-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2018; 7(2): 26-30
doi:10.5923/j.ijim.20180702.02

Coarctation of Aorta in a 21-year-old Female: A Case Report
Ngongang Ouankou Christian1, 2, Tsambang Djeufack Wilfried Lionel3, Magny Thiam Eric1, 2, Bitchou Marie Philomene1, Wandji Ngamga Josée Christiane2, Chendjou Kapi Léana Oriane4, Tankeu Tiakouang Aurel2, Kenfack Monique1, Ndongo Amougou Sylvie1, 2, Kuate-Mfeukeu Liliane2, Wawo Yonta Edwine5, Jonte Mbianda Klod Paturelle4, Tchuisseu Kwangoua Larissa Ange2, Tchikapa Joachim2, Azabji Kenfack Marcel2, Nganou Chris Nadege2, Djomou Ngongang Armel Florent4, Boombi Jérôme2, Ouankou Mérimée Débozard6, Kingue Samuel2, Ngu Blackett Kathleen2
1Internal Medicine and Specialities, University Hospital Center Yaounde, Cameroun
2Faculty of Medicine and Biomedical Sciences, University of Yaounde I, Cameroun
3Higher Institute of Medical Technology Nkolondom Yaounde, Cameroun
4Université Des Montagnes, Institut Supérieur des Sciences de la Santé (ISSS), Cameroun
5Centre Médical Hippodrome Yaoundé, Cameroun
6Centre Cardiologique et Médical, Cameroun
Correspondence to: Ngongang Ouankou Christian, Internal Medicine and Specialities, University Hospital Center Yaounde, Cameroun.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: The aortic coarctation is a congenital malformation of the aorta, characterised by the narrowing of the aorta. It represents for 5 – 10% of congenital heart diseases and it shows a male predominance. Its diagnosis is usually posed and treatment done early in life. Objective: In this case report, we present a late diagnosis of isthmic aortic coarctation in a 21-year-old female. Clinical and para-clinical presentation: The patient was relatively asymptomatic until she was fortuitously diagnosed with hypertension. Physical examination showed blood pressures of 182/89 mmHg (left arm) and of 194/89mmHg (right arm), a bradycardia of 52 beats/minute. On cardiovascular physical assessment was recorded a systolic murmur of intensity 3/6, posterior over the thoracic spine and subclavicular space and a decrease in femoral pulse. Biological exams such as creatininemia and kalemia were normal. The transthoracic echocardiogram showed a stenosis at the isthmic part of the descending aorta, with an increased peak velocity of 3.6 m/s (max gradient = 50 mmHg) and no associated patent ductus arteriosus. Thoracic computerised tomographic (CT) angiography showed an aortic isthmus coarctation with a rounded arch. The CT angiography also recorded duplicated superior vena cava, dilatation of collateral partway below the coarctation to hypertrophied intercostal, internal mammary artery dilatation and Cardiomegaly with left ventricular dilatation. The electrocardiogram recorded a sinus bradycardia at 47 bpm. The chest X-ray noted an enlargement of the cardiac figure, without notching of the ribs. She was addressed to the Cardiac Center of Saint Elisabeth Catholic Hospital of Shison for a surgical management. Meanwhile, she was placed on combined therapy (Atenolol 50mg and Nifedipine 20mg daily) and a good clinical condition was achieved. Conclusion: A fortuitously discovered case of late aortic coarctation, diagnosed in a 21 year female during the evaluation of an asymptomatic hypertension. Echocardiographic assessment permitted to pose de diagnosis. Prior to surgical management, Blood pressure controlled was achieved on pharmacological treatment. Due to financial constraint her interventional therapy is pending. The particular aspect in this case was the association of a duplicated superior vena cava.
Keywords: Aortic isthmic coarctation, Hypertension, Young, Echocardiography, CT angiography
Cite this paper: Ngongang Ouankou Christian, Tsambang Djeufack Wilfried Lionel, Magny Thiam Eric, Bitchou Marie Philomene, Wandji Ngamga Josée Christiane, Chendjou Kapi Léana Oriane, Tankeu Tiakouang Aurel, Kenfack Monique, Ndongo Amougou Sylvie, Kuate-Mfeukeu Liliane, Wawo Yonta Edwine, Jonte Mbianda Klod Paturelle, Tchuisseu Kwangoua Larissa Ange, Tchikapa Joachim, Azabji Kenfack Marcel, Nganou Chris Nadege, Djomou Ngongang Armel Florent, Boombi Jérôme, Ouankou Mérimée Débozard, Kingue Samuel, Ngu Blackett Kathleen, Coarctation of Aorta in a 21-year-old Female: A Case Report, International Journal of Internal Medicine, Vol. 7 No. 2, 2018, pp. 26-30. doi: 10.5923/j.ijim.20180702.02.
1. Case Presentation
- We report the case of a relatively asymptomatic 21 year old woman in whom a grade III Hypertension was fortuitously discovered during a systematic visit in September 2017. She was addressed for a cardiologist consultation during which was recorded elevated blood pressure values on physical examination. She had a blood pressures of 182/89 mmHg (left arm) and of 194/89mmHg (right arm), a bradycardia of 52 beats/minute. On cardiovascular physical assessment was recorded a systolic murmur of intensity 3/6, posterior over the thoracic spine and sub-clavicular space. Femoral pulses were palpable bilaterally but weak and delayed compared to the brachial pulses. Her ambulatory blood pressure measurement (ABPM) showed a permanent systolic and paroxystic diastolic hypertension, with a daytime adrenergic component in a dipper. A regular sinus bradycardia on electrocardiographic examination with heart rate of 47 beats per minute. A mild enlarged cardiac silhouette without notching of the ribs were observed on the chest radiography (Figure 1). The transthoracic echocardiogram showed a stenosis at the isthmic part of the descending aorta, with an increased peak velocity of 3.6 m/s (max gradient = 50 mmHg) (Figure 2) and no associated patent ductus arteriosus. Thoracic computerised tomographic (CT) angiography showed an aortic isthmus coarctation with a rounded arch (Figure 3A), the presence of a duplicated superior vena cava ( Figure 4A), dilatation of collateral partway below the coarctation to hypertrophied intercostal (Figure 4B), internal mammary artery dilatation (Figure 3B) and Cardiomegaly with left ventricular dilatation; no lungs lesion. These findings are represented in figures below. Biological assessment done for renal function, glycaemia, lipid profile and blood uric acid level where normal. The patient was placed on Atenolol 50mg and Nifedipine 20mg daily then referred to cardiothoracic surgery for an angioplasty.
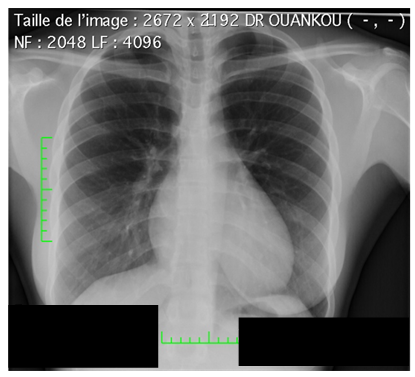 | Figure 1. Mild cardiomegaly on chest radiography, without rib notching |
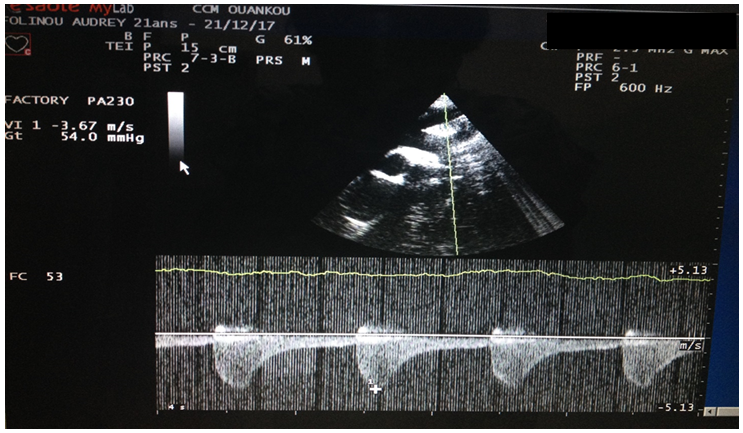 | Figure 2. Continuous wave Doppler characteristics, including high speed jet spectrum during systole and extended speed reduction during diastole |
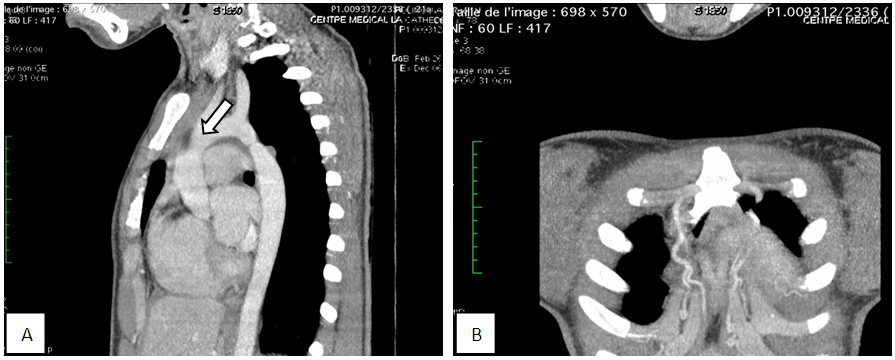 | Figure 3. (A) Coarctation of the aorta: oblique sagittal reconstruction; (B) Hypertrophy of the internal mammary arteries: coronal reconstruction |
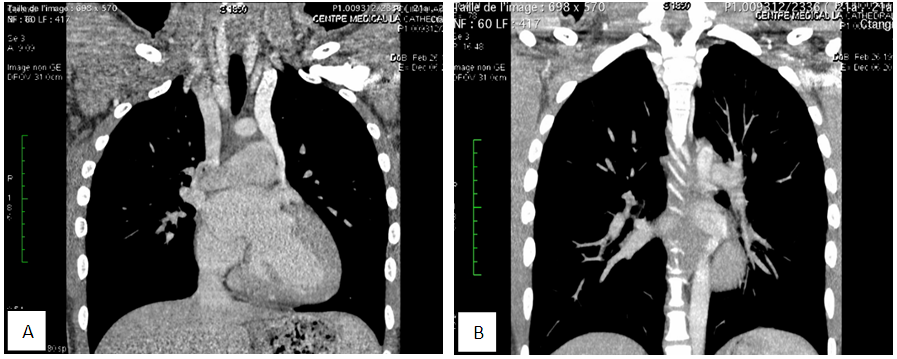 | Figure 4. (A) CT angiography showing the presence of a duplicated superior vena cava; (B) Intercostal artries hypertrophy: coronal reconstruction |
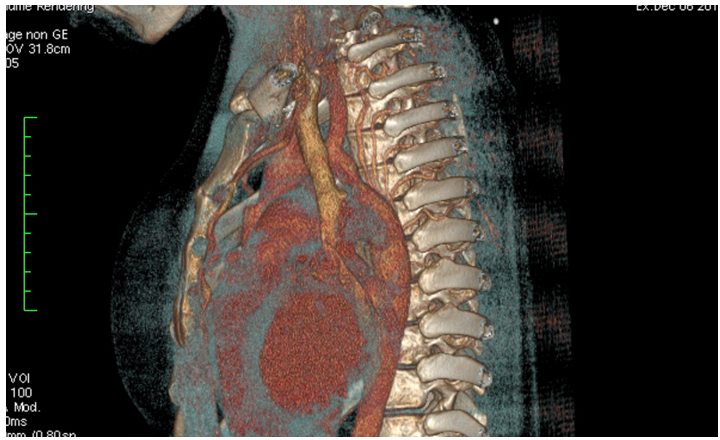 | Figure 5. Volume reconstruction with surface rendering |
2. Discussion
- Aortic coarctation is a congenital vascular lesion typically diagnosed in early life, accounting for 5 to 10% of all congenital cardiovascular malformations [1] but may go undetected well until adulthood [2]. Its clinical presentation beyond infancy is usually asymptomatic. However, they may be clinical signs as: hypertension, headache, nosebleed, leg cramps, muscle weakness, cold feet, or neurologic changes may be seen [3]. Diagnosis is usually based on clinical suspicion and physical findings [4, 5]. The latter include blood pressure difference between the upper and lower extremities, pulse delay and systolic murmur over the thoracic spine [3, 6]. This malformation is usually associated to the turner syndrome or some congenital cardiac defects like left side obstructive or hypoplastic defects and ventricular septal defects, bicuspid aortic valve, aortic arch hypoplasia, and rarely, various right side obstructive lesions [7]. In this case, we reported a relatively asymptomatic patient until she was fortuitously recorded hypertension during a routine check-up. The clinical suspicion was evident with classical findings in aortic coarctation such as permanently high blood pressure (grade 3 ESH); a typical systolic murmur on examination and a weak and delay femoral pulse. Moreover, there are paucity of reported cases of patients first diagnosed with uncorrected aortic coarctation at very late age [3, 8, 9]. A morphological diagnostic imaging is essential to determine the location, characteristics and severity of lesions. Ultrasound diagnosis for aortic coarctation has an accuracy rate of 90.6%, from a study from by Zhenxing Sun and collaborators [10]. In our case echocardiography permitted pose the diagnosis. This case presented a patient with isthmic aortic coarctation which describes some common diagnostic features described in literature and some absent of common features such as: no rib notching and no common associated cardiovascular defects were founded [11, 6]. Whereas, an uncommon abnormality was founded in this case with a duplicated superior vena cava. Patient management consisted of antihypertensive therapy, endocarditis prophylaxis and surgical corrective treatment for coarctation lesions is pending. In accordance to actual protocols [12]. This correction will be through an intravascular stent therapy. Once the stent is positioned across the obstructive lesion, inflating the balloon results in implantation of the stent. The diameter over which the stent is mounted will determine the diameter of the implanted stent [13]. A study demonstrated a procedural success of 97.9% [14]. Nevertheless, are described rare incidence at 1.6% of Aortic wall complications, including dissection or rupture, which may lead to circulatory collapse and death [14]. Multicentre reports showed excellent acute, intermediate and long-term success of stent placing. A report in a cohort of 302 patients showed acute procedural success of 96%, intermediate success of 86% (41% of the patients from the cohort completed follow-up), and long-term success of 77% of patients [15].
3. Conclusions
- Through this case, we presented a young female with an aortic coarctation fortuitously discovered during the evaluation of an asymptomatic hypertension. The diagnostic was easily obtained during her echocardiographic assessment. Prior to surgical management, Blood pressure controlled was achieved on pharmacological treatment. Due to financial constraint her interventional therapy is pending. The particular aspect in this case was the association of a duplicated superior vena cava.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML