-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Internal Medicine
p-ISSN: 2326-1064 e-ISSN: 2326-1072
2013; 2(1): 1-5
doi:10.5923/j.ijim.20130201.01
The Evaluation of Nutrition in Male COPD Patients Using Subjective Global Assesment and Mini Nutritional Assesment
Yuceege MB M.D., Salman SO M.D., Duru S M.D., Saygıdeğer Y M.D., Sonmez Z. M.D., Ardıç S.
Dışkapı Educational Hospital, Respiratory Diseases Department, Ankara, Turkey
Correspondence to: Yuceege MB M.D., Dışkapı Educational Hospital, Respiratory Diseases Department, Ankara, Turkey.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Malnutrition in Chronic Obstructive Lung Diseases (COPD) leads to increased hospital admissions. We aimed to investigate the nutritional status of COPD patients with Body Mass Index (BMI), Subjective Global Assesment (SGA) and Mini Nutritional Assesment (MNA) and compare the correlation of SGA and MNA values with air flow limitation, BMI, anthropometric values and hospital admission (HA) for the last 6 months. 60 outpatient COPD patients without comorbidity and infection were enrolled to this cross-sectional study. Malnutrition rate (according to BMI) was related with the COPD severity: %10 in mild ,%13 moderate, %35 severe and 23.3 % in very severe COPD. MNA identified more patients as malnutrioned than SGA (65% versus 41.7 %). BMI, number of HA, triseps skin fold were less in the MNA-malnutritioned group. Adding to those parameters, spirometric values (FEV1, FVC, PEF) were less in the SGA-malnutritioned group . SGA and MNA can be used for the evaluation of the nutritional status in COPD and in addition to that SGA can be a useful method to assess the relation between the nutritional depletion and air flow limitation in COPD noninvasively. Cohort studies can clarify whether MNA enables to earlier diagnosis of malnutrition in COPD then SGA or not.
Keywords: COPD, Nutritional Assessment
Cite this paper: Yuceege MB M.D., Salman SO M.D., Duru S M.D., Saygıdeğer Y M.D., Sonmez Z. M.D., Ardıç S., The Evaluation of Nutrition in Male COPD Patients Using Subjective Global Assesment and Mini Nutritional Assesment, International Journal of Internal Medicine, Vol. 2 No. 1, 2013, pp. 1-5. doi: 10.5923/j.ijim.20130201.01.
Article Outline
1. Introduction
- Chronic Obstructive Pulmonary Disease (COPD) is a chronic disorder, and is one of the global leading cause of morbidity and mortality. Nutritional status disorders pose a serios problem, which concerns about 1/5 of the COPD population (1). Multiple problems cause malnutrition in COPD which can be listed as: 1. Higher metabolism due to increased respiratory work, 2. Chronic inflammation, 3.Medications, 4. Recurrent infections 5. Oral /teeth problems 6. Reduced dietary intake/dietary problems (2-4) . Schols defined this situation as “pulmonary cachexia” (5). ). Most commonly seen form is Protein-Energy-Malnutrition Nutritional status disorders can lead to negative clinical consequences. Body Mass Index <20 is shown to be a predictive factor for hospitalisation in COPD (6).. There is no single test to diagnose malnutrition. Body mass index, history taking, the evaluation of the dietary intake, anthropometric measures (triceps skin fold thickness, mid-arm muscle circumference…), serum proteins (albumine, prealbumine, transferine…), free fat mass index, screening tests (Subjective global assesment, Mininutritional assesment..) are all used in clinical studies. BMI has been integrated in a multidimensional score for mortality risk in COPD (7,8). Adding to that, in patients with low body mass, the diffusion capacity is diminished and air trapping is increased as a consequence of dyspnea. (9) Subjective Global Assessment (SGA) and Mini Nutritional Assessment (MNA) have been introduced for clinical nutritional assessment based on patient history and simple physical status and their use in geriatric patients have been validated. MNA identified more patients as“malnutritioned” than SGA in geriatric group and those identified as normal nutritioned” by MNA appeared to have better 3-year survival than normal nutritioned patients classified using SGA (i.e., 75% and 48% still alive after 3 years, respectively) (10). So early diagnosis of malnutrition is important.There are many studies investigating SGA and MNA in geriatric patients, but there are few studies in COPD patients (11, 12,13) Our aims in this study were to investigate the nutritional status of COPD patients, compare the correlation of SGA and MNA values with air flow limitation, BMI, anthropometric values
2. Methods and Materials
2.1. Patients and Tests
- The study was carried out over 4 months in Dıskapi Educational Hospital (a 1500 bedded hospital) in Ankara, Turkey. The study group consisted of 60 male COPD patients. The diagnosis and severity were determined according to GOLD classification criterias. The patients were qualified both from our outpatient clinics and our clinic. 63 consecutive suitable patients on admision were asked to participate in the study. Three refused to participate, resulting in a sample of 60 patients. Inclusion criterias were: diagnosis of COPD, age 40-75 years, stable state of COPD. The presence of any of these were ruled out of the study: Purulan sputum, worsening of daily respiratory symptoms, ronchus in physical examination and the patients with any disease that could effect nutritional status (thyroid problems, diabetes mellitus, cancer, congestive heart failure). The protocol of the study was approved by the ethics commitee of Dışkapı Educational Hospital Medical Center. An informed consent was signed by all participants. The patient’s body weight, Body Mass Index, Anterior-arm circumference and triceps skin fold (by Caliper) were measured by standart tecniques. Anterior-arm circumference was measured by a soft measure tape. Patient’s bodyweight was measured with light clothes on and without shoes. We classified patients as normal nutritioned if BMİ≥20, and malnutritioned if BMİ<20. All the measurements were done by the same doctor who has got special education in a nutritional clinic. Hemoglobine was measured by immunoturbidometric method , serum prealbumine by nephelometric method and serum albumine by calorimetric method. ..Lung function was measured using by Jaeger in accordance with ERS standarts.; FEV1, FVC, %FEV1, PEF were recorded. Exacerbation rate for the last 6 months were analysed from our hospital records and patient history.
2.2. Nutritional Status
- Assessment of nutritional status was done by Mini Nutitional Assessment (MNA) and Subjective Global Assessment (SGA). SGA was firstly used in gastrointestinal surgery patients. MNA consists 18-score-weighted items. MNA test is an internationally validated, two-step procedure (screening for risk of malnutrition, followed by global assessment of the nutritional conditions), which evaluate the overall health status of elderly subjects including cognitive function, functional status, walking, balance, socio-economic status. (14). The first section deals with BMI, weight loss, appetite, mid-arm and calf circumference of totally 8 points. A general section includes physical and cognitive activity, intake of daily prescribed drugs and pressure sores or skin ulcers in totally 9 points. Dietery intake and habits constitute the third section With items for daily meal times, intake of food, liquid, appetite and feeding assisstance, resulting in 9 points. The last section consists a subjective assessment of respondents’ health and nutritional status, totally 4 points. MNA provides a total score that ranges from 0 to 30. <= 17 points are classified as:”malnutritioned”, while “at risk for malnutrition” when between 17.5-23.5 and “normal nutritioned” when greater than 23.5. SGA, briefly consists of a nutritional history (weight loss during the last 6 months; dietary change and a short physical examination of subcutaneous fat, muscle mass and fluid balance. SGA classifies the patient as having Protein Energy Malnutrition (PEM) or moderate PEM or being normal nutritioned. ( 15)All the SGA and MNA tests were performed by the same doctor in our clinic.
3. Statistical Analyses
- Data analysis was performed by using SPSS for Windows, version 11.5. The distributions of continuous variables were determined by Shapiro Wilk test. Continuous data were shown as mean(standart deviation )or median (minimum-maximum). Means were compared by Student’s t test and medians by Mann Whitney U test. were applied for the comparisons of the median values., when the number of independent groups was two. The differences among more than two groups were evaluated by One-Way ANOVA or Kruskal Wallis test. When the p value from the One-Way ANOVAwas statistically significant, post hoc Tukey test was used to determine which groups differ from the others. A p value less than 0.05 was considered as statistically significant.
4. Results
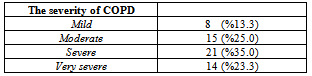
- 60 stable male COPD patients were enrolled to the study. The mean age of the patients was 63±9.4. %68.3 (41 patients)were Empysematous COPD , %16.7 (10 patients) were Chronic bronchitic COPD while %15 (9 patients) were defined as mix type COPD. Malnutrition rate (according to BMI) was related with the COPD severity: %10 in mild COPD, %13 in moderate COPD, %35 in severe COPD, %23..3 in very severe COPD: In Table 1, malnutrition rate in COPD stages are shown.
|
|
|
|
5. Discussion
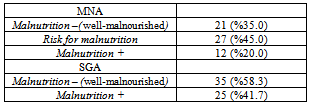
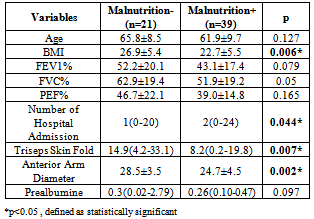
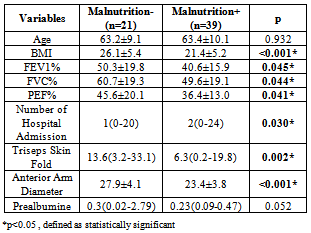
- Nutritional depletion has an important impact on COPD by adversely effecting respiratory and peripheral muscle function, exercise capacity and even mortality rates. Here in this study malnutrition prevalance was found to be %26.7 using BMI, in compatible with the other studies on COPD (1,16,17). Furthermore, depletion of fat-free mass may even occur in normal-weight COPD patients; Vermeeren et all found that the prevalance of normal BMI and low free-fat mass index was %15 in 389 COPD outpatients. Free-fat mass index is not available in many clinics. We were also unfortunately unable to analyze fat-free mass index in this study. We found that malnutrition based on BMI was correlated with the COPD severity: %10 in mild COPD, %13 in moderate COPD, %35 in severe COPD, %23.3 in very severe COPD. By using SGA, %41.7 of the patients were defined as malnutritioned and nutritional status defined by SGA correlated with FEV1, FVC,PEF, triceps skin fold, anterior arm diameter and the number of hospital admissions; those classified as normal nutritioned with SGA score A had statistically significant greater FEV1, FVC, PEF, triceps skin fold, anterior arm diameter and less hospital admission rates than those classified as malnutritioned with SGA scores B and C. On the other hand, FEV1, FVC, PEF and MEF25-75 were less in patients classified as malnutritioned with MNA , but not statistically significant. Only triceps skin fold,,anterior arm diameter and the number of hospital admissions were statistically significantly less in malnutritioned patients with low MNA scores (<17.5). SGA classifies patients as normal nutritioned with SGA-A scores and malnutritioned with SGA-B and SGA-C scores. MNA defines patients as “normal nutritioned” when score is > 23.5, “risk for malnutrition” when the score is 17.5-23.5, “malnutritioned” when the score is ≤17 (10). MNA was spesifically developed to evaluate the risk of malnutrition in elderly people and to identify those who could benefit from early intervention by Guigoz. in 1994 (18)The”risk for malnutrition” group had the patients who could benefit from early intervention. In clinical studies assessing nutritional status in geriatric patients, MNA identified more patients as malnutritioned or at risk for malnutrion than SGA (10,19, 20). SGA classifies patients as:normal (SGA-A), moderately malnutritionerd(SGA-B) and severely malnutritioned (SGA-C); resulting with SGA-B and SGA-C as malnutritioned patients . In a cohort study, MNA identified more patients as “malnutritioned ” than SGA in geriatric group and those identified as “normal nutritioned” by MNA appeared to have better 3-year survival than normal nutritioned patients classified using SGA (i.e., 75% and 48% still alive after 3 years, respectively) (10). This result may be important as it points out to the early therapy for malnutrition. In our study, MNA identified more patients as malnutritioned than SGA when “risk for malnutrition” group is combined with the “normal nutritioned” group in COPD patients similar to the study cited above (10) Anterior arm diameter (AAD) reflects both muscle mass and subcutaneous fat. In our study, both SGA and MNA corralated well with AAD which identified normal nutritioned and malnutritioned patients statistically significantly.( p=0.002 in MNA, p<0.001, in SGA). It is a very simple test and only a tape dispenser is enough to measure it. In our study, by using SGA, malnutritioned group were found to have more empyhsematous patients. (%23 empyhsematous COPD in malnutritioned group versus %18 in normal nutritioned group, ) This is compatible with other studies.(13, 21, 22). There are many studies associated with SGA and BMI evaluating nutritional state; in geriatric patients (23, 24), in hemodialysis patients (25) and cancer (26). SGA questions loss of body weight, weight change by clothing size, diet change ( suboptimal solids, full liquid diet, hypocaloric fluid…), gastrointestinal symptoms, functional examination and physical examination findings :muscle wasting, subcutaneous fat loss and edema. The questions have the following response options: well (A), mild/moderate (B), severe (C). The total score (A, B or C) depends on the majority of the scores A, B and C.MNA questions the patient’s food intake in detail, weight loss, mobility, physcological status, neurophyscological problems, BMI, Mid-arm circumference and Calf-circumference. MNA has more objective and numeric response options than SGA. (eg. 1. Mode of feeding: 0.0 if less than 3 cups, 0.5 if 3-5 cups, 1.0 if more than 5 cups. Eg.2. Mode of feeding: 0 if unable to eat without assistance, 1 if self-fed with some difficulty, 2 if self-fed without any problem. ) MNA takes more patients into “malnutrition” group due to the”risk for malnutrition” cases with any small corruption in nutritional state. MNA seems to diagnose the malnutritioned patients earlier. Spirometric deterioration can be seen later. Cohort studies can clarify this point. Our study was limited to male COPD patients. This could be thougt a s a missing part but many stdies underline the clinic differences betweeen male and female COPD patients (27, 28). We have designedly enrolled male COPD patients in order to overcome possible gender differences in COPD patients and evaluate only the effect of malnutrition on male COPD patients. We concluded in this present study that, the malnutrion rate increases paralely with the stage of COPD. Spirometric measures including FEV1, FVC and PEF deteriorated in the malnutritioned group. Present data support using SGA and MNA for the evaluation of the nutritional status in COPD and in addition to that SGA can be a useful method to assess the relation between the nutritional depletion and air flow limitation in COPD noninvasively. As in the geriatric patients, MNA identified more patients as malnutritioned than SGA in our study. In the geriatric group, this can have significance in early diagnosis and early administration of nutritional therapy. Our study underlines that SGA is correlated with malnutrition, frequent hospital admissions which were shown to be bad prognostic markers in COPD. Cohort studies can clarify whether MNA enables to earlier diagnosis of malnutrition in COPD then SGA or not.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML