-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2018; 7(1): 4-7
doi:10.5923/j.ijim.20180701.02

HbA1C as a Predictor of Left Ventricular Diastolic Dysfunction (LVDD) in Type 2 Diabetic Patients
Srinivasa S. V., Modugula S. Naga Swetha, Abhishek Kumar Verma, Prabhakar K.
Department of General Medicine, Sri Devaraj Urs Medical College, Kolar, India
Correspondence to: Modugula S. Naga Swetha, Department of General Medicine, Sri Devaraj Urs Medical College, Kolar, India.
| Email: |  |
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Diabetes mellitus is a worldwide health problem, affecting millions of people in both developed and developing countries. Cardiovascular diseases like congestive heart failure, coronary artery disease, myocardial infarction which are commonly associated with diabetes are the leading cause of mortality in diabetic patients. Diabetes, itself can lead to the development of heart failure (HFnEF) referred to as diabetic cardiomyopathy. Objective: To assess the correlation of HBA1C levels with left ventricular diastolic dysfunction in newly diagnosed Type 2 diabetic patients. Materials and Methods: The present study was conducted in R L Jalappa hospital, Kolar, Karnataka. All the newly detected type 2 diabetic patients (detected within one month) presented to the OPD and admitted to wards of department of General Medicine, fulfilling the inclusion criteria were included in the study. Sample size of 100 is obtained by the formula n = 4pq/d2 with 95% confidence level, 10% error and 5% alpha error. It was a observational prospective (cross sectional) type of study. Results: 56 out of 100 participants (56%) were males and 44 (44%) were females. Age of the patients was between 42 to 58 yrs, with mean age being 52 years. Mean age of subjects with LVDD was 52.68± 5.69 years and that of population without LVDD was 46.38 ±5.15 years. The mean HbA1C of subjects with LVDD was 7.95 ±1.09 and of subjects without LVDD was 7.21 ± 1.22. HbA1c level is positively associated with the incidence of LVDD in diabetic population as mean HbA1C of population. Conclusion: Our study showed that HbA1c is a reliable predictor of LVDD in the newly diagnosed cases of type 2 diabetes mellitus.
Keywords: Glycocylated Hemoglobin, Left Ventricular Diastolic Dysfunction, Type 2 Diabetes Mellitus
Cite this paper: Srinivasa S. V., Modugula S. Naga Swetha, Abhishek Kumar Verma, Prabhakar K., HbA1C as a Predictor of Left Ventricular Diastolic Dysfunction (LVDD) in Type 2 Diabetic Patients, International Journal of Internal Medicine, Vol. 7 No. 1, 2018, pp. 4-7. doi: 10.5923/j.ijim.20180701.02.
Article Outline
1. Introduction
- Diabetes mellitus is a worldwide health problem, affecting millions of people in both developed and developing countries [1]. Cardiovascular diseases like congestive heart failure, coronary artery disease, myocardial infarction which are commonly associated with diabetes are the leading cause of mortality in diabetic patients. [2, 3] Diabetes, itself can lead to the development of heart failure (HFnEF) referred to as diabetic cardiomyopathy [4]. Hyperglycaemia in poorly controlled diabetes leads to production of advanced glycation end products and free radicals. Both can cause elevated collagen deposition in myocardium leading to myocardial fibrosis and thus effecting contractility and relaxation of heart [5]. Hence a poor glycemic control can be associated with high chances of having left ventricular hypertrophy and left ventricular diastolic dysfunction (LVDD). Several studies have identified left ventricular diastolic dysfunction (LVDD) as the first manifestation of myocardial involvement in diabetes. [6, 7, 8] Hence, the early identification of LVDD among type 2 diabetes patients might have relevant clinical, prognostic, and economic implications by preventing or delaying the evolution of overt HF. As poor glycemic control can be associated with LVDD, the aim of the present study is to verify whether HbA1c levels can detect left ventricular diastolic dysfunction in type-2 diabetic patients.
2. Objective of the Study
- × To assess the correlation of HBA1C levels with left ventricular diastolic dysfunction in newly diagnosed Type 2 diabetic patients.
3. Materials and Methods of Study
- The present study was conducted in R L Jalappa hospital, Kolar, Karnataka. All the newly detected type 2 diabetic patients (detected within one month) presented to the OPD and admitted to wards of department of General Medicine, fulfilling the inclusion criteria were included in the study. Sample size of 100 is obtained by the formula n = 4pq/d2 with 95% confidence level, 10% error and 5% alpha error. It was a observational prospective (cross sectional) type of study.Inclusion criteria:1. All the newly diagnosed type 2 diabetes mellitus (with in 1 month) patients according to ADA recommendations [9] with age more than 18 years and had given consent for participation in the study.ADA Diagnostic criteria of type 2 Diabetes include:• FBS ≥ 126 mg/dL.• 2 hr. plasma glucose ≥200 mg/dL during an OGTT.• RBS ≥200 mg/dL with symptoms (polyuria, polydipsia, weight loss).• HbA1C >6.5%.Exclusion Criteria: Patients with the following diseases were excluded from the study.• Ischaemic heart disease. • Hypertensive heart disease. • Congestive heart failure. • Valvular heart disease. • Cardiomyopathy. • Renal failure. • Thyroid dysfunction • Chronic pulmonary illness• Severe anaemiaDetailed history was taken and examination of all the participants included in the study was done.The following investigations were done in all the patients included under study:• HbA1C levels• Transthoracic EchocardiographyDoppler Echo was done in each patient and 3-4 cardiac cycles were analysed to get best phase for better outcome of results. In Doppler Echo Study, following values were measured:1. E-peak velocity of early mitral flow (N: 50-90 cm/sec). 2. A-peak velocity of late mitral flow (N: 30-70 cm/sec). 3. E/A ratio (N: 1-2). 4. Left atrial size (N: 3–4 cms). 5. EF (N: >60%). (E: peak velocity across mitral valve during early diastolic rapid filling phase, A: peak velocity across mitral valve during late diastole/ atrial contraction phase)LV diastolic dysfunction was measured according to recommendation of American Society of Echocardiography (ASE). [10] The following criteria were considered as the evidence of left ventricular diastolic dysfunction. 1. Reduction in peak velocity of early mitral flow (E) increase over peak velocity of late mitral flow (A) with E/A ratio of <1 and2. Increase in Left Atrial (LA) size with preserved ejection fraction STATISTICAL ANALYSIS:Data obtained was entered into Microsoft excel data sheet and was analyzed using SPSS 22 version software. Categorical data were represented in the form of frequencies and proportions. Chi -square was used as test of significance for categorical data. Continuous data was represented as mean and standard deviation. Independent t test was used as test of significance to identify the mean difference between two groups i.e. group with LVDD and group without LVDD. p value <0.05 was considered as statistically significant [11].
4. Observations and Results
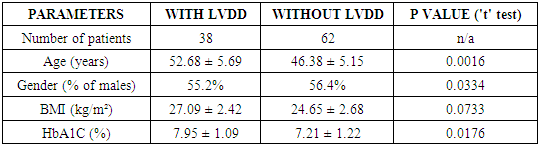
- Total 100 patients of newly diagnosed type 2 diabetes mellitus were selected for this cross sectional study. 56 out of 100 participants (56%) were males and 44 (44%) were females. Age of the patients was between 42 to 58 yrs, with mean age being 52 years. Among the study population, 38 patients had LVDD whereas 62 patients did not had LVDD.
|
 | Figure 1. Distribution of various parameters among patients with and without LVDD |
|
5. Discussion
- Diabetes Mellitus is a metabolic disease, associated with a number of complications including retinopathy, nephropathy, neuropathy, ischemic heart disease, cerebrovascular disease and peripheral vascular disease. Among these, most common cause of mortality among diabetic patients is cardiac involvement. In 1974, Framingham study showed that heart failure was more common in diabetes due to diabetic cardiomyopathy. Left ventricular diastolic dysfunction represent the first stage of diabetic cardiomyopathy preceding changes in systolic function. In this study, we assessed the correlation of left ventricular diastolic dysfunction (LVDD) with glycosylated haemoglobin (HbA1C).In our study, incidence of left ventricular diastolic dysfunction in Type 2 diabetics without known hypertension, cardiac, cerebrovascular or peripheral vascular disease was 38%. Similar study done by Somaratne et al [12] showed the similar prevalence. Another study done by Dawson et al [13] in UK found a very high prevalence of 74% which may be because they included already diagnosed cases of type 2 DM along with newly detected diabetics. Left ventricular diastolic dysfunction which is an ominous prognostic sign and independent risk factor for cardiac events is often present in type 2 diabetes mellitus patients. The possible contribution of hyperinsulinemia and hyperglycemia to left ventricular mass have been suggested in normotensive diabetic patients [14]. But there are less studies on glycated haemoglobin being the predictor of LVDD. In this study a positive correlation was found between prevalence of LVDD and level of HbA1C and Age but association with BMI and gender was not significant. Such positive correlation was also shown in other similar studies. [15, 16]
6. Conclusions
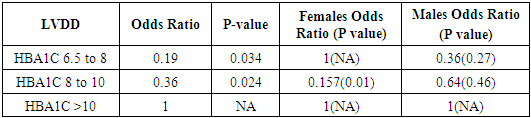
- In our study, around one-third of study population had LVDD.As poor glycaemic control can be associated with LVDD, the objective of the present study was to assess the correlation of HBA1C levels with left ventricular diastolic dysfunction in newly diagnosed Type 2 diabetic patients. Analysis of the data obtained from the study showed that patients with HBA1C between 8 to 10 have double the chances to develop LVDD than with HbA1c between 6.5 to 8; and patients with HBA1C more than 10 have five times the chances to develop LVDD than with HbA1C 6.5 to 8. This signifies that higher the value of HbA1C at the time of diagnosis, higher will be the incidence of LVDD in diabetic patients i.e, diastolic dysfunction is common in patients whose diabetes is not well controlled. Hence the present study suggests that HbA1c level is positively associated with the incidence of LVDD in diabetic population. Thus the objective of the study has been achieved. Correlation between gender and BMI with the incidence of LVDD in diabetic population was not noted in the study. The data provide a simple and practical approach in identification of LVDD in diabetic patients using their HbA1C levels. Limitations of our study are though we have considered newly diagnosed diabetics as in whom diabetes was diagnosed within one month, due to prolonged asymptomatic period of type 2 diabetes, we cannot accurately know duration for which patient had been diabetic. Furthermore, the sample size in our study is small, which is the other limitation. Therefore, the present results may not be readily represent the general population. Hence, more studies should be conducted to establish relationship between these two parameters.Our study recommends that as around one third of diabetic patients were found to have LVDD, screening the diabetic patients for LVDD at regular intervals using should 2D echo cardiography can identify the early changes of diastolic dysfunction before a person has symptomatic diastolic heart failure. Patients with elevated HbA1c can be a target population for screening of LVDD.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML