-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2013; 2(3): 17-19
doi:10.5923/j.ijim.20130203.01
Insulin Dose and Hospitalary Stay in Patient with Acute Pancreatitis by Hypertriglyceridemia
Arnulfo González-Cantú1, José Luis Charles-González2
1Department of Endocrinology, Universitary Hospital “José E. González”, Monterrey Nuevo León, Post Code, 64460, México
2Department of Internal Medicine, General Hospital “Dr. Norberto Treviño Zapata”, Cd. Victoria Tamaulipas, Post Code, 87024, México
Correspondence to: Arnulfo González-Cantú, Department of Endocrinology, Universitary Hospital “José E. González”, Monterrey Nuevo León, Post Code, 64460, México.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
The aim of the study is do correlation between the insulin total dose and the hospitalary stay.We included all patients with acute pancreatitis by hypertriglyceridemia that were admitted in our hospital since 2008 to 2012. The information was recollected from the clinical archive. The inclusion criterion was considered a concentration of serum triglycerides greater than 1000mg/dl. We excluded patients with another causes of acute pancreatitis. The subjects were categorized by insulin dose (low, medium, high).Acute pancreatitis was more common in men within the fourth decade of life, and has risk factor of alcoholism and smoking. The severity scales shown that acute pancreatitis by hypertriglyceridemia was milder than other causes of pancreatitis. The insulin dose stayed in the range of 73 - 240 UI/day. Events of hypoglycemia were similar in the groups of low and medium insulin dose.The pancreatitis by hypertriglyceridemia was not severe than other kinds of acute pancreatitis, greater dose of insulin not improve the hospitalary stay.
Keywords: Acute Pancreatitis, Hypertriglyceridemia, Insulin Dose
Cite this paper: Arnulfo González-Cantú, José Luis Charles-González, Insulin Dose and Hospitalary Stay in Patient with Acute Pancreatitis by Hypertriglyceridemia, International Journal of Internal Medicine, Vol. 2 No. 3, 2013, pp. 17-19. doi: 10.5923/j.ijim.20130203.01.
Article Outline
1. Introduction
- Acute pancreatitis is an inflammatory process of pancreas[1] associated with hypertriglyceridemia in 1-4% of cases[2]. The risk rises when the serum levels of triglycerides are above of 1000mg/dl[2]. The increment of triglycerides could be caused by multiples etiologies like primary and secondary alterations of the lipids metabolism, alcoholism, diabetes mellitus and hypothyroidism[3].Lipoprotein lipase, a key piece in the lipids metabolism localized in vascular endothelium, degrades triglycerides to free fatty acids for its tissue using[4]. Taskinen MR et al.demonstrated that heparin and insulin increase lipoprotein lipase activity[5, 6]. Treatment based in activation of this enzyme has been suggested in severe hypertriglyceridemia cases. However, there is no evidence that intensive insulin therapy improves the intrahospitalary stay in pancreatitis by hypertriglyceridemia.Intravenous insulin therapy has the disadvantage risk of hypoglycemia, with direct proportional increase with dosage, needing more glucose solutions to keep euglycemia. The aim of our study was to determinate the correlationbetweeninsulin therapy and the hospitalary stay in patients with acute pancreatitis by hypertriglyceridemia.In addition we described the adverse outcomes of insulin treatment and other factors like initiation day of enteral feeding.
2. Subjects and Methods
- This retrospective, retrolective, descriptive study was performed in the Universitary Hospital “José E. González”. We included all patients with diagnosis of acute pancreatitis by hypertriglyceridemia since 2008 to 2012. The information was taken from the clinical records of the hospital.We included subjects with age between 18 to 65 years old, serum amylase mayor to three times over the normal range and serum triglycerides concentration above 1000mg/dl; and excluded the patients with other associated illness (myocardial infarction, stoke, pneumonia, acute hepatitis, uremic syndrome, etc), autoimmune disease, biliary cancer and any other possible etiology of acute pancreatitis (ej. cholecystolithiasis, alcohol ingestion). The characteristics of the patients included the admission status and severity scales at 48 hrs. (APACHE, SOFA and Ranson). The patients were categorized by insulin daily dose in: low (< 24 UI/day), medium (24 - 72 UI/day) and High (>72 UI/day). The results were expressed in average, and standard deviation (SD). We used independent samplet test for continues variables, Chi-square for dichotomic variables and Spearman´s correlation for theassociation variables. We used Medcalc 12.2.1.0 for statistical analysis.
3. Results
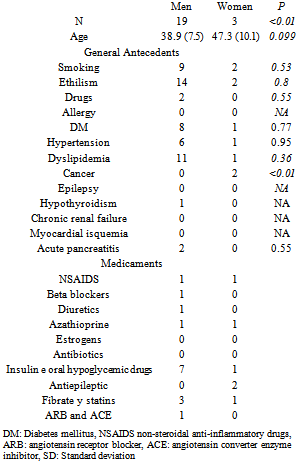
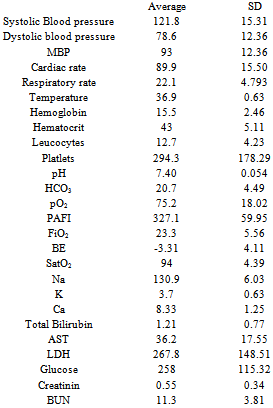
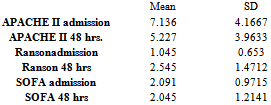
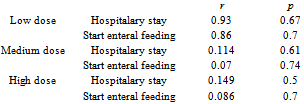
- Between 2008 to 2013, 22 patients were admitted in our hospital with diagnosis of acute pancreatitis by hypertriglyceridemia, only 3 cases were women. The general characteristics are shown in table 1. There was not any statistically difference in age between genders. In men, the risk factors for hypertriglyceridemia (smoking, alcoholism, dyslipidemia and previous diagnosis of DM) are more frequent than in women although there wasn´t any statistical difference between genders. Table 2 describes the subjects characteristics in their admission. The mean blood pressure was 93 mmHg (± 12.36 SD). In average, the patients had a slight hypoxemia with 94% oxygen saturation in room air. No subject had a cholestasis pattern in the liver function test or acute renal failure. The severity scales showed no severe pancreatitison admission and 48 hours after, table 3. The average daily insulin dose was 73 UI/day (±57.4). The low insulin dose group counted with only one subject; medium insulin dose group included 15 subjects and 6 subjects formed the high dose of insulin group. We only analysed the association among the last 2 groups with the hospitalary stay and the start of the enteral feeding were we did not find any statistic correlation, table 4.
|
|
|
|
4. Discussion
- Acute pancreatitis by hypertriglyceridemia is not a frequentetiology of abdominal pain, wehad only 22 cases in five years. Its thought that this etiology is more severe than other causes of pancreatitis, however, in our study the cases were mild. This is supported by the fact that none had distributive shock, acute pulmonary injury or multiorganic failure.In this study although there was no statistically difference between genders,in raw the man had more risk factors forhypertriglyceridemia than women. There is a limitation in women sample size Standard treatment of pancreatitis by hypertriglyceridemia includes general support, fast and intravenous insulin with a dose range of .1 to .3 UI/kg/hr[2]. This last indication must be followed by stretch evaluation of glycemia and it necessary requires glucose solutions to preventhypoglycaemia. Clinically this can bring excessive hydration and a higher incidence of hypoglycaemia. In our study the severity of hypoglycemia were major in the higher dose group, supporting that more insulin does not improve the hospitalary stay, but increase the severity of complications.We didn´t found a correlation between the hospitalary stay and the insulin dose, probablybecause this intervention is useful to eliminate the precipitating factor(hypertriglyceridemia) but not to enhance the outcomethat is dependent of the severity of inflammation caused by the pancreatitis.In the review of medical literature we didn´t found another study that correlated the insulin dose with the outcome of hospitalary stay and the enteral feeding. Although we still have concerns with the patients with recurrent hypertriglyceridemia after the initiation of enteral feeding and the better time to discharge this patients.
5. Conclusions
- Acute pancreatitis by hypertriglyceridemia is an infrequent event with not necessary major severity than other pancreatitis. There´s no association between insulin dose and hospitalary stay, thus, our recommendation is not to give more insulin than the necessary to keep the euglycemia. The beginning of enteral feeding neither had association with the insulin dose. The severity of hypoglycemia is higher as the amount of insulin administrated.
ACKNOWLEDGEMENTS
- We acknowledge to Dr. Alfonso Zapata-Garridoand Dra. María Elena Romero-Ibarguengoitiafor his support on the analysis and the Department of Clinical archives for his cooperation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML