-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2018; 7(2): 31-35
doi:10.5923/j.ijim.20180702.03

Cardiac Manifestations in Overt and Subclinical Hypothyroidism Subjects in a Tertiary Care Centre
Ravishankar M. S.1, Harish Kumar S.2, Balachandra G.1
1Department of General Medicine, BGS Global Institute of Medical Sciences, Bangalore, India
2Department of General Medicine, SDUMC, Kolar, India
Correspondence to: Harish Kumar S., Department of General Medicine, SDUMC, Kolar, India.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

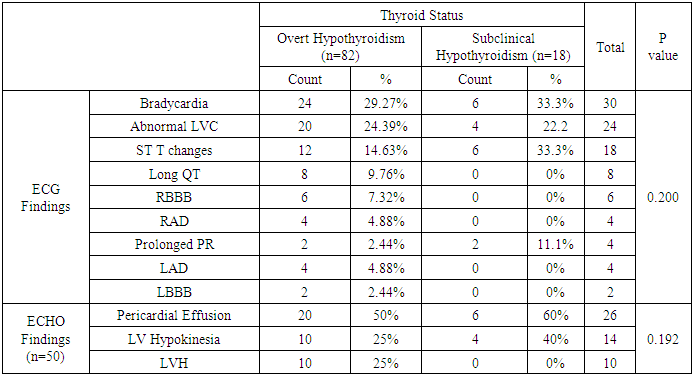
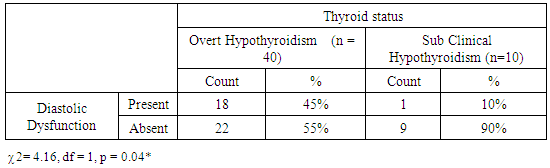
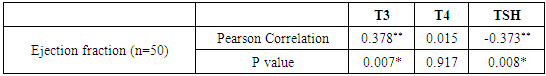
Background: Thyroid hormones are very vital for the normal functioning of heart. Cardiovascular manifestations are frequent findings hypothyroidism. Hypothyroidism and can produce changes in cardiac contractility, myocardial oxygen consumption, cardiac output, blood pressure and systemic vascular resistance. Most cardiac abnormalities return to normal once a euthyroid state has been achieved. Methods: Cross sectional study on 100 cases of hypothyroidism was carried out in a tertiary care centre. Structured questionnaire was to collect information from subjects with respect to history, clinical examination and investigations. ECGs and 2D ECHO was done to find the cardiac changes and diastolic dysfunction. Data was analyzed using SPSS 22 version software. Chi-square was used as test of significance. Pearson correlation was done to find the correlation between two quantitative variables. p value <0.05 was considered as statistically significant. Results: Mean age of subjects was 43.54 ± 11.2 yrs. Majority of them were in the age group > 50 years (34%). Females constituted 72% and males were 28%. Commonest symptom on presentation was Dyspnea (60%). 82% of subjects had Overt Hypothyroidism and 18% had Subclinical Hypothyroidism. On ECG, 30% had Bradycardia, 24% had abnormal LVC, 18% had ST T changes, 8% had long QT, 6% had RBBB, 4% had RAD, prolonged PR and LAD respectively and 2% had LBBB. On Echo 52% had pericardial effusion, 28% had LV Hypokinesia and 20% had out of 40 subjects with Overt Hypothyroidism, 45% had diastolic dysfunction and out of 10 subjects with Sub Clinical Hypothyroidism, 10% had diastolic dysfunction. Significant Positive correlation was observed between T3 and Ejection Fraction and Significant Negative correlation was observed between TSH and Ejection Fraction. Conclusion: Study concludes that there was significant association of hypothyroidism with cardiac diseases especially those of diastolic dysfunction and pericardial effusion. The findings suggest the importance of early detection and effective treatment of cardiac abnormalities in patients affected by thyroid disorders.
Keywords: Hypothyroidism, Electrocardiographic changes, Echocardiography changes, Diastolic dysfunction
Cite this paper: Ravishankar M. S., Harish Kumar S., Balachandra G., Cardiac Manifestations in Overt and Subclinical Hypothyroidism Subjects in a Tertiary Care Centre, International Journal of Internal Medicine, Vol. 7 No. 2, 2018, pp. 31-35. doi: 10.5923/j.ijim.20180702.03.
Article Outline
1. Introduction
- Thyroid dysfunction is relatively common, and its prevalence increases with advancing age. An estimated 108 million people in India suffer from endocrine and metabolic disorders. Thyroid disorders are the most common among all the endocrine diseases in India and hyperthyroidism and hypothyroidism are more frequent in women. Functional studies of the goitrous subjects showed overall prevalence of 5.4% hypothyroidism, 1.9% hyperthyroidism. [1, 2]Hypothyroidism is the most common pathological hormone deficiency. Pathology of thyroid gland (primary hypothyroidism) accounts for over 99.5% of cases of thyroid gland failures and <0.5% result from disorders of the pituitary gland or hypothalamus (central hypothyroidism). [3]Adverse cardiovascular effect of hypothyroidism has been identified in many studies. Most of the studies focused on systolic/diastolic dysfunction in hypothyroidism. [4, 5]Early identification of patients with overt hypothyroidism and sub-clinical hypothyroidism may lead to early treatment and thereby favourable effect on cardiovascular morbidity and mortality. Hence this study was done with the objective to determine the cardiac manifestations in overt and subclinical hypothyroidism and to find the association b/w left ventricular diastolic dysfunction overt and subclinical hypothyroidism.
2. Materials and Methods
- A cross sectional study was carried out among 100 cases of hypothyroidism (Overt and Subclinical hypothyroidism) in a tertiary care centre for a period of 18 months. Written informed consent was obtained from all the subjects before including in to the study. Institutional ethical clearance was obtained prior to the start of the study. Patients on antiarrhythmic drugs, with known cardiac disease, conditions causing LV hypertrophy, conditions rendering myocardium stiff and any chronic medical or surgical condition which may independently effect the left ventricular function were excluded from the study. Sample size was estimated by using the proportion of hypothyroid subjects with diastolic dysfunction as 17.9% from the study by Gupta et al. [6, 8] By using the formula n = Z 1-α/22p(1-p) / d2. Considering p as 18.8%, q as 81.2% and d (precision) at 10% and at 99% confidence level, sample size of 100 was obtained and was included in the study. Simple random sampling was done on out patients and inpatients undergoing thyroid function tests such as - TSH, free T3 and free T4. Structured questionnaire was to collect information from subjects with respect to history, clinical examination and investigations. Overt hypothyroidism refers to cases in which serum thyrotropin (TSH) concentration is elevated (>4.68 uIU/ml) and serum T4 (free thyroxine) is below the reference range (<0.78 ng/dl). Subclinical hypothyroidism is defined as a serum thyroid stimulating hormone (TSH) above the defined upper limit of the reference range (>4.68 uIU/ml), with a serum free thyroxine (T4) within the reference range. (0.78-1.79 ng/dl). ECGs were taken accordingly to look for abnormal signs and left ventricular dysfunction based on the preformed criteria. Those with suspected ECG abnormalities were subjected to 2D ECHO to look for left ventricular diastolic dysfunction. Statistical analysis: Data was analyzed using SPSS 22 version software. Categorical data was represented in the form of Frequencies and proportions. Bar diagrams and Pie diagrams were used to show the data graphically. Chi-square was used as test of significance. Continuous data was represented as mean and standard deviation. Independent t test was used as test of significance to identify the mean difference between two groups. Pearson correlation was done to find the correlation between two quantitative variables. p value <0.05 was considered as statistically significant.
3. Results
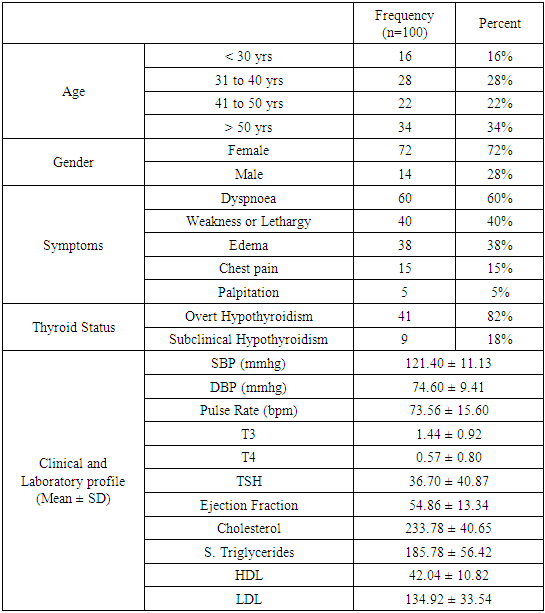
- Data of 100 hypothyroid subjects fulfilling the inclusion and exclusion criteria were included for analysis. Mean age of subjects was 43.54 ± 11.2 yrs. Majority of them were in the age group > 50 years (34%). Females constituted 72% and males were 28%. Commonest symptom on presentation was Dyspnea (60%), Lethargy (40%), edema (38%) chest pain (15%) and palpitations (5%). 82% of subjects had Overt Hypothyroidism and 18% had Subclinical Hypothyroidism. Mean T3 levels was 1.44 ± 0.92, mean T4 levels was 0.57 ± 0.80 and mean TSH levels was 36.70 ± 4.87 (Table 1).
|
|
|
|
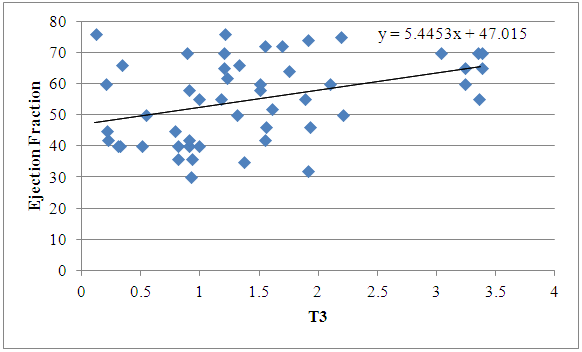 | Figure 1. Scatter Plot Showing Positive Correlation between T3 and Ejection Fraction |
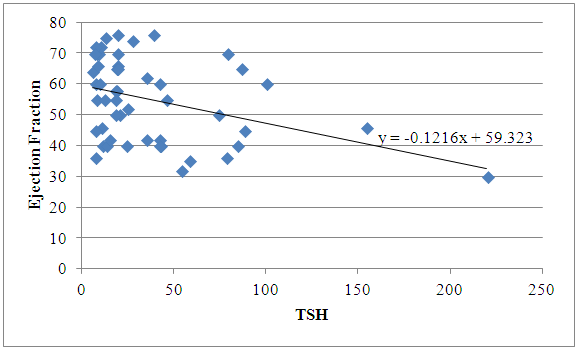 | Figure 2. Scatter Plot showing Negative Correlation between TSH and Ejection Fraction |
4. Discussion
- In the present study, 100 patients of hypothyroidism were studied for cardiovascular changes and left ventricular diastolic dysfunction. Of them 82% had overt hypothyroidism and 18% had subclinical hypothyroidism. Al-Farttoosi et al.58 in their study observed breathlessness in 75% of patients, angina in 11.1%, edema in 47.2% and Bradycardia in 47.2%. Al-Farttoosi et al. [7] found in their study that 47.2% had sinus Bradycardia, 33.3% had low voltage complex, 27.8% had ST-T changes, 19.5% had long QT and prolonged PR respectively. Similarly Agarwal et al. [8] study showed low average pulse rate in hypothyroid patients, 15% patients had low voltage complex and 10% of patients had ST-T changes. Gupta et al. [6] in their study observed that 18.18% had diastolic dysfunction, 45.5% had pericardial effusion. Similarly Hardisty et al. [9] and Rawat et al. [10] observed that 32.5% and 72% had pericardial effusion. Verma et al. [11] concluded from his study that pericardial effusion and diastolic dysfunction was seen in significant cases of hypothyroidism.Qari FA [12] observed significant positive correlation between EF and the FT3 level (r=0.818; p value=0.045). Hemodynamic alterations in hypothyroidism cause narrowing of pulse pressure, prolongation of circulation time and decrease in blood flow to tissues. In severe primary hypothyroidism the cardiac silhouette is enlarged and heart sounds decrease in intensity due to pericardial effusion [13]. Changes in myocardial contractility and cardiovascular haemodynamics occur across entire spectrum of thyroid disease. T3 regulates cardiac ionotrophy and chronotrophy through a variety of both direct and indirect mechanisms. Cardiac output may decrease by as much as 30-40% in hypothyroidism. Cardiovascular findings of hypothyroidism are more subtle. Signs and symptoms of hypothyroidism include mild degree bradycardia, diastolic hypertension, a narrowed pulse pressure, cold intolerance and quiet precordium. [14, 15, 16] Subclinical hypothyroidism is associated with impaired left ventricular diastolic function at rest, systolic dysfunction on effort and enhanced risk for atherosclerosis and myocardial infarction. Subclinical hyperthyroidism is associated with increased heart rate, atrial arrhythmias, increased left ventricular mass with marginal concentric remodeling, impaired ventricular relaxation, reduced exercise performance and increase risk for cardiovascular death [17].
5. Conclusions
- Study concludes that there was significant association of hypothyroidism with cardiac diseases especially those of diastolic dysfunction and pericardial effusion. The findings suggest the importance of early detection and effective treatment of cardiac abnormalities in patients affected by thyroid disorders.
Limitation
- Effect of thyroid hormones treatment and its impact on reversibility of diastolic dysfunction in hypothyroidism was not seen. Control group would have helped in the comparison of cardiac abnormalities with hypothyroid group.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML