-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2013; 2(2): 7-10
doi:10.5923/j.ijim.20130202.01
Defecation Syncope – A Poorly Described Phenomenon that should not be at the ‘Bottom’ of Your Differential
Paul C. Hertz1, Kenneth G. Gin2
1Internal Medicine Department, University of British Columbia, Vancouver, Canada
2Department of Cardiology, University of British Columbia, Vancouver, Canada
Correspondence to: Paul C. Hertz, Internal Medicine Department, University of British Columbia, Vancouver, Canada.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Syncope is widespread and responsible for three to five percent of US emergency room visits. While clear cardiac or orthostatic factors are identified in a majority of cases, situational syncope is infrequently described in the literature despite case reports dating back to the early 20th century. Here we present a case of an 84 year old with recurrent hypotension and bradycardia related to defecation. We hope to expand the knowledge around this subject and enhance earlier recognition and treatment.
Keywords: Syncope, Defecation, Micturation, Autonomic Failure
Cite this paper: Paul C. Hertz, Kenneth G. Gin, Defecation Syncope – A Poorly Described Phenomenon that should not be at the ‘Bottom’ of Your Differential, International Journal of Internal Medicine, Vol. 2 No. 2, 2013, pp. 7-10. doi: 10.5923/j.ijim.20130202.01.
1. Introduction
- Syncope is a widespread phenomenon with an incidence between three and six percent over 10 years[1] and is responsible for three to five percent of US emergency room visits[2]. While clear cardiac factors (including arrhythmias and valvular disease) or orthostatic factors (including drugs and hypovolemia) are identified in a majority of cases many times the cause is not ultimately obvious. Vasovagal syncope, or carotid hypersensitivity, is a common cause of syncope. However, situational syncope is not as well described. Typical triggers include any actions that cause a Valsalva response (expiring against a closed glottis)[3] and include coughing, swallowing, micturation and defecation. While well known, with case reports dating back to the early 20th century[4], defecation syncope is infrequently described in the literature.
2. Case Presentation
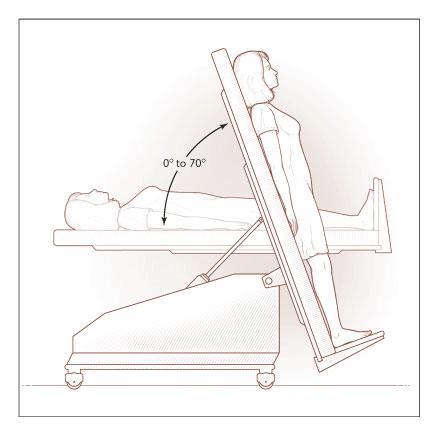
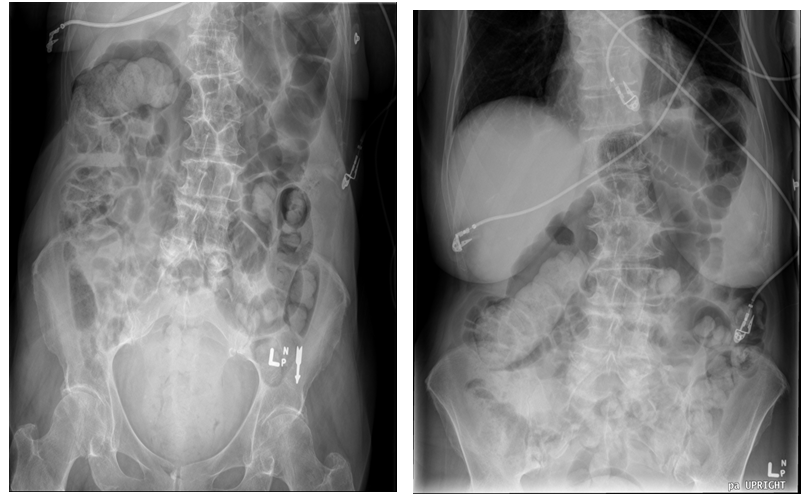
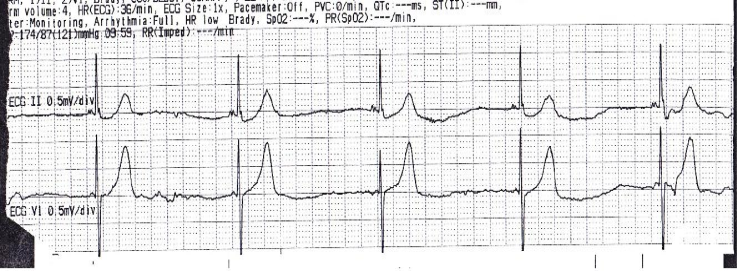
- Here we present a case of an 84 year old woman with coronary artery disease, hypertension and hyperlipidema, presented to the emergency department after a syncopal event. She had no history of diabetes mellitus or thyroid disease. A recent Echo showed normal biventricular function. She lived independently. She had been complaining of significant constipation and was, in fact, at a drug store buying a laxative when she felt unwell, went to the bathroom and had a syncopal event while straining.On her arrival she felt well and had little recall of the event. She denied angina, dyspnea, palpitations or infectious symptoms. She did not appear post-ictal. Her blood pressure was 197/78, her pulse was 78 and regular and her oxygen saturation of 98% on room air. There was no significant postural change in her blood pressure or pulse upon standing. She was in no distress. The remainder of her physical exam revealed abdominal fullness and significant hard stool in her rectal vault. Bloodwork demonstrated normal troponin, TSH and fasting glucose. Her medications at home included: metoprolol 25 mg orally twice daily, hydralazine 12.5 mg orally three times daily, felodipine 10 mg once daily, ramipril 5 mg orally twice daily, ASA 81 mg orally once daily and simvastatin 40 mg orally once daily. All doses had been stable for several months. Her blood pressure had been somewhat difficult to control, evidenced by the fact that she was on four different anti-hypertensive agents. ECG obtained in the emergency department showed normal sinus rhythm. Abdominal x-ray revealed large amounts of stool throughout her colon from the rectum to the hepatic flexure “Figure 1”. There were no signs of obstruction and no masses. Upon stimulation with an enema, the patient promptly became bradycardic (heart rate of 36; “Figure 2”) and hypotensive (blood pressure of <80 mmHg systolic) requiring treatment with intravenous fluids and atropine.The patient was admitted to the Cardiac Care Unit for cardiac monitoring. During her admission she experienced several further episodes of presyncope while straining to pass bowel movements (see “Figure 3”). An aggressive bowel protocol was initiated (with the exemption of any enemas). Due to the difficulty in resolved our patient’s constipation, a computed tomography scan of her abdomen and pelvis was ordered to rule out any obstruction. The CT confirmed severe constipation with dilation of her colon (maximum diameter 9.5 cm). There were no masses or signs of obstruction.
 | Figure 1. An abdominal X-rays of our patient showing significant fecal loading throughout the colon |
 | Figure 2. A rhythm strip demonstrating marked sinus bradycardia with a rate of 36 beats per minute |
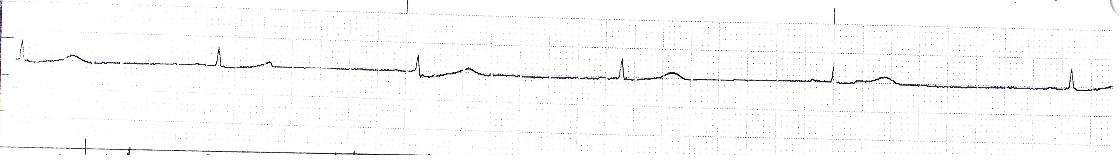 | Figure 3. A subsequent episode of bradycardia which occurred during this patient’s admission to the Cardiac Care Unit |
3. Discussion
- Neurocardiogenic syncope is common in the general population with a prevalence of up to 3-3.5%[5]. It has a bimodal distribution with peaks in the early teens and the 8th decade of life. The differential diagnosis is large and includes all types of syncope with etiologies including (but not limited to) valvular heart disease, arrhythmias, thromboembolic events, hypovolemia, drugs, autonomic failure and seizures. Defecation syncope (DS) and micturation syncope (MS) may be more common than previously described owing to the lack of patient reporting for fear of embarrassment or other factors. It has been estimated by some that defecation and micturation may precipitate up to 4% of cardiovascular events and up to 22% of venous thromboembolic events[6]. DS is a phenomenon that is more common in women and may take years to appropriately diagnose[7, 8]. It can occur at any time throughout the day, generally has an associated GI prodrome and tends not be aggravated by EtOH, all of which are key differences between DS and MS[9]. One often used test for situational syncope is the Tilt Table Test/Head Up Tilt Test[10]. In susceptible patients, this may induce postural symptoms, while the patient is in a carefully monitored environment (“Figure 4”). However, this has been found to be not only cumbersome, but unreliable in the diagnosis of DS[8, 11]. Molnar and Somberg instead propose a heart rate recovery index (HRRI) that better predicts those at risk for DS. The HRRI involves measuring a patient’s heart rate at maximum exercise and then again one minute after exercise cessation. The authors found a significantly greater drop in among those with neurocardiogenic syncope with a sensitivity of greater than 80%. Diagnosis of this condition is important as it may be a sign of underlying chronic disease. Several studies have suggested that DS may be an early form of autonomic failure[12, 13]. One case series reported central abnormalities in the autonomic nervous system or local abnormalities in the innervation of capacitance vessels of the lower limbs and/or splancnic vessels in patients with DS[12]. Another series of 20 patients with DS found about half of the patients with “unknown cause” for their syncope to have significant underlying comorbidities including hypothyroidism, panhypopituitarism and severe CAD or multiple co-existing diseases such as one patient with diabetes and SLE. More importantly this group had quite a high mortality rate of 35% over the 24 months of follow up[13].
4. Conclusions
- Defecation is an important cause of syncope, especially in the elderly population who are more at risk of constipation. There are several potential causes of constipation. They include reversible causes (such as medication side effects and immobility) and non-reversible causes (such as underlying neurological or endocrine disease).While treatment can be difficult, it can also be an elegant solution to a disruptive and harmful problem for patients. Further, DS may be a clue to more serious underlying pathology and should not be overlooked.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML