-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2018; 6(3): 47-51
doi:10.5923/j.ijcp.20180603.01

A Study to Asses the Magnitude of Depression in Children and Adolescents with Epilepsy
Harsha G. T.1, Rajesh Raman2, Ravi M. D.3, T. S. S. Rao2
1Department of Psychiatry, BGS Global Institute of Medical Sciences, Bangalore
2Department of Psychiatry, JSS Medical College and Hospital, Mysore
3Department of Pediatrics, JSS Medical College and Hospital, Mysore
Correspondence to: Harsha G. T., Department of Psychiatry, BGS Global Institute of Medical Sciences, Bangalore.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

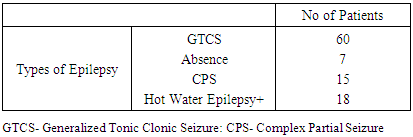
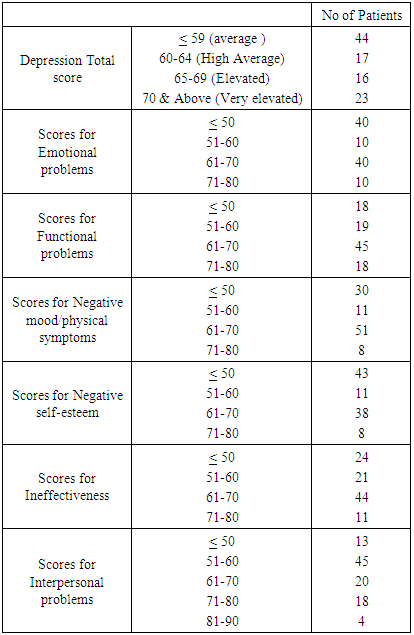
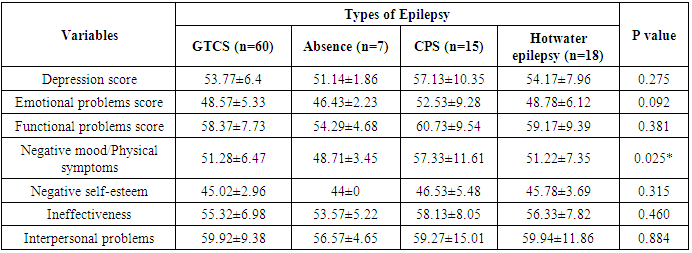
Background: While the risk of mental health problems is increased in young people with chronic epilepsy, many characteristics of these disorders remain to be clarified, including their distribution, timing /onset, aetiology and course. An assumption has been that factors associated with seizures or their chronicity increase the risk of psychiatric comorbidity. However, recent population-based studies report that certain mental health problems, specifically depression, anxiety and suicidal ideation, represent independent risk factors for unprovoked seizures in children and adolescents. These studies provoke the need for study of bidirectional relationship between psychiatric disorders and epilepsy, suggesting that behavioural and psychosocial impairment in epilepsy may be the consequence of unrecognized psychiatric disorder rather than the cause of a psychiatric condition. Objectives: To study the relationship between demographic and epilepsy related Depression among the children and adoloscents. Materials and Methods: 100 consecutive children and adolescents aged 8-17years diagnosed to have epilepsy presenting to the paediatric and neurology outpatient department of J.S.S. Hospital, Mysore from December 2011 to June 2013 were enrolled for the study. Detailed socio-demographic and epilepsy characteristics were recorded in proforma specially designed for the study after fulfilment of the inclusion and exclusion criteria. After screening for mental retardation, all the patients were assessed using self-report CDI for depression and anxiety respectively. Results: The study sample contained four different types of epilepsy namely GTCS(60%), Absence(7%), focal/CPS(18%) and hot water/ reflex epilepsy(18%). About 39% of the sample had elevated depression scores. In particular focal/CPS variety had significantly elevated scores for negative mood when compared to absence seizures. Conclusion: Although depression symptoms are frequently seen in children and adolescents with epilepsy, they are under recognized and undertreated. It is essential that children and parents receive education about depression and anxiety disorders.
Keywords: Epilepsy, Depression, Adoloscents, Seizures, Psycosocial
Cite this paper: Harsha G. T., Rajesh Raman, Ravi M. D., T. S. S. Rao, A Study to Asses the Magnitude of Depression in Children and Adolescents with Epilepsy, International Journal of Clinical Psychiatry, Vol. 6 No. 3, 2018, pp. 47-51. doi: 10.5923/j.ijcp.20180603.01.
Article Outline
1. Introduction
- Epilepsy is one of the world’s most prevalent non-communicable diseases affecting approximately 50 million people in the world with no age, racial, social class, and national or geographical boundaries [1]. Worldwide, it is estimated that 10·5 million children under 15 years have active epilepsy, representing about 25% of the global epilepsy population.9 Of the 3·5 million people who develop epilepsy annually, 40% are younger than 15 years, and more than 80% live in developing countries. [2] Population-based studies on childhood-onset epilepsy indicate annual incidence rates of 61–124 per 100 000 in developing countries, and 41–50 per 100000 in developed countries. Incidence falls progressively from around 150 per 100 000 in the first year of life to 45–50 per 100000 after the age of 9 years. [2]Over the past half century, neuropsychology has played an increasingly important role in the assessment of people with epilepsy. Advances in our understanding of brain-behavior relationship have mirrored the rapidly expanding technologies of diagnostic neurophysiology and structural and functional neuro-imaging, resulting in a more accurate understanding of the effects of seizures on higher cortical functions. [3] Furthermore, behavior does not only become altered in the presence of organic variables that alter the structure and functioning of the central nervous system, but also in the presence of psychological and social variables that are mediated through the nervous system. [4, 5] Thus, since the organ of pathology in epilepsy is the brain, epilepsy has been implicated as a cause of impaired behavioral, emotional and cognitive functioning in children suffering from this disorder. [6]A number of psychiatric and neuropsychiatric disorders are found to occur at a higher rate in children with epilepsy. Among all types of psychiatric illnesses in epilepsy, depression and anxiety are most commonly reported psychiatric problems followed by ADHD, OCD, autism, mental retardation and psychotic disorders. Hence this study was carried out to assess the magnitude of Depression among the childhood and adolescents who are suffering from epilepsy.
2. Objective
- To study the magnitude of depression in children and adolescents with Epilepsy and its correlation with Sociodemographic factors.
3. Materials and Methods
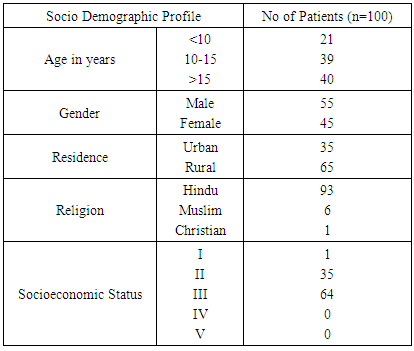
- The Cross Sectional study was conducted in the Department of Pediatric and Neurology at J.S.S. Hospital, Mysore, Karnataka, India from December 2011 to June 2013. The study enrolled 100 consecutive children and adolescents aged 8 to 17years diagnosed to have epilepsy presenting to the outpatient Department of Pediatric and Neurology at J.S.S. Hospital, Mysore. Detailed socio-demographic and epilepsy characteristics were recorded in proforma specially designed for the study after fulfillment of the inclusion and exclusion criteria. All patients between the age group of 8-17 years of either gender who have been diagnosed as epilepsy with or without medication were included in the study after obtaining the informed Consent. Presence of psychiatric disorder prior to the onset of seizure disorder and Mental Retardation were excluded from the study. No Mood Modulator drugs were given in our study. All the study participats were screened for any other diseases and all the biochemical values were normal were included in the study.
4. Tools Used
- 1. A detailed proforma specially designed for the study to collect data, which included demographic, seizure related and antiepileptic medication related details. 2. Binet-kamath intelligence scale for screening mental retardation.3. Children’s depression inventory-2[CDI-2] for assessment of depression. [8]The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver. 2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc. Data are expressed in term of Percentage and figures. Appropriate Statistical test have been used to test the level of Significance. P<0.05 is considered as significant.
5. Results
- A total of 100 subjects were Selected for the study in the study period who were found to be not mentally retarted by Binet-kamath intelligence scale.
|
|
|
6. Discussion
- The cause of depression in patients with epilepsy are probably multifactorial, including clinical (seizure frequency, seizure type or foci, epilepsy duration, age at onset) and psychosocial factors (quality of life, life stressors, employment, marital status). [8] Clinical or psychosocial factors cannot fully account for the high prevalence of depression in patients with epilepsy because the biological characteristics of epilepsy also affect the manifestation of depression. [9, 10]For depression, age and gender have been the most studied child characteristics. While some studies showed a correlation with increasing age/adolescence, others have not found such a relationship. Adolescent females are at highest risk of depression in the general population, but the evidence for female preponderance in children with epilepsy is inconsistent, with only a few studies showing a relationship. Regarding demographic factors e.g. age and gender, Caplan et al [11] indicated that there has been a tendency for epileptic patients with affective and anxiety disorders to be female (63% vs 43%), however, the correlation was not significant. Turky et al [12] showed that female gender was an independent predictor for depression in epileptic subjects (73.7% vs 26.3%, P=0.04).
|
7. Conclusions and Recommendations
- The prevalence of symptoms of depression is high in patients with epilepsy, consistent with previous studies on children and adolescents with epilepsy. Although depression symptoms are frequently seen in children and adolescents with epilepsy, they are under recognized and undertreated. It is essential that children and parents receive education about depression disorders. Increased awareness of the clinical presentations of depressive disorders may help clinicians to develop effective prevention and intervention strategies to improve the long term outcome. The role of pediatrician is discerning depression symptoms in this special population is of prime importance for the holistic management of the child. Prompt referral at the earliest will ensure better treatment outcome with respect to both psychiatric co-morbidity as well as seizure control in these individuals.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML