-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2018; 7(3): 37-40
doi:10.5923/j.ijim.20180703.01

Upper Gastrointenstinal Bleeding: A Prospective Clinical Study
Sushant Sethi1, Rasmirekha Behera2
1Department of Gastroenterology Apollo Hospital Bhubaneswar, India
2Department of Pharmacology I.M.S & SUM Hospital Bhubaneswar, India
Correspondence to: Rasmirekha Behera, Department of Pharmacology I.M.S & SUM Hospital Bhubaneswar, India.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

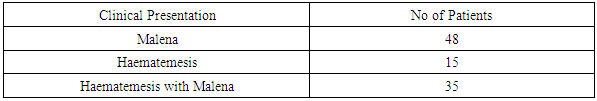
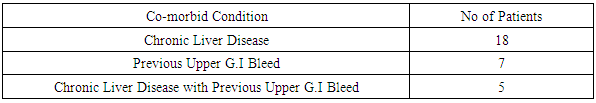
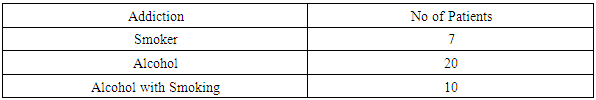
Introduction: Gastrointenstinal bleeding also known as gastrointenstinal hemorrhage is all forms of bleeding in the gastrointenstinal tract from mouth to the rectum. Upper gastrointenstinal bleeing includes hemorrhage originating from above ligament of Treitz. GI bleeding can be potentially life threatening. Upper GI bleed usually present with hematemesis, coffee-ground emesis or malena. Acute upper GI bleeding is assessed by risk scores such as Rockall Score and Glasgow Blatchford Score. Aim: To study the Clinical aspects of Upper Gastrointenstinal Bleeding in a Tertiary Care Hospital. Methods: Total 100 patients were included for a period of one year. Patient with age above 18 yrs and below 60yr of both sexes presenting with gastrointenstinal bleed were included. All the patients were stabilized & subjected to endoscopic procedure within 72hrs. Severity was assessed by Rockall Score. Result: In this study the most common clinical presentation is malena. Chronic liver disease is the most frequent associated co-morbid condition. There is a association of alcohol with that of upper g.i bleed. Conclusion: Upper G.I Bleed is a common medical emergency. In this study conducted in a tertiary care hospital the most common presentation of upper GI bleed is malena. It is associated with the more incidence of duodenal ulcer. The frequent associated co-morbid condition is chronic liver disease. Alcohol shares a significant role in onset of upper GI bleed.
Keywords: Upper Gastrointenstinal Bleeding, Malena, Haematemesis, Chronic Liver Disease
Cite this paper: Sushant Sethi, Rasmirekha Behera, Upper Gastrointenstinal Bleeding: A Prospective Clinical Study, International Journal of Internal Medicine, Vol. 7 No. 3, 2018, pp. 37-40. doi: 10.5923/j.ijim.20180703.01.
1. Introduction
- Gastrointenstinal bleeding (GI bleed) also known as gastrointenstinal hemorrhage is all forms of bleeding in the gastrointenstinal tract from the mouth to the rectum. [1] Gastrointenstinal Bleeding is typically divided into two main types: Upper gastrointenstinal bleeeing and lower gastrointenstinal bleeding. [2] Upper gastrointenstinal bleeding includes hemorrhage originating from the esophagus to the ligament of Treitz. Peptic ulcer bleeding causes more than 60 percent of cases of upper gastrointenstinal bleeding, where as oesophageal varices cause approximately 6 percent. Other etiologies include Arteriovenous malformations, Mallory Weiss tear, gastritis and duodenitis and malignancy. [3] Drugs associated with gastrointenstinal haemorrhage includes Aspirin, NSAIDs, Prednisolone, warfarin, Clopidogrel, SSRIs. Aspirin, NSAIDs, Prednisolone cause gastrointenstinal haemorrhage by Mucosal toxicity. Warfarin, Clopidogrel, SSRIs cause gastrointenstinal haemorrhage by impaired haemostasis. [4] Other relatively common causes include esophagitis, erosive gastritis/duodenitis, vascular ectasia and Dieulafoy’s lesions. [5] Acute upper gastrointenstinal haemorrhage is a common medical emergency (170 per 100 000 adults annually). Although its incidence may be declining, the mortality rate of upper gastrointenstinal haemorrhage remains high, approximately 6-8%. [6] Upper gastrointenstinal bleeding is twice as common in men as in women and increases in prevalence with age. [3] GI bleeding can be potentially life threatening, it has been shown that many cases can be safely managed on an outpatient basis. [7] Despite advances in therapy, the in-hospital mortality rate remains high (13 percent) and rebleeding is common (15 percent). [8, 9] Depending on the rate of blood loss, GI bleeding can manifest in several forms and can be classified as overt, occult or obscure. Overt GI bleeding, otherwise known as acute GI bleeding, is visible and can present in the form of hematemesis, “coffee-ground” emesis Malena, or hematochezia. Occult or chronic GI bleeding as a result of microscopic hemorrhage can present as Hemooccult-positive stool with or without iron deficiency anaemia. [10, 11] Upper GI bleeding usually presents with hematemesis (vomiting of fresh blood), “coffee-ground” emesis (vomiting of dark altered blood), and/or malena (black tarry stools). Hematochezia (passing of red blood from rectum) usually indicates bleeding from the lower GI tract, but can occasionally be presentation for a brisky bleeding from upper GI source. [12] The presence of frank bloody emesis suggests more active and severe bleeding compared to coffee-ground emesis. [13] Rapid assessment and resuscitation should precede diagnostic evaluation in unstable patients with acute severe bleeding. [14] Once hemodynamic stability is assured, patient should be evaluated for the immediate risk of rebleeding and complications, as well as the underlying source of bleeding. For an acute upper GI bleeding, risk scores such as the Rockall Score and Glasgow Blatchford Score (GBS) have been developed and validated. [7, 15]
2. Material and Methods
- The study was conducted in Apollo Hospital Bhubaneswar in the Dept of Gastroenterology.Total 100 patients were included. The study period was one year i.e Jan 2017-Dec 2017.Inclusion Criteria: Patients with age more than 18yrs and less than 60 yrs of both sexes presenting with gastrointenstinal bleeding irrespective of underlying cause.Exclusion Criteria:a. Patients who have undergone UGI endoscopy or sigmoidoscopy orcolonoscopy within last 1 monthb. Patients who did not give consent for procedurec. Patients not fit for endoscopyd. Patients who were having GI bleed following GI surgeryFirst the patient were, assessed if needed resuscitated followed by necessary clinical and laboratory investigation. After initial hemodynamic stabilization was achieved patients were subjected to endoscopic procedure within 72hrs to determine the cause.Study Design:This is a prospective cohort study conducted for one year. Patients were diagnosed as Upper g.i bleed according to clinical presentation and upper GI endoscopy. Severerity was assessed with Rockall Score.Statistical Analysis:All datas were analysed using Chi-square Test. p<0.05 considered as statistically significant and p<0.001 as highly significant.
3. Result
- Among 100 patients 82 patients were Male and 18 patients were females.
|
|
|
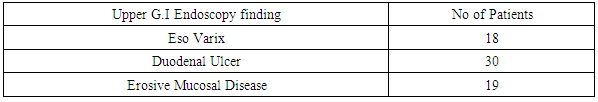
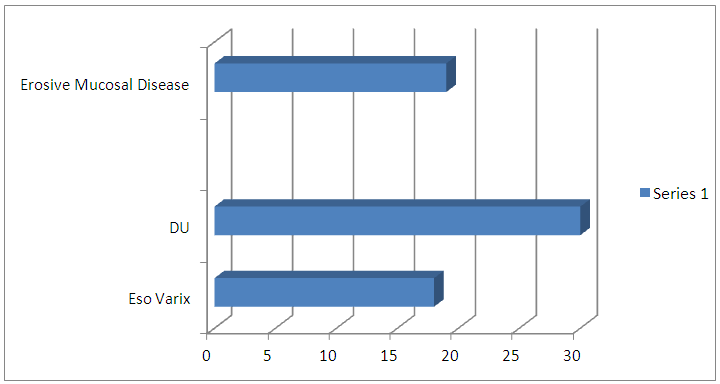 | Upper G.I Endoscopy finding (Graph-1) |
|
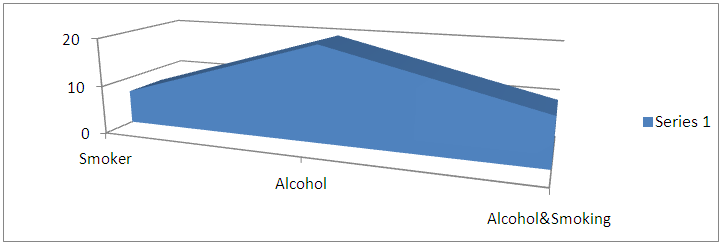 | Association of addiction with Upper G.I bleeding (Graph-2) |
4. Discussion
- Chronic liver disease refers to disease of the liver which lasts over a period of six months. It consists of a wide range of liver pathologies which include chronic hepatitis, liver cirrhosis & hepatocellular carcinoma. The pathology of alcoholic liver disease consists of three major lesions, with the progressive injury rarely existing in a pure form: fatty liver, patients with cirrhosis have portal hypertension, alcoholic hepatitis, Cirrhosis. [16] It is worthwhile emphasising that mortality is often due to medical comorbidity, rather than uncontrolled bleeding. [17] In patients with acute upper GI bleeding, upper g.i endoscopy is considered the investigation of choice. [18] Early upper endoscopy within 24 hr of presentation is recommended in most patients with acute upper GI bleeding to confirm diagnosis and has the benefit of targeted endoscopic treatment, resulting in reduced morbidity, hospital length of stay, risk of recurrent bleeding and the need for surgery. [14] In other studies main causes of acute upper GI bleeding is Non-Variceal Upper GI bleed (80-90%) and Variceal Upper GI bleed 10-20%. [19]
5. Conclusions
- Upper G.I Bleed is a common medical emergency. In this study conducted in a tertiary care hospital the most common presentation of upper g.i bleed is malena. It is associated with more incidence of duodenal ulcer. The frequent co-morbid condition associated is chronic liver disease. Alcohol shares a significant role in onset of upper g.i bleed.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML