-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2014; 3(2): 35-37
doi:10.5923/j.ijim.20140302.03
Cardiomyopathy due to Pegylated Interferon Therapy for Hepatitis C
Punita Kaveti, Erica T. Isom, Kelly Schrapp, Marvin Crawford
Department of Internal Medicine, Morehouse School of Medicine, Atlanta, USA
Correspondence to: Punita Kaveti, Department of Internal Medicine, Morehouse School of Medicine, Atlanta, USA.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Pegylated interferon is an important drug in the treatment of Hepatitis C. Cardiomyopathy due to interferon is rare but can be fatal. With increasing incidence of hepatitis C, more patients are being treated with Interferon based therapy. We report a case of 53 year old man who presented with new onset congestive heart failure within 11 weeks of starting triple therapy with pegylated interferon for Hepatitis C infection. Patient had a remote history of cocaine, alcohol, tobacco use, family history of coronary artery disease, congestive heart failure but he never had a previous cardiac work up. We suggest getting a baseline Echocardiogram in patients who are at high risk for cardiomyopathy before starting interferon therapy.
Keywords: Interferon induced cardiomyopathy, Hepatitis C therapy, Cardiomyopathy
Cite this paper: Punita Kaveti, Erica T. Isom, Kelly Schrapp, Marvin Crawford, Cardiomyopathy due to Pegylated Interferon Therapy for Hepatitis C, International Journal of Internal Medicine, Vol. 3 No. 2, 2014, pp. 35-37. doi: 10.5923/j.ijim.20140302.03.
1. Introduction
- With the new USPSTF guidelines released on June 2013, recommending screening for hepatitis C virus (HCV) infection in persons at high risk for infection and to those born between 1945 and 1965 [1], more number of patients are being diagnosed with hepatitis C and are being treated with Triple therapy for Chronic Hepatitis C infection. Interferon related cardiotoxicity although rare has been reported in the literature in the past. We report a case of a patient who failed dual therapy and was on triple therapy for hepatitis C, who presented with new onset CHF which was attributed to interferon as the work up for other causes was negative. In this article we want to highlight the cardiac side effects of interferon therapy and also suggest getting a baseline Echocardiogram to assess left ventricular systolic function, especially in high cardiac risk patients prior to starting interferon therapy.
2. Case Description
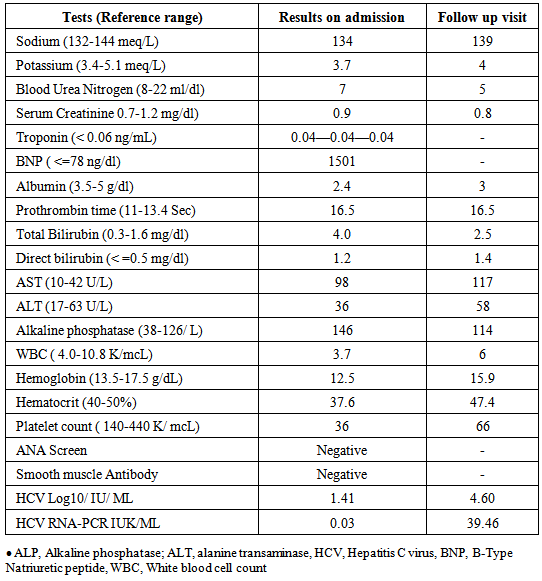
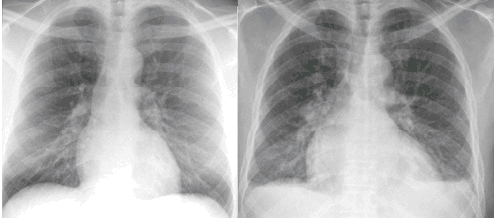
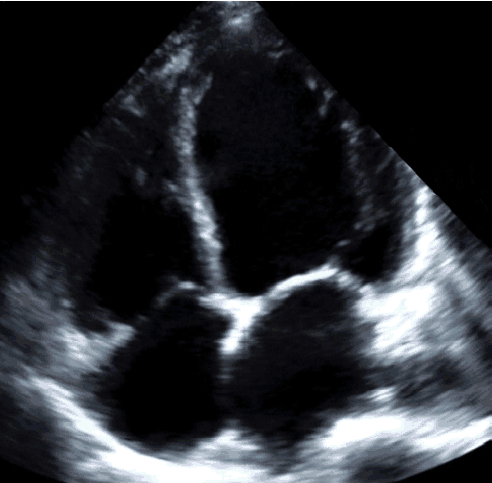
- A 53 year old male with chronic hepatitis C presented with worsening shortness of breath for 2 weeks. He also endorsed early satiety, decreased exercise tolerance, paroxysmal nocturnal dyspnea, orthopnea associated with nocturnal productive cough and bilateral lower extremity swelling. Patient has cirrhosis secondary to chronic hepatitis C, null responder to dual therapy in the past, was on 11/48 weeks of triple therapy consisting of pegylated interferon, ribavirin, and telaprevir. Prior to this presentation, patient did not have any significant cardiac history. Other significant history included cocaine, alcohol and tobacco abuse, quit more than 23 years ago and family history of heart failure and coronary artery disease. His vitals were normal on presentation. On examination, he had jugular venous distension up to the jaw, with decreased breath sounds at the lung bases with crackles on the right side, 2+ pitting edema of both lower extremities. Laboratory results are shown in Table 1. ECG showed sinus rhythm with heart rate 82, diffuse T wave inversion in all the leads, borderline prolonged QTC interval, no acute ST-T wave changes suggestive of ischemia. Chest X-ray (Figure 1) showed cardiomegaly with pulmonary edema and new small bilateral pleural effusion. Three sets of cardiac enzymes were negative. BNP was 1501. Echocardiogram (Figure 2) showed nonspecific cardiomyopathy with moderately dilated left and right ventricles and atria, severe global hypokinesis of left ventricle (LV) with estimated ejection fraction of 10-15%, with Stage 2 LV diastolic dysfunction. Ischemia work up with Nuclear medicine cardiac stress test did not show any evidence of stress induced myocardial ischemia. ANA panel, smooth muscle antibody test were negative. HCV viral load was low.
 | Figure 1. Left side: CXR from 8 months prior to presentation showing normal cardiac silhouette. Right side: CXR showing cardiomegaly taken at presentation |
 | Figure 2. Echocardiogram with Apical 4 Chamber view showing Dilated cardiomyopathy |
|
3. Discussion
- Hepatitis C infection is one of the most common viral infections worldwide which can be cured. In a quarter of a century, the percentage of cure has increased from 6% to 90%, with pegylated interferon in triple therapy increasing cure in 70-80% of cases [2]. Common side effects of interferon therapy are irritability, insomnia, fatigue, loss of appetite, depression [2]. Cardiac toxicity due to interferon therapy is rare and presents as arrhythmia, myocarditis, reversible hypertension, ischemic heart disease, pericarditis, pericardial effusion and rarely cardiomyopathy [3-6]. The mechanism of interferon induced cardiomyopathy is not known. Sonnenblick et al; suggest that cardiomyopathy was induced through impaired myocyte metabolism rather than through histological damage [3]. To the best of our knowledge, ours is the fifth case reporting cardiomyopathy associated with pegylated interferon therapy for Chronic Hepatitis C. As per literature, most cases with interferon related cardiomyopathy had improved left ventricular function within 1-2 months after cessation of interferon therapy. However pegylated interferon related cardiomyopathy showed a poor prognosis [7]. In our patient, cardiac function was still low inspite of being on appropriate therapy for 6 months. Although our patient had multiple risk factors that could have caused cardiomyopathy like Hepatitis C infection per se, alcohol and cocaine use ( remote > 15 years back), family history of congenital heart disease, he did not have any prior cardiac work up which would have helped us compare his LV function before and after therapy. Due to increased number of people getting pegylated interferon related therapy for hepatitis C, we suggest getting a baseline echocardiogram in all patients, especially high cardiac risk patients prior to starting interferon therapy. Emanuele Durante-Mangonia et al; report that treatment with pegylated interferon/ribavirin may be safely offered to carefully selected chronic hepatitis C patients with coexisting, clinically significant heart disease [8]. However, clinicians should be aware of interferon related cardiac toxicity and monitor for cardiac symptoms in the patients to detect early cardiac toxicity, so that therapy can be aborted before irreversible cardiac damage occurs and those patients can be good candidates for interferon free regimen.
4. Conclusions
- Pegylated interferon is an important medication used for treatment of hepatitis C. Cardiac function needs to be monitored in patients on interferon therapy. We recommend a baseline echocardiogram to assess Left ventricular systolic function prior to starting interferon therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML