-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2019; 7(1): 18-22
doi:10.5923/j.ijcp.20190701.03

An Overview of the Genetic Influence of Schizophrenic Patients Treated at the Lakipadada Hospital
Kristanty Randa Arung1, Syafari Daniel Mangopo2
1Psychiatrist in Lakipadada Hospital, Tana Toraja, Indonesia
2Director of Lakipadada Hospital, Tana Toraja, Indonesia
Correspondence to: Kristanty Randa Arung, Psychiatrist in Lakipadada Hospital, Tana Toraja, Indonesia.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Schizophrenia is a complex severe mental disorder with pathogenesis that involves many risk factors. Many studies have tried to examined the role of genes which responsible for the etiology of schizophrenia. The Lakipadada Hospital in Tana Toraja (Indonesia) has treated 2.322 outpatient and 81 inpatient of schizophrenic patients on the 2018. In January until April 2019, it has 500 outpatient and 18 inpatient. This study aims to describe the genetic influence of schizophrenic patients who are treated outpatient and inpatient at The Lakipadada Hospital from January to April 2019. The subjects consist of 101 persons, they are schizophrenic patients who traced to a family history of schizophrenia in the first, second and third generations, they are examined using Tools Brief Psychiatric Rating Scale (BPRS). The study was approved by the Ethics Commitee of Lakipadada Hospital. The datas will analyzed by using Pearson test for each items of BPRS then we use a multivariate analysis with linear regression to determine a constant item derived to the across generation. The Pearson's test determine 3 items from BPRS that have a strong relationship in every across generation, they are conceptual disorganization (r=0,474; p=0,00), suspiciousness (r=0,471; p=0,000) and hallucinatory behavior (r=0289; p=0,04). After a linear regression test, hallucinatory behavior item is constantly inherited in schizophrenic patients in every across generation (Anova: p=0,005, r=1,030 and r=0,995), ith Adjusted R Square 0,986. Hallucinatory behavior item of the BPRS are constantly inherited to each schizophrenic patient who has a genetic history of schizophrenia across generations.
Keywords: Schizophrenia, Genetic influence, BPRS
Cite this paper: Kristanty Randa Arung, Syafari Daniel Mangopo, An Overview of the Genetic Influence of Schizophrenic Patients Treated at the Lakipadada Hospital, International Journal of Clinical Psychiatry, Vol. 7 No. 1, 2019, pp. 18-22. doi: 10.5923/j.ijcp.20190701.03.
Article Outline
1. Introduction
- Schizophrenia is a complex severe mental disorder with pathogenesis that involves many risk factors. The prevalence of schizophrenia in the world about 1% of the population with an incidence rate of 1 per 10,000 people per year [1]. In the 2007, the prevalence of schizophrenia in Indonesia was 2 per mile, but in the 2013 increased to 2.6 per mile [2,3,5]. Symptoms in men usually occur at the end of childhood or early 20s, whereas in women in their 20s or early 30s [1].Psychopathology in schizophrenia can be classified into three dimensions, they are consist of positive symptoms, negative symptoms and disorganization symptoms. The positive symptoms include hallucinations, delusion, excitement, odd behavior and hostility. The negative symptoms include blunt or flat affect, withdrawal, reduced motivation, poor emotional contact (quiet, difficult to talk), passivity and apathy. The symptoms of disorganization include speech, behavioral disorganization and disruption in concentration and information processing [2,3].The etiology of schizophrenia is still unclear, but it is thought to involve genetic factors, perinatal and gestational factors, psychosocial stressors and neurochemical factors (dopamine hypothesis and serotonin hypothesis) [1,3,4].Genetic factors play an important role of etiology schizophrenia. It has a significantly inheritance, complex and polygenic. In the twin studies, monozygotic twins have a 4-6 times risk than dizygotic twins. The risks of schizophrenia during life are as follows: in monozygotic twins (40-50%), dizygotic twins (10%), schizophrenic siblings (10%), children of one schizophrenic parent (10-15%) and children of both schizophrenic parents (30-40%). Linkage analysis based on the fact from the affected individuals concluded that they are received chromosomal material from the ancestor, it was explained why in the families had multiple affected individuals [8,9,23,24,26].Several large meta-analyses have found strong evidance of nomerous genetic linkages of 6p24-22, 1q21-25, 22q11-12, 5q21-33, 10p15-11, and 1q42 [6-9].The Torajan ethnic has the high cases of schizophrenia among other ethnic in South Sulawesi. The Lakipadada Hospital in Tana Toraja (indonesia) has 2.322 schizophrenic outpatient and 81 inpatient on the 2018. At January until April 2019, it has 500 schizophrenic outpatient and 18 inpatient.The studies about genetic schizophrenia in Indonesia is still limited when compared with studies in other developed countries. Based on the background, this study aimed to describe the genetic influence of schizophrenic patients who are treated inpatients and outpatients at Lakipadada Hospital from January to April 2019.
2. Methods
2.1. Subjects
- One hundred and one schizophrenic patients were recruited from Lakipadada Hospital. The subjects have family history of schizophrenia in the first, second and third generations, they are examined using Tools Brief Psychiatric Rating Scale (BPRS). The study was approved by the Lakipadada Ethics Commitee. Inclusion criteria included: (1). ICD-10 diagnostic criteria for schizophrenia; (2). Schizophrenic patients who have a family history of schizophrenia. Exclusion critera included is schizophrenic patients who have history of drug abuse.
2.2. Design and Procedure
- This study was an observational analytic studies. The study was approved by the Lakipadada Ethics Commitee, in Lakipadada Hospital, Tana Toraja, Indonesia, and all experiments were performed in accordance with relevant guidelines and regulations. After a detailed explanation of the study protocols, all subjects and their family were given written informed consent for participating in this study and the publication of the results.Each patient and family who came for treatment at the Lakipadada hospital was measured by Brief Psychiatric Rating Scale (BPRS) scale, then we analyzed each items on the Brief Psychiatric Rating Scale (BPRS) scale which tended to be derived from the previous generation.Brief Psychiatric Rating Scale (BPRS) is a widely used instrument for asessing the positive, negative, and affective symptoms of individuals who have psychotic disorders, especially schizophrenia. It should be administrated by clinician who is knowledge able concerning psychotic disorder and able to interpret the constructs used in the assessment. Also considered is the individual’s behavior over the previous 2-3 days and it can be reported by the patient’s family [10].
2.3. Measurement
2.3.1. Psychometric Measures
- The BPRS consists of 18 symptoms include somatic concern, anxiety, emotional withdrawal, conceptual disorganitation, guilt feelings, tension, mannerism and posturing, grandiosity, depressive mood, hostility, suspiciousness, hallucinatory behavior, motor retardation, uncooperativesness, unusual throught content, blunted affect, excitement and disorientation. It takes 20-30minutes for the interview and scoring. The rater should enter a number ranging from 1 (not present) to 7 (extremely severe). 0 is entered if the items is not assessed. First published in 1962 as a 16-construct tool by Drs.John Overall and Donald Gorham, the developers added two additional items, resulting in the 18-item scale used widely today to assess the effectiveness of treatment [10].
2.3.2. Statistical Analysis
- The data was analyzed using statistical program (SPSS) and presented with tables. The data will be analyzed using Pearson’s test then continue with a linear regression test to get the constantly inherited in schizophrenic patients in every across generation.
3. Result
3.1. Subjects Characteristic
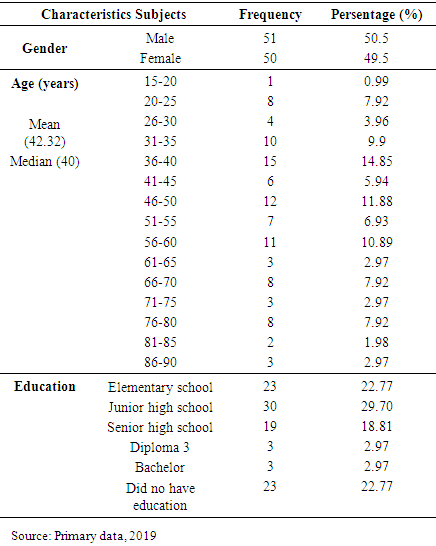
- The demographic characteristics of the subjects are shown in table 1.
|
3.2. The Genetic Influence of Schizophrenic Patients
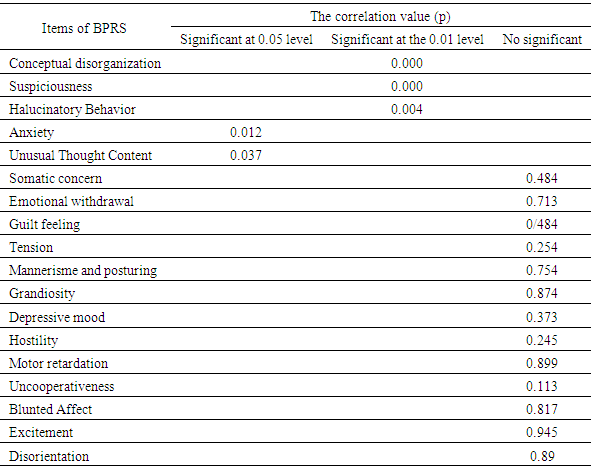
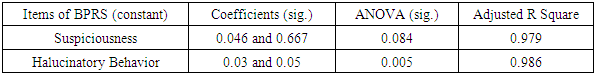
- Based on statistical results using Person test, there are 5 items of BPRS that are statistically significant and inherited genetically in schizophrenic patients. The statistical results of the Person test are shown in table 2.
|
|
4. Discussion
- Schizophrenia commonly has a chronic course albeit with fluctuating patterns, and cognitive disability. Its hallmark is psychosis, mainly characterized by positive symptoms such as hallucinations and delusions that are frequently accompanied by negative (deficit) symptoms such as reduced emotions, speech, and interest, and by disorganization symptoms such as disrupted syntax and behavior. Severe mood symptoms, up to and including manic and major depressive episodes, are present in many cases [11,12,15,17,18].There are no diagnostic laboratory test for schizophrenia; instead, the diagnosis relies on clinical observation and self-report. Epidemiological studies over the last century using clinical phenotype, it has consistenly shown the importance of genetic factors in schizophrenia. Psychiatric genetics has historically focused in large part on the study of schizophrenia and its epidemiology. It is well-established that the heritability of schizophrenia is > 80%, among the highest known for complex genetic disorders. 22q11.2 deletion syndrome (22q11.2DS; previously George syndrome and velocardiofacial syndrome) is the only established genetic subtype of schizophrenia of proven clinical relevance. The association of 22q11.2DS with schizophrenia followed soon after the discovery in the early 1990s that the 22q11.2 deletion was the underlying molecular anomaly unifying several, seemingly distinct, clinical syndromes first described in the 1960s and 1970s [7,13,14,15,22,25,26].Many of the studies determine that the genetic etiology of schizophrenia, include spontaneous mutations, reduced penetrance, and variable expressivity, are found in 22q11.2DS. Several studies have confirmed that 22q11.2DS accounts for approximately 1% of all cases of schizophrenia. Conversely, an estimated 22.5% of adults with 22q11.2DS develop schizophrenia or a related psychotic disorder [16,17,18,26].22q11.2DS is also associated with the psychotic symptoms in schizophrenic patients such as auditory hallucinations and delusional. It is also explain the impact of 22q11.2DS on the inheritance of the next generation. Based on this study, we found that the clinical symptoms of BPRS that were constantly inherited across generations are halucinatory behaviors [19-26].This study had several limitation. The limitation including: (1). Sample is still in small group, (2). Limitations of tools for detecting chromosomes that are responsible for inheritance of schizophrenia.Future directions in this area include the following:Ÿ Collection of sufficiently large samples and better methods of pedigree ascertainment to obtain power to detect linkage and then loci to chromosomal regionsŸ Application of large-scale family-based association tests across the whole genome.Ÿ Resolution of genetic heterogeneity requires further work on phenotypic classification to identify clinical characteristics that can delineate genetically distinct groups.
5. Conclusions
- These study was support that schizophrenia is associated with strongly genetic predisposition. It shows that the hallucinatory behavior is a clinical symptom that is inherited constantly across generations.
ACKNOWLEDGEMENTS
- The authors declare that there is no conflict of interest regarding the publication of this paper. The authors would like to acknowledge the important support and contributions of Syafari Daniel Mangopo (Surgeon; Director of Lakipadada Hospital).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML