-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2018; 6(3): 52-56
doi:10.5923/j.ijcp.20180603.02

A Study to Assess the Anxiety among the Adolescents Suffering from Epilepsy at a Tertiary Care Hospital in Mysore, Karnataka
Harsha G. T.1, Ashok Kumar K. S.2
1Assistant Professor, Department of Psychiatry, BGS Global Institute of Medical Sciences, Bangalore
2Assistant Professor, Department of Psychiatry, Mandya Institute of Medical Sciences, Mandya
Correspondence to: Ashok Kumar K. S., Assistant Professor, Department of Psychiatry, Mandya Institute of Medical Sciences, Mandya.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

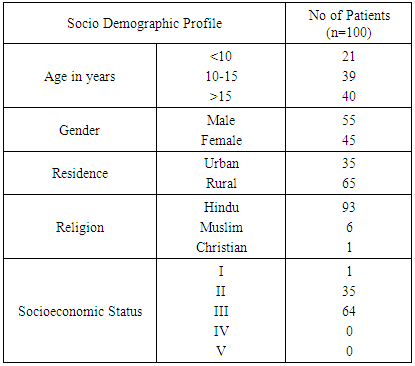
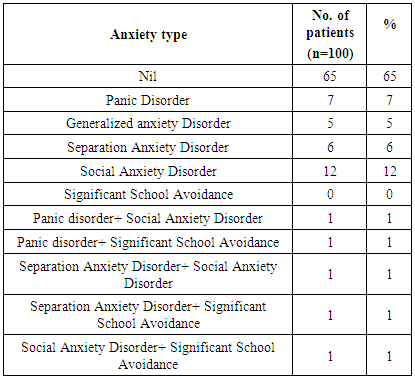
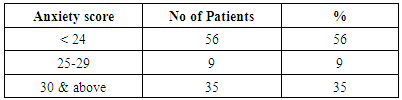
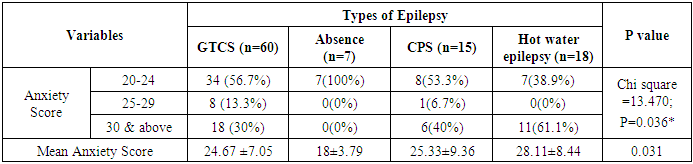
Background: Historically psychiatric disorders in epilepsy were considered to be a consequence of psychosocial disturbance due to poor adaptation to a chronic disease, but recent studies have suggested that epilepsy and psychiatric disorders are best conceptualized as epiphenomena rather than cause or consequence. These studies foster the need for study of bidirectional relationship between psychiatric disorders and epilepsy, suggesting that behavioral and psychosocial impairment in epilepsy may be the consequence of unrecognized psychiatric disorder rather than the cause of a psychiatric condition. Objective: A Study to Asses the Anxiety among the Adolescents suffering from Epilepsy. Materials and Methods: 100 consecutive children and adolescents aged 8-17years diagnosed to have epilepsy presenting to the paediatric and neurology outpatient department of J.S.S. Hospital, Mysore from December 2011 to June 2013 were enrolled for the study. Detailed socio-demographic and epilepsy characteristics were recorded in proforma specially designed for the study after fulfilment of the inclusion and exclusion criteria. After screening for mental retardation, all the patients were assessed using self-report CDI for anxiety. Results: About 35% of patients could be grouped into specific anxiety disorder with majority of patients having social anxiety disorder and various other types of disorders as mentioned in the table. 5% of patients had mixed type of anxiety which has been detailed in the above table. 44% of patients had significant anxiety scores with 35% of them having very elevated scores. Conclusion: Increased awareness of the clinical presentations of anxiety and depressive disorders may help clinicians to develop effective prevention and intervention strategies to improve the long term outcome.
Keywords: Anxiety, Adolescents, Epilepsy, Cdi, Psychiatric
Cite this paper: Harsha G. T., Ashok Kumar K. S., A Study to Assess the Anxiety among the Adolescents Suffering from Epilepsy at a Tertiary Care Hospital in Mysore, Karnataka, International Journal of Clinical Psychiatry, Vol. 6 No. 3, 2018, pp. 52-56. doi: 10.5923/j.ijcp.20180603.02.
Article Outline
1. Introduction
- There is strong evidence to suggest that neurological diseases are accompanied by psychological disturbances. [1-4] One such neurological disorder is epilepsy, which is the disturbance of the nervous system that abruptly interferes with ongoing behavior, perception, movement, consciousness and other brain functions. Epilepsy is one of the world’s most prevalent non-communicable diseases affecting approximately 50 million people in the world with no age, racial, social class, and national or geographical boundaries. [5-7] It has to be acknowledged that more than 80% of people with epilepsy live in developing countries, where the condition remains largely untreated. [8]Aprroxuamtely nearly 25% of the world population who are suffering from epilepsy are below 15 years of age. [9] Many studies done by various researchers showed the annual incidence rate of epilepsy is about 60-124 per 100000 population and is around 40-50 per 100000 population in developed countries.Moreover, epilepsy is considered by several researchers [3, 10, 11] to represent the most common chronic neurological disorder in childhood. It is a rather unique neurological disorder in that the clinical presentation, progression and underlying etiology appear to vary across clinical cases.Historically psychiatric disorders in epilepsy were considered to be a consequence of psychosocial disturbance due to poor adaptation to a chronic disease, but recent studies have suggested that epilepsy and psychiatric disorders are best conceptualized as epiphenomena rather than cause or consequence. These studies foster the need for study of bidirectional relationship between psychiatric disorders and epilepsy, suggesting that behavioral and psychosocial impairment in epilepsy may be the consequence of unrecognized psychiatric disorder rather than the cause of a psychiatric condition.There is an increased risk of behavioural problems and psychiatric disorders amongst children with epilepsy, said to be 3 to 6 times higher compared with normal children and those with other chronic disorders like diabetes. Of these, anxiety, depression and attention disorders are the most common and well-studied. Although anxiety and depressive disorders have distinct features that enable separate classification in the Diagnostic and Statistical Manual of Mental Disorders 4thEdition65 (DSM-IV-TR) [10], these two mood disorder stend to exist co-morbidly and are often studied together. The relationship between epilepsy and mood disorders is thought to be bidirectional rather than a simple cause-and-effect phenomenon.Interictal anxiety and depression can exert independent adverse effects on health-related quality of life (HRQOL). In addition, frequent, severe, and chronic seizures also reduce HRQOL, but appear less powerful predictors of HRQOL than interictal psychiatric symptoms. Recognition and treatment of co-morbid depression and anxiety thus form an important consideration in improving quality of life in Epilepsy. [11]The three most common pediatric anxiety disorders—separation anxiety, generalized anxiety and social phobia—have much in common and can be readily distinguished from other childhood anxiety disorders. Generalized anxiety disorders are common anxiety diagnoses in children, with a reported prevalence range of 0.5 to 7.1 percent. Pediatric generalized anxiety disorder is commonly associated with other anxiety disorders and mood disorders. Up to 50 percent of children and adolescents with generalized anxiety will have another psychiatric disorder. In children and adolescents the anxiety disorders are consider to be one of the most common psychiatric diagnosis, and have been shown to affect 5-18% of children, 0.3-12.9% of pre adolescents and 0.6-7% of adolescents. The prevalence of anxiety in paediatric epilepsy is estimated to be 15 to 20%.Historically psychiatric disorders in epilepsy were considered to be a consequence of psychosocial disturbance due to poor adaptation to a chronic disease, but recent studies have suggested that epilepsy and psychiatric disorders are best conceptualized as epiphenomena rather than cause or consequence. These studies foster the need for study of bidirectional relationship between psychiatric disorders and epilepsy, suggesting that behavioral and psychosocial impairment in epilepsy may be the consequence of unrecognized psychiatric disorder rather than the cause of a psychiatric condition. Moreover children with epilepsy are found to have more risk of psychiatric disorders. Unfortunately these children with epilepsy are often unrecognized and left untreated for these psychiatric disorders, which can lead to negative outcome on quality of life.As there are no published Indian studies throwing light on these issues it is difficult to gauge the prevalence of this comorbidity in the Indian context. Hence our study aims to make clinicians aware of accompanying psychiatric symptoms in epileptic children to aid in early detection and treatment of psychiatric comorbidities.
2. Objective
- A Study to Asses the Anxiety among the Adolescents suffering from Epilepsy.
3. Materials and Methods
- The Cross Sectional study was conducted in the Department of Pediatric and Neurology at J.S.S. Hospital, Mysore from December 2011 to June 2013.
4. Sample Procedure
- The study enrolled 100 consecutive children and adolescents aged 8 to 17years diagnosed to have epilepsy presenting to the outpatient Department of Paediatric and Neurology at J.S.S. Hospital, Mysore from December 2011 to June 2013. Detailed socio-demographic and epilepsy characteristics were recorded in proforma specially designed for the study after fulfillment of the inclusion and exclusion criteria. After screening for mental retardation using Binet- Kamath test for intelligence, all the patients were assessed further using self-report CDI and SCARED scales for depression and anxiety respectively. All the data was collected by Interview technique in a pretested and semi structured questionnaire after obtaining the informed consent from the parents.After screening for mental retardation using Binet- Kamath test for intelligence, all the patients were assessed further using Self-report for childhood anxiety related emotional disorders (SCARED) for assessment of anxiety disorders. [12] The SCARED was initially developed by Birmaher and his collaborators. 81 It comprises of 38-items that can be grouped into five subscales. Four of these subscales measure anxiety disorder symptoms as conceptualized in the DSM-IV-TR: panic disorder, generalized anxiety disorder, separation anxiety disorder, and social anxiety. The fifth subscale, school anxiety, represents a common anxiety problem in childhood and adolescence. [12]The 38-item SCARED questionnaire was employed in this study. The adolescent rated each symptom on a 3-point scale: 1 (almost never), 2 (sometimes), 3 (often). The subscales of the questionnaire are: panic disorder (13 items), generalized anxiety disorder (9 items), separation anxiety disorder (8 items), social anxiety (4 items), and school anxiety (4 items).Children’s Depression Inventory was 27 item self-rated symptom orientated scale suitable for school age children and adolescents to screen for Depression among the adoloscents.Presence of psychiatric disorder prior to the onset of seizure disorder and Mental Retardation were excluded from the study.The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc. Data are expressed In term of Percentage and figures. Appropriate Statistical test have been used to test the level of Significance. P<0.05 is considered as significant.
5. Results
- A total of 100 subjects were Selected for the study in the study period who were found to be not mentally retarted by Binet-kamath intelligence scale
|
|
|
|
6. Discussion
- Patients with epilepsy have a high prevalence of psychiatric comorbidity. Most psychiatric disturbances are predominant in people with drug-resistant epilepsy and temporal lobe epilepsy, with/without associated neurological or mental abnormalities and psychosocial problems. [13, 14] Comorbidity of epilepsy may be due to a shared pathophysiological mechanism, however, coincidence or selection bias cannot always be excluded. In addition, genetic, psychosocial and iatrogenic factors may also contribute to the co-morbidity. 22 Comorbidity of epilepsy and psychiatric disorders are often, yet the most common are depression, nervousness and anxiety, less common being psychosis and schizophrenia. [15]The different type of epilepsy seen in our study was similar to the study findings of the Mandebaum and Burack [16], Mendez et al [17] and Hoare et al [18]. Roeder et al [19] stated that greater number of AEDs was independently associated with severe symptoms of anxiety, suggesting the number of AEDs to be a risk factor for undetected symptoms of Anxiety. Plioplys [20] stated that the depressogenic effect of AEDs cannot explain development of depression in children per se; suggesting this effect to be related to the side effects of individual drugs. Oguz et al [21] stated that anxiety was significantly higher in patients receiving more than one AED.The effectiveness of psychological treatments, such as cognitive-behavioral therapy (CBT), has been well established in the adult literature. For example, studies have revealed that CBT and other psychological approaches can lead to improvements in quality of life and even reductions in seizure frequency. Unfortunately, despite the recognized clinical need for psychosocial interventions in pediatric epilepsy [22] similar studies with children and adolescents have been minimal. Among the available studies, there are multiple methodological limitations that affect their applicability to clinical practice, such as small sample sizes, poor treatment specificity, and questionable differential diagnosis within the samples. Studies on the pharmacotherapy of anxiety disorders have revealed that SSRIs, including fluoxetine, fluvoxamine, sertraline, and citalopram are effective in treating anxiety disorders in children and adolescents. [23] At this time, there are no known controlled studies of the medication therapy of anxiety disorders in adults or children with epilepsy. However, investigations supporting the safety of SSRIs in the treatment of depression in patients with epilepsy are likely applicable to the treatment of anxiety disorders in this population. As previously discussed, some AEDs can exacerbate anxiety in certain types of patients, especially in the context of polytherapy. However, it has been further shown that some AEDs have anxiolytic effects. Valproate, gabapentin, tiagabine, and vigabatrin have been used with varying success in the treatment of anxiety disorders in adult studies. [24] In a review of the literature, Mula et al. [25] indicated that the strongest evidence for the antianxiety effects of AEDs has been demonstrated for pregabalin in social phobia and generalized anxiety disorder, lamotrigine in posttraumatic stress disorder, and gabapentin in social anxiety. In their general psychiatric use, benzodiazepines are routinely used in conjunction with SSRIs in the management of anxiety disorders in adults. Their use with children is typically reserved for symptomatic treatment of severe anxiety on a short-term basis. However, it should be highlighted that benzodiazepines carry with them a high risk of dependency when used in long term treatment.Considering all the above facts currently SSRI’s remain the best treatment option with the combination of CBT in childhood depression and anxiety. [26]
7. Conclusions
- Of greater concern is that only one third of those who were diagnosed sought or received mental health treatment. This represents an area of unmet health needs, with a significant impact on long term mental and physical health outcome. Hence there is a need for increased awareness and better training to address issues on diagnosis, monitoring and treatment. While multimodality treatment aimed at the patient, family and community currently represents the best approach, more research is required to determine best practices so that these children can make a smooth and happy transition to adulthood.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML