-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2015; 4(1): 9-13
doi:10.5923/j.ijim.20150401.02
Corelation between the Endoscopic and Histologic Diagnosis of Gastritis at the Ekiti State University Teaching Hospital, Ado Ekiti, Nigeria
Akande Oladimeji Ajayi1, Ebenezer Adekunle Ajayi1, Olusoji Abidemi Solomon2, Babatunde Duduyemi3, Emmanuel Abidemi Omonisi3, Olufemi Joshua Taiwo3
1Department of Medicine, College of Medicine, Ekiti State University, Ado-Ekiti, Nigeria
2Department of Family Medicine, Ekiti State University Teaching Hospital, Ado-Ekiti, Nigeria
3Department of Anatomic Pathology, College of Medicine, Ekiti State University, Ado-Ekiti, Nigeria
Correspondence to: Akande Oladimeji Ajayi, Department of Medicine, College of Medicine, Ekiti State University, Ado-Ekiti, Nigeria.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
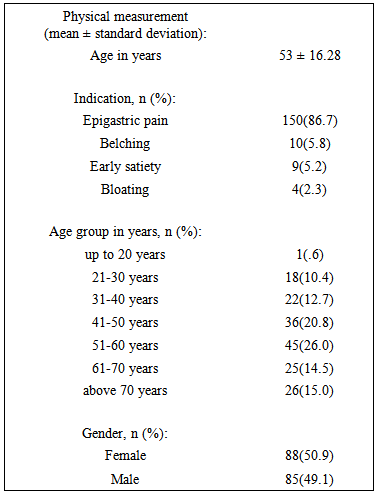
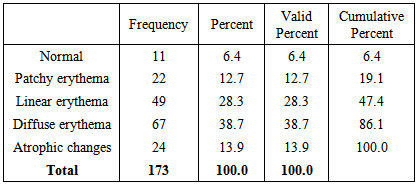
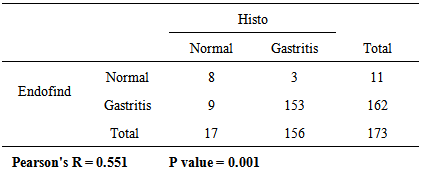
AIM AND OBJECTIVE: Endoscopists make judgements on the presence or absence of gastritis on the basis of endoscopic appearances of the gastric mucosa. Most studies in literature have shown poor concordance between endoscopic and histologic diagnosis of gastritis with concordance rates of between 54-63%. The aim of this study was to evaluate the rate of concordance between endoscopic and histologic diagnosis of gastritis at our facility given the variable but generally poor concordance reported in literature.MATERIALS AND METHODS: One hundred and seventy three consecutive patients who underwent upper gastrointestinal endoscopy and biopsy for dyspepsia at Ekiti State University Teaching Hospital (EKSUTH), Ado Ekiti, Nigeria were recruited into this study. Ethical approval for the study was obtained from the hospital’s Research and Ethics Committee and all the patients gave their individual written consent. RESULTS: The mean age of the studied population was 53.02±16.28 years (age range 17-87 years). Epigastric pain was the main (86.7%) indication for referral for upper gastrointestinal endoscopy, distantly followed by belching (5.8%), early satiety (5.2%) and bloating (2.3%) respectively. At endoscopy; diffuse erythema was found in 38.7% (67/173), followed in the descending order by linear erythema in 28.3% (49/173), atrophic gastritis in 13.9% (24/173), patchy erythema in 12.7% (22/173) respectively and normal findings in 6.4% (11/173). At histology; superficial chronic active gastritis was the most common findings 74.6% (129/173) of the patients, followed by chronic atrophic gastritis 15.6% (27/173) and normal findings in 9.8% (17/173). Of the 162 that were endoscopically diagnosed as gastritis, 153 were histologically confirmed (concordance rate of 94.4%). Also, of the 156 histologically diagnosed as gastritis, 153 were endoscopically diagnosed (concordance rate of 98.1%). In all, 153 of the 173 patients were both endoscopically and histologically diagnosed as gastritis (concordance rate of 88.4%). 76.3% (119 /156) of those that were diagnosed as gastritis histologically were found to be H.pylori associated gastritis.CONCLUSIONS: In conclusion, endoscopy is a reliable predictor of histological gastritis in a population with a severe form of gastritis. We equally agreed with other authors that histology is the goal standard and mandatory for accurate diagnosis of gastritis in all cases.
Keywords: Endoscopy, Histology, Gastritis, Concordance
Cite this paper: Akande Oladimeji Ajayi, Ebenezer Adekunle Ajayi, Olusoji Abidemi Solomon, Babatunde Duduyemi, Emmanuel Abidemi Omonisi, Olufemi Joshua Taiwo, Corelation between the Endoscopic and Histologic Diagnosis of Gastritis at the Ekiti State University Teaching Hospital, Ado Ekiti, Nigeria, International Journal of Internal Medicine, Vol. 4 No. 1, 2015, pp. 9-13. doi: 10.5923/j.ijim.20150401.02.
1. Introduction
- Endoscopists and Gastroenterologists make judgements on the presence or absence of gastritis on the basis of the endoscopic appearance of the gastric mucosa. The concept of “endoscopic gastritis” was given acknowledgement by the working party that formulated the Sydney System of classifying gastritis (endoscopic division) [1].Most studies in literature have shown poor concordance between endoscopic and histologic diagnosis of gastritis with concordance rates of between 54-63% [2-4]. Very few studies however, have found good concordance with one in particular reporting a concordance rate of about 97% [5-6]. In the severe forms of gastritis, concordance is said to be good and that a normal endoscopy may actually excludes active gastritis [2, 7].The aim of this study was to evaluate the rate of concordance between endoscopic and histologic diagnosis of gastritis at our facility given the variable but generally poor concordance reported in literature.
2. Materials and Methods
- Study location: This study was carried out at the Ekiti State University Teaching Hospital (EKSUTH), Ado-Ekiti, Nigeria from January 2012 to December 2013.Study population: One hundred and seventy three consecutive patients who underwent upper gastrointestinal endoscopy for dyspepsia were recruited into this study.Study type: This is a cross sectional prospective study.Inclusion and exclusion criteria: All patients aged 16 years and above with signs and symptoms of dyspepsia were included in the study, while patients who refused endoscopy or their medical condition precluded a satisfactory endoscopic examination were excluded.Data collection: The followings were extracted from the patients or the relations: age, gender, use of aspirin or NSAIDS, alcohol ingestion, use of native concoctions, heamatemesis, melena, haematochezia, presenting signs and symptoms. Endoscopic findings and histologic reports were documented. Methods and procedure: Upper gastrointestinal endoscopy was performed using Olympus EVIS GIF-140 under xylocaine anaesthetic spray of the oropharynx and where necessary with midazolam after an overnight fasting with the patient on the left lateral position. All the endoscopies were performed by a single trained Endoscopist who formed a global impression on the presence or otherwise of gastritis in the antrum of the stomach. Three gastric biopsies were taken from the antrum using a standard 7 FG sized biopsy forceps. All the biopsies were taken from the perceived “inflamed” areas and fixed immediately in 10% formalin. Endoscopic gastritis was classified according to the Sydney system [1] taking into consideration the following components oedema, punctate and confluent erythema, friability, punctate and confluent exudate, flat and raised erosions, rugal hyperplasia and atrophy, visibility of the vascular pattern, punctate and confluent intramural bleeding spots, and fine and coarse nodularity. The endoscopic appearances of the antrum were documented. The biopsies were cut into sections and stained with the routine Haematoxylin and Eosin (H & E) and also with Giemsa stain. The slides were assessed histologically by three Gastrointestinal Pathologists at different times and were blinded to the endoscopic features of the patients. The histological assessment was in accordance with the criteria described by the Sydney classification System (histologic division) [1, 8], which includes a subjective assessment of severity as mild, moderate or severe, and then classified into one of the following eight categories: erythematous/ exudative gastritis, atrophic gastritis, raised erosive gastritis, flat erosive gastritis, haemorrhagic gastritis, rugal hyperplastic gastritis, enterogastric reflux gastritis, and congestive gastroenteropathy.Ethical clearance: Ethical approval for the study was obtained from the hospital’s Research and Ethics Committee and all the patients gave their individual written consent. Statistical analyses: SPSS version 15.0 (SPSS, Inc., Chicago, Illinois, USA) was deployed for statistical analysis using the t-test for quantitative variables and χ2 test for qualitative variables. Differences were considered to be statistically significant if P value was less than 0.05.
3. Results
- The male: female ratio was 1:1. The mean age of the studied population was 53.02±16.28 years (age range 17-87 years). Majority of the patients were in the age group 31-60 years (Table 1). Epigastric pain was the main (86.7%) indication for referral for upper gastrointestinal endoscopy, distantly followed by belching (5.8%), early satiety (5.2%) and bloating (2.3%) respectively (Figure 1).
|
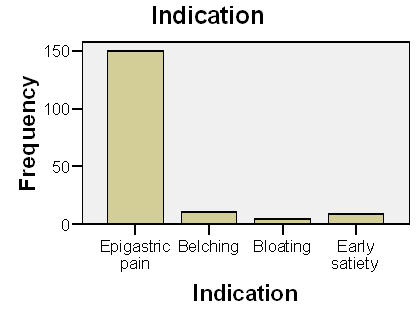 | Figure 1. Showing the indications for endoscopy |
|
|
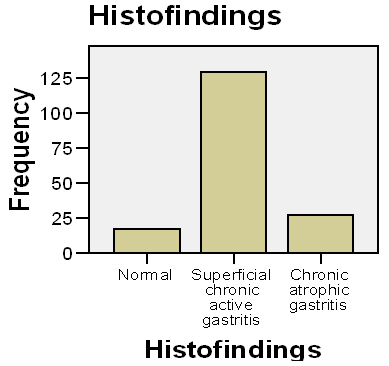 | Figure 2. Showing the various histological findings |
4. Discussion
- The Sydney classification of endoscopic gastritis [1] aims to standardize reporting by classifying endoscopic gastritis into seven categories, based on 15 endoscopic mucosal features: oedema, punctate and confluent erythema, friability, punctate and confluent exudate, flat and raised erosions, rugal hyperplasia and atrophy, visibility of the vascular pattern, punctate and confluent intramural bleeding spots, and fine and coarse nodularity. It also re-categorizes portal hypertensive gastropathy as congestive gastroenteropathy. This study was devised to correlate the endoscopic features described by the Sydney system with the histological findings.Diffuse erythema was the commonest type of gastritis diagnosed endoscopically in this study 38.7% (67/173) while on the other hand; superficial chronic active gastritis was the most common histological diagnosis 74.6% (129/173). Of the 173 patients, 153 were diagnosed as gastritis both endoscopically and histologically giving a concordance of 88.4%. While a number of studies in literature have shown abysmal or poor concordance between endoscopic and histologic diagnosis of gastritis with concordance rates of between 54-63% [2-4, 9-13], a high concordance obtained in this study is similar to the 97% concordance obtained by Fung et al [5] and Zubair et al [6]. This might be due to the fact that most of our patients had severe forms of gastritis at the time of their presentation. Late presentation is the most common form of presentation of diseases in the third or under developed worlds. Studies have equally shown that concordance between endoscopy and histology may be good in the severe forms of gastritis [1] and that a normal endoscopy may in actual fact excludes active gastritis [7]. High resolution magnifying endoscopy has been shown to have a better correlation with histologic findings and might indeed allow definitive diagnosis of gastritis to be made without the need for biopsy [14-15]. Similar conclusions have been reached for duodenitis [11, 16].Out of the eleven that were found to be normal endoscopically, eight were confirmed to be histologically normal while the remaining three were diagnosed as superficial chronic active gastritis. This observation was similar to the findings in the study of Gad [17].Of the 22 diagnosed endoscopically as patchy erythema, 13 were histologically found to have gastritis (concordance of 59%). This findings support the studies that found poor concordance in mild forms of gastritis showing the insensitivity of endoscopy in diagnosing gastritis in the mild forms of gastritis. Endoscopically in this study, 80.9% (140/173) of the patients had severe forms of gastritis and all these patients had gastritis histologically. This finding is in keeping with the studies of Tytgat [1], and Toukan et al [7]. This might be due to the high prevalence of H.pylori infection in the third world countries. 93.6% of our study population had one form of gastritis or the other at endoscopy; this was in contrary to the 62.1% obtained by Jemilohun et al [18] in a similar population study. Again, this might be due to fact that most of our patients had severe forms of gastritis at the time of their presentation. 90.1% of our patients had histologically diagnosed gastritis similar to the 96.6% found by Jemilohun et al [18]. 88.4% of our patients were both endoscopically and histologically diagnosed as gastritis compared to the 60.9% in the Jemilohun et al study [18]. The prevalence of H.pylori associated gastritis in this study was 73.6% while the overall prevalence among the studied population was 68.8%. This is consistent with results of previous studies conducted in Nigeria and other parts of West Africa which have consistently shown a high prevalence of H. pylori with the use of biopsy based methods [19-24].In conclusion, endoscopy is a reliable predictor of histological gastritis in a population with a severe form of gastritis. We equally agreed with other authors that histology is the goal standard and mandatory for accurate diagnosis of gastritis in all cases.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML