chronic DIC. DCBM derived from solid cancer with DIC has a very poor prognosis and despite all treatments these patients will die soon. So, malignancies should be considered in cases of DIC.
5. Conclusions
- In conclusion, malignancies should be considered in cases of DIC, especially in elderly men in whom no underlying cause can be found to explain it. So simple overlooked hematological signs and symptoms can be a part of dreaded disease, we recommend doing routine investigations before taking patient for any simple procedures in today’s evidence based practice.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML