-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Genetic Engineering
p-ISSN: 2167-7239 e-ISSN: 2167-7220
2025; 13(9): 212-214
doi:10.5923/j.ijge.20251309.08
Received: Aug. 28, 2025; Accepted: Sep. 22, 2025; Published: Sep. 29, 2025

Evaluation of the Analysis of Quantitative Changes in Cytokines in the Blood of Patients with Cutaneous Leishmaniosis in the Central and Southern Regions of Uzbekistan
Tolibova Shakhlo Erkinovna1, Sattarova Khullar Gayratovna1, 2, Eshkuvatov Sanjar2
1Samarkand State Medical University, Uzbekistan
2L.M. Isayev Scientific Research Institute of Microbiology, Virology, Infectious and Parasitic Diseases under Samarkand State Medical University, Uzbekistan
Correspondence to: Tolibova Shakhlo Erkinovna, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this article, we identify important changes in the blood composition of patients with cutaneous leishmaniasis and compare these changes with the blood of healthy people. Blood samples from people in the area of distribution and endemic areas of cutaneous leishmaniasis were used.
Keywords: Cutaneous leishmaniasis, Interleukin 1, Interleukin-4, Interleukin-6, Cytokines
Cite this paper: Tolibova Shakhlo Erkinovna, Sattarova Khullar Gayratovna, Eshkuvatov Sanjar, Evaluation of the Analysis of Quantitative Changes in Cytokines in the Blood of Patients with Cutaneous Leishmaniosis in the Central and Southern Regions of Uzbekistan, International Journal of Genetic Engineering, Vol. 13 No. 9, 2025, pp. 212-214. doi: 10.5923/j.ijge.20251309.08.
1. Introduction
- Cutaneous leishmaniasis (CL) remains a pressing health problem, particularly in parasitology. According to WHO, 350 million people are at risk of infection each year, and approximately 1 million new cases are recorded worldwide. Given the annual increase in the incidence of cutaneous leishmaniasis in endemic areas of Central Asia, WHO recommends the development of a leishmaniasis control program for endemic areas.In the 2000s-2010s, significant scientific advances were made in the treatment, diagnosis and prevention of leishmaniasis. The results of this research have helped to develop and implement sustainable national and regional programs against leishmaniasis in several countries. Unfortunately, most countries do not have programs to combat these diseases. There is an alarming increase in the incidence of cutaneous leishmaniasis worldwide. Recognizing the global nature of the problem, the World Health Assembly adopted Strategic Resolution 60.13 on the control of leishmaniasis in 2007. This document calls on interested countries to create conditions that will allow WHO to coordinate the provision of technical assistance necessary for the initiation, maintenance and globalization of programs to combat leishmaniasis. One of the main tasks was to develop guidelines for the prevention and treatment of leishmaniasis [3].
2. Materials and Methods
- Today, along with the large-scale measures being implemented in our country to improve the healthcare system, special attention is paid to reducing the incidence of infectious diseases, reducing the incidence rate, and improving the treatment of infectious diseases. In this regard, the tasks of "...increasing the efficiency, quality and accessibility of medical care to the population, as well as creating a medical standardization system, introducing high-tech diagnostic and treatment methods, promoting a healthy lifestyle, and preventing diseases through the creation of effective models of medical care..." have been set. modern medical care and the use of modern technologies and approaches in the diagnosis and treatment of infectious skin diseases require modern medical care and the use of modern technologies and approaches in the diagnosis and treatment of infectious skin diseases.There are two main clinical and epidemiological forms of cutaneous leishmaniasis: anthroponosis (urban, small-wounded, dry cutaneous leishmaniasis) and zoonosis (rural, acute necrotic, moist cutaneous leishmaniasis). Among the local population, the disease primarily affects children, while among visitors it affects people of all ages.Immunity to cutaneous leishmaniasis in humans is permanent and occurs only as a result of natural or artificial (after vaccination) infection. Among the permanent populations of endemic foci of leishmaniasis, the disease mainly affects young children; therefore, immunity is acquired in the first years of life.Therefore, cutaneous leishmaniasis is relatively rare among the adult population of these regions. Immunological changes in cutaneous leishmaniasis are manifested not only in the development of persistent immunity, but also in the development of a predisposition to an allergic reaction to the introduction of a specific antigen. Both types of cutaneous leishmaniasis are characterized by the persistence and uniformity of immune reactions, which determines the high prophylactic effectiveness of vaccination against cultural leishmania [Rodyakin; p. 125-129, Agakishiev; pp. 165-198].A number of diagnostic methods have been developed for the diagnosis of cutaneous leishmaniasis, with significant differences in diagnostic accuracy, including parasitological examination (histopathology, microscopy and parasite culture), serological methods and molecular diagnostics (Goto and Lindoso 2010). Parasitological diagnostic methods remain the gold standard for the diagnosis of leishmaniasis (de Vries et al. 2015) and are crucial in ecoepidemiological studies (Shirian et al. 2014). In vitro diagnosis can be performed by direct examination of amastigotes from Giemsa-stained wound specimens, skin scrapings, biopsies or blood samples from wounds (Boelaert et al. 2007).
3. Result and Discussion
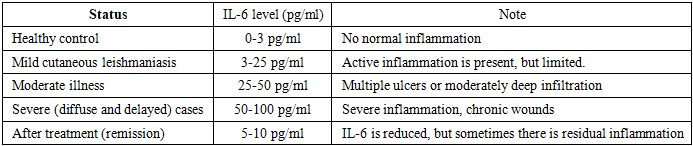
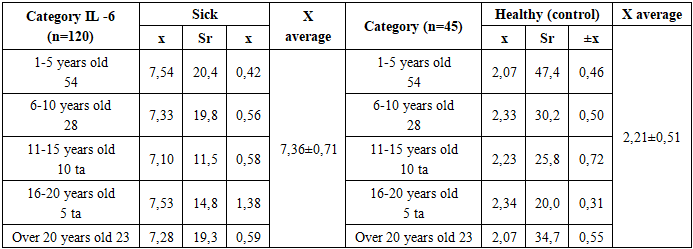
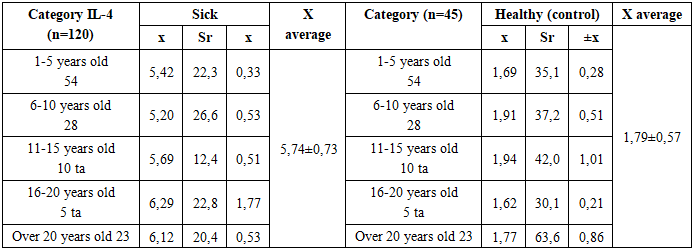
- In cutaneous leishmaniasis, pro-inflammatory cytokines are produced. Depending on the balance and dynamic changes in cytokines, clinical outcomes may be controlled or predicted. T helper 1 (Th1) inflammatory cytokines (especially interferon-γ, tumor necrosis factor-α, and interleukin-12) are crucial factors in initiating protective immunity against primary L. infection, while T helper 2 cytokines, including IL-5, IL-4, and IL-13, are down-regulating cytokines. On the other hand, increased inflammatory responses lead to collateral tissue damage and ulcer formation. Therefore, the immune system, such as regulatory T cells, produces cytokines that regulate the damage that may occur as a result of increased inflammatory responses at the site of infection.The aim of the study is to analyze and evaluate changes in the quantitative indicators of anti-inflammatory cytokines (interleukin-1, interleukin-4, interleukin-6) in patients with cutaneous leishmaniasis [4].Results of the study. At the L.M. Isayev Scientific Research Institute of Microbiology, Virology, Infectious and Parasitic Diseases under the Samarkand State Medical University, blood serum tests were conducted to determine the interleukin (cytokine) profile in patients with cutaneous leishmaniasis. 100 patients with cutaneous leishmaniasis were examined. 20 healthy people were included in the control group for the determination of IL-4. Serum IL-4 was determined using immunoenzyme diagnostics with the appropriate test system of OJSC "Vector-Best" (Novosibirsk). The level of IL-4 in the blood of patients with cutaneous leishmaniasis was 2.6 ± 0.4 in healthy controls, compared with 6.5 ± 0.7 (P <0.05). In patients with cutaneous leishmaniasis with concomitant parasitoids, this indicator was even higher - 11.1 ± 1.2 pg / ml (.P <0.05). The duration of the disease process, the lack of vaccines, and the toxicity of etiotropic therapy can negatively affect the course of TL, especially in patients with zoonotic cutaneous leishmaniasis. Objective of the study: When determining the level of IL-4 in patients with zoonotic cutaneous leishmaniasis, the level of IL-4 is significantly increased [5].A total of 100 patients with cutaneous leishmaniasis were examined. The comparison group consisted of 100 patients. For the determination of IL-4, 40 healthy people were included in the control group. Serum IL-4 was determined using immunoenzyme diagnostics with the appropriate test system of AO Vector-Best (Novosibirsk). The results were statistically processed.The level of IL-4 in serum in patients with cutaneous leishmaniasis was 6.5 ± 0.7 compared to 2.6 ± 0.4 in healthy controls (P < 0.05). Thus, there was a significant increase in the level of IL-4, which, according to the literature, is a sign of the development and prolongation of the pathological process.The results of the study showed that the level of IL-6 is increased in cutaneous leishmaniasis, especially in the stage of active infection. The following main indicators are observed:In active leishmaniasis:The level of IL-6 is higher than normal.This indicator may be related to the severity of the disease (more number of ulcers, size, resistance to treatment).Increased inflammatory response is reflected in IL-6 levels [1,2].In remission (recovery phase): IL-6 levels begin to gradually decrease. This indicates that IL-6 is elevated during periods of active inflammation (de Lima et al., 2019). IL-6 levels were 2-3 times higher in patients with active cutaneous leishmaniasis compared to controls.
|
|
|
4. Conclusions
- As a result of the studies, a significant change in the level of inflammatory mediators - interleukins - in patients with cutaneous leishmaniasis was scientifically substantiated. While the level of IL-1 in the healthy control group was on average 1.93± 0.64 pg/ml, in patients this indicator increased to 5.44±0.50 pg/ml, which is almost 2.2 times higher. While IL-6 was 2.21± 0.51 pg/ml in healthy subjects, in patients it increased to 7.36±0.71 pg/ml, which is 2.3 times higher. IL-4 levels increased to 5.74±0.73pg/ml in patients compared to 1.79± 0.57pg/ml in the control group, which was 2.5 times higher.These changes indicate that the balance between proinflammatory (IL-1, IL-6) and anti-inflammatory (IL-4) cytokines is disrupted in the pathogenesis of cutaneous leishmaniasis, and that the immune response plays a crucial role in the course of the disease through shifts in the Th1/Th2 direction. Moreover, an increase in IL-1 and IL-6 indicates an active inflammatory phase of the disease, and an increase in IL-4 indicates an increase in the humoral immune response.The results of the study show that an increase in IL-1, IL-4 and IL-6 levels by 2–2.5 times compared to the norm can be used as an important biomarker in the diagnosis of cutaneous leishmaniasis and in assessing its severity. The detection of these interleukins using modern biochemical methods is of scientific and practical importance in early diagnosis of patients, differentiation of disease forms, and increasing the effectiveness of treatment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML