-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2013; 2(3): 20-22
doi:10.5923/j.ijim.20130203.02
Case Report: Anemia with Jaundice throughout Acute Hemolysis, Transaminasemia and Systemic Lupus Erythematosus (Sle) with Autoimmune Hemolytic Anemia (Aiha)
Azreen Syazril Adnan1, Mohammad Salman2, Amer Hayat Khan2, Siti Maisarah Sheikh Ghadzi2, Ahmad Shahir Yusof2, Syamimee Wan Ghazali3
1Chronic Kidney Disease (CKD) Resource Center, School of Medical Sciences, University Science Malaysia, Kota Bharu, 16150, Kelantan, Malaysia
2Department of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, 11800 Penang, Malaysia
3Medical Departments, Hospital Universiti Sains Malaysia, Kota Bharu, 16150, Kelantan, Malaysia
Correspondence to: Azreen Syazril Adnan, Chronic Kidney Disease (CKD) Resource Center, School of Medical Sciences, University Science Malaysia, Kota Bharu, 16150, Kelantan, Malaysia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
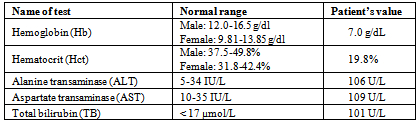
A 32-year-old Malaysian woman was admitted to Hospital University Science Malaysia (HUSM) in May 2013 with complains of discoloration of scleras and passing out tea colored urine for 2 days. She had the history of systemic lupus erythematosus (SLE) with autoimmune hemolytic anemia (AIHA) and was steroid dependent. On admission, she was alert, conscious and afebrile. Laboratory investigations revealed alanine transaminase (ALT), aspartate transaminase (AST) and total bilirubin (TB) levels elevation, decreased level of hemoglobin (7.0 g/dl) and non-reactive Australian antigen (HBsAg) and Anti-HCV antibodies. Chest radiograph showed no pulmonary edema, pleural effusion and cardiomegaly. A diagnosis of anemia with jaundice throughout acute hemolysis, transaminasemia and SLE and AIHA was made. She was administered Prednisolone 5mg once daily and Cyclosporine 200mg twice daily after which serum levels of ALT and AST and TB were decreased to within normal range. We conclude that this is a unique case of anemia with jaundice with acute hemolysis, transaminsemia and SLE with AIHA.
Keywords: Systemic Lupus Erythematosus, Anemia, Jaundice, Autoimmune Hemolytic Anemia
Cite this paper: Azreen Syazril Adnan, Mohammad Salman, Amer Hayat Khan, Siti Maisarah Sheikh Ghadzi, Ahmad Shahir Yusof, Syamimee Wan Ghazali, Case Report: Anemia with Jaundice throughout Acute Hemolysis, Transaminasemia and Systemic Lupus Erythematosus (Sle) with Autoimmune Hemolytic Anemia (Aiha), International Journal of Internal Medicine, Vol. 2 No. 3, 2013, pp. 20-22. doi: 10.5923/j.ijim.20130203.02.
1. Introduction
- Systemic lupus erythematosus (SLE) is an autoimmune disorder that affects skin, joints, kidneys, brain and other organs, which lead to chronic inflammation[1]. SLE is most common in women age less than 50 years than men[1, 2]. The prevalence of SLE was found to be 124 cases per 100,000 persons and incidence of SLE varies among ethnic groups with the annual incidence in adults ranging from 1.9-5.6 per 100,000 persons per year[3]. The 5- year survival rate exceeds 96% and 20-year survival rates approach 70%[4]. Hematological manifestations of SLE are thrombocytopenia and anemia which is mostly due to chronic disease or autoimmune hemolytic anemia and hypoblastic anemia[5]. SLE can affect the liver in several ways (hepatomegaly, jaundice, Budd-chiari syndrome, hepatitis, ascites and many others) and 25-50% SLE patients have abnormal liver function tests in their lifetime[6]. Jaundice is a yellow discoloration of skin and sclerae caused by increase of bilirubin in serum due to break down of hemoglobin[7]. This can lead to changes of urine color to be dark yellow or brown. The common cause of jaundice is the hemolytic anemia. As previously discussed, the red blood cell or hemoglobin content in the body is reduced because destruction rate of red blood cell is faster than bone marrow production. The SLE causes complication to the blood by incidence of autoimmune hemolytic anemia (AIHA). As a result, patients may have symptoms of jaundice.
2. Case Description
- A 32-year-old Malaysian female was admitted to Hospital University Sciences Malaysia (HUSM) in May 2013 with complains of yellowish discoloration of sclera and passing tea colored urine for 2 days. Patient denied itchiness during urination, pale stool and abdominal pain. Her body temperature was normal and it was day 2 of her menstrual cycle. Patient also denied smoking, alcohol and any drug addiction/abuse. She had history of Systemic lupus erythematosus (SLE) with autoimmune hemolytic anemia (AIHA) and she was steroid dependent. She also had history of thalassemia treatment. She was taking cyclosporine and prednisolone for the management of SLE with AIHA and Folate for thalassemia. Moreover, her past medical history was community acquired pneumonia and recurrent abortion due to isolated prolong activated partial thromboplastin time (aPTT).On admission, patient’s physical findings were blood pressure 143/79 mmHg; pulse rate 86 beats/minute, body temperature 37.3°C and saturating oxygen 100%. She was alert, conscious and non-tachypneic. Jaundice could be seen on both sclerae with mild paler. Lungs were clear, cardiovascular system showed normal rate and rhythm and there were no murmurs of S1 and S2, abdomen was soft, non-tender, non-distended and no hepatosplenomegaly. Chest radiograph showed that cardiac size was normal and there was no pulmonary edema and pleural effusion. Laboratory investigations revealed that she had elevated levels of alanine transaminase (ALT), aspartate transaminase (AST) and total bilirubin (TB), low level of hemoglobin. Hepatitis viruses antibodies were non-reactive. Her abnormal laboratory findings are given in table 1.
|
3. Discussion
- A study reported 23% of their 81 SLE patients had abnormal liver tests for which the cause was no other than SLE itself[8]. In another study of 365 patients suffering from SLE, 30% had abnormal liver function tests at the time of diagnosis[9]. During the admission, cyclosporine 200mg BD and prednisolone 5mg OD were administered for the treatment of SLE. Combinations of cyclosporine with corticosteroids have been the mainstays of immunosuppressive therapy. Although both are known to suppress and stabilize extrarenal disease activity, much of the evaluation of these agents has focused on lupus nephritis which is a major factor associated with morbidity and mortality in SLE. Cyclosporine is calcineurin inhibitor, acts by inhibiting the production and release of interleukin I and inhibits interleukin I-induced activation of resting T-lympocytes. The reference level of cyclosporine is 50- 400 µg/ml[10]. Although this patient had level of 500 µg/ml but it is still considered safe. After the treatment with cyclosporine and prednisolone patient’s AST, ALT and TB level reduced to within normal range.Hematological abnormalities are frequent in SLE and anemia can be found in 50% of the patients[11]. In SLE patients, the immune system of body become over reactive and cause hemolytic anemia. It is due to suppressed erythropoiesis from chronic inflammation (anemia of chronic disease/anemia of chronic inflammation). The anemia is normocytic and normochromic with a relatively low reticulocyte count. Although serum iron levels may be reduced, bone marrow iron stores are adequate and the serum ferritin concentration is elevated. During the admission, the patient was administered with folate tablets for treatment of anemia. According to a case report of SLE presenting with acute hepatitis and jaundice, patient’s serum level of AST and ALT were decreased after the administration of prednisolone 60mg/day[12]. In our case, patient was suffering from anemia with jaundice throughout acute hemolysis and SLE with AIHA but her condition was improved and liver tests became normal because of treatment with prednisolone and cyclosporine.
4. Conclusions
- Our patient had anemia with jaundice throughout acute hemolysis, transaminasemia and SLE with AIHA. The main disease was SLE which led to other complications. The Patient treatment was successful and her liver enzymes were normal at the time of discharge. Since our patient had the history of SLE and AIHA and thalassemia treatment, the abovementioned complications might occur due to non-compliance with therapy prescribed at home. Therefore, patient counseling and providing adequate information are very important in order to prevent the recurrence and also hospitalization.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML