-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2018; 6(2): 27-33
doi:10.5923/j.ijcp.20180602.01

Effect of Non-Computerized Cognitive Remediation on the Cognitive Function of the Schizophrenic Patients Treated with Typical Antipsychotic
Sonny Teddy Lisal1, Saidah Syamsuddin1, Kristanty Randa Arung2, Idham Jaya Ganda3, Theodorus Singara1, Rinvil Renaldi1
1Department of Psychiatry, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia
2Postgraduate, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia
3Department of Pediatric, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia
Correspondence to: Kristanty Randa Arung, Postgraduate, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Schizophrenia is a severe mental disorder associated with deterioration in the function of everyday life and social functions. The study aims to determine the effect of non-computerized cognitive remediation on the cognitive function of schizophrenic patients who were treated with typical antipsychotics. It is an experimental study of the schizophrenic inpatients who were admitted to the regional special hospital of South Sulawesi Province for the first time for at least six months. The study was conducted from August to September 2017. The subjects consist of 32 patients divided into 2 groups: 16 subjects as an experimental group and other 16 subjects as a control group. The data were statistically analyzed with Wilcoxon test. The study showed that statistically, 12 sessions of non-computerized cognitive remediation had not been able to improve the patient’s cognitive dysfunction (the mean: 39.75, SD: 9.82 p=0.108) but there were tendency of improved cognitive dysfunction on the graph of each subjects. Therapy with typical antipsychotic makes the cognitive dysfunction in the patients becomes more severe (mean: 53.25, SD: 9.12, p=0.002). Longer series of non-computerized cognitive remediation are needed and reduction of the dosage of antipsychotic drugs whenever there has been a clinical improvement of the symptoms or switching the typical antipsychotics to atypical antipsychotics by considering the dosage equivalence. Brain Derived Neurotrophin Factor (BDNF) was also required to determine the effectiveness of non-computerized cognitive remediation.
Keywords: Schizophrenia, Non-computerized cognitive remediation, Typical antipsychotic
Cite this paper: Sonny Teddy Lisal, Saidah Syamsuddin, Kristanty Randa Arung, Idham Jaya Ganda, Theodorus Singara, Rinvil Renaldi, Effect of Non-Computerized Cognitive Remediation on the Cognitive Function of the Schizophrenic Patients Treated with Typical Antipsychotic, International Journal of Clinical Psychiatry, Vol. 6 No. 2, 2018, pp. 27-33. doi: 10.5923/j.ijcp.20180602.01.
Article Outline
1. Introduction
- Schizophrenia is a severe mental disorder associated with deterioration in the function of everyday life and social functions. The prevalence of schizophrenia in the world is about 1% of the population. Psychopathology of schizophrenia can be classified into three dimensions, positive symptoms, negative symptoms and disorganization symptoms. The positive symptoms include hallucinations, delusion, agitated, freak behavior and hostility. The negative symptoms include blunted or flat affects, withdrawal, reduced motivation, poor emotional contact (quiet, difficulty to talk), passive and apathetic. The disorganization symptoms include speech and behavior disorganization and disruption of attention and information processing [1, 2].Deterioration of cognitive function is also found in schizophrenic patients, so cognitive deficits are one of the core symptoms of schizophrenia. Cognitive dysfunction in schizophrenic patients has a very high prevalence, and estimated 98% of schizophrenic patients indicate a worsening of cognitive function. This deterioration can usually be identified early in the course of the illness, before receiving antipsychotic therapy and will continue to stay throughout the course of schizophrenia [3, 4]. The cause of cognitive dysfunction in schizophrenia is abnormality anatomical and functional of neuronal cells in the brain. Recent study emphasizes that the cause of cognitive dysfunction of schizophrenic patients due to abnormality neuroplasticity of neuronal cell in the brain, it was caused by molecular changes in mRNA expression for the formation of neurotransmitters, transporters and their receptors or changes in the expression and secretion of neurotropin which responsible for the development of neural circuits and modulate the synapse function in the brain [5, 6].Typical antipsychotic drugs for schizophrenic patients (such as haloperidol, chlorpromazine) may cause cognitive dysfunction because it is not only blockade D2 receptors in the mesolimbic, but also blockade D2 receptors in other places such as D2 receptors in the mesocortical pathway, thereby aggravating the negative symptoms and cognitive function as the result of decreased dopamine in this pathway [7, 8].The new therapeutic approach to schizophrenia involves multi-dimensional interventions to reduce disability in multiple domains. One of approach is psychiatric rehabilitation. Rehabilitation is a process of refunctionalization and development to enable patients with disabilities to increase their perform and social functions in community. Psychiatric rehabilitation is aimed to improved psychological, social and occupational functions [9]. Cognitive remediation is one of the psychiatric rehabilitation by providing an intervention to improve the neurocognitive skills. Initially the program was given individually to the schizophrenic patient by completing the task according to the instructions. The task is designed to activate the frontal and temporal system, it consists of three mayor tasks, they are cognitive flexibility, working memory and planning. Some methods of cognitive remediation was developed rapidly, ranging from simple methods without using a computer (non-computerized) to computerized methods (computerized) [5, 6].Previous studies by Haut et al (2010); Bor et al (2011), had proven the effectiveness of cognitive remediation on improving cognitive function by using imaging, such as Magnetic Resonance Imaging (MRI), Functional Magnetic Resonance Imaging (fMRI), Near-Infrared Spectroscopy (NIRS), Magnetoencephalography (MEG), Positron Emission Tomography (PET) and DiffusionTensor Imaging (DTI). The study showed an increase activity in the Prefrontal Cortex (PFC), frontal gyrus area, Anterior Cingulate Cortex (ACC), parietal, temporal, parahipokampal and limbic regions and also increased gray matter volume in the temporal and hippocampal areas after schizophrenic patients receive cognitive remediation therapy (using both non-computerized and computerized cognitive remediation) [10, 11].Studies about psychiatric rehabilitation in Indonesia, especially cognitive rehabilitation using cognitive remediation is still very limited when compared with studies in other developed countries to improve cognitive function of schizophrenic patients. Based on this background, this study aimed to determine the effect of non-computerized cognitive remediation on the cognitive function of schizophrenic patients who receive typical antipsychotic therapy.
2. Methods
2.1. Subjects
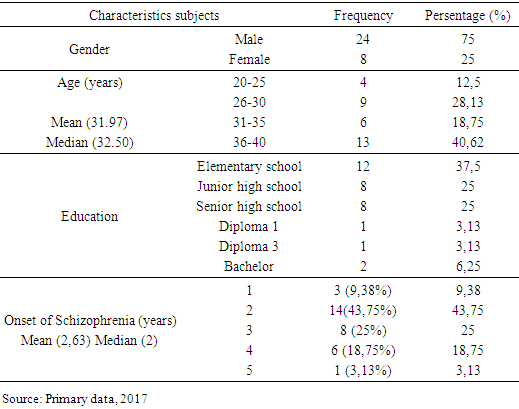
- Thirty-two admitted inpatients with schizophrenia (24 males and 8 females, mean age 31.97 years, range from 20 to 40) were recruited from Special Hospital of the Province of South Sulawesi. The subjects were divides into two groups, an experimental group (consist of 16 patients) received combination therapeutic doses of typical antipsychotic and non-computerized cognitive remediation for 12 sessions (2 session in a week) and the a control group (consist of 16 patients) received therapeutic doses of typical antipsychotic without non-computerized cognitive remediation for 6 weeks. Inclusion criteria included: (1). ICD-10 diagnostic criteria for schizophrenia; (2). The subjects could write and read; (3). Graduated at least for elementary school; (4). Clinically they did not suffer mental retardation; (5). The onset of schizophrenia within 5 years; (6). They could communicate properly according to Positive and Negative Syndrome Scale (PANSS) 30-60 (range from absent to minimal symptoms); (7). They had deficits cognitive function according to Schizophrenia Cognition Rating Scale with Indonesian version (SCORSVI) at least 40 (range from mild to severe deficits cognitive function). Exclusion criteria included: (1). Schizophrenic patients who have history of drug abuse; (2). Suffer physical illness which could not attend the complete series of non-computerized cognitive remediation. The subjects were stratified by age, gender, education and onset of schizophrenia disorder.
2.2. Design and Procedure
- This study was an experimental study using an open randomized of clinical trial design. The study was approved by the Ethics Commitee of Faculty Medicine, Hasanuddin University and Special Hospital of the Province of South Sulawesi, and all experiments were performed in accordance with relevant guidelines and regulations. After a detailed explanation of the study protocols, all subjects and their guardians were given written informed consent for participating in this study and the publication of the results. An experimental group received 12 sessions of non-computerized cognitive remediation. It included 2 sessions in a week for 6 weeks with duration of 60 minutes. Both of the group received therapetic doses of typical antipsychotic included Haloperidol tablets 7,5-15 miligrams per day and Chlorpromazine tablet 100-300 miligrams per day. The treatment procedure consisted of subjects training on cognitive remediation module with guidance / assistance from therapist. Cognitive remediation module consist of three domain task including task for attention, executive memory and understanding and application in daily life. It is consisted of 4 sessions, with duration 60 minutes for each session. All the task in cognitive remediation module had undergone validity test by an expert and has been tested on study by Herdaetha, A [9]. If the subjects could finish the task correctly, they will be given positive reinforcement to improve the subjects 's achievement.
2.3. Measurement
2.3.1. Psychometric Measures
- § Psychiatric symptomatology was evaluated using The Positive and Negative Syndrome Scale (PANSS) which had been validated for Indonesia language version. PANSS consist of 3 items scale included the positive, negative and general psychopathology scales [12]. The subjects of this study have PANSS score range from 30 to 60, so they can communication properly.§ Deficits cognitive function was evaluated using Schizophrenia Cognition Rating Scale with Indonesian version (SCORSVI) which had been validated for Indonesia language version. SCORSVI is a measurement scale based on interviews and focusing on everyday functions. SCORSVI consists of 20 questions which the interviewer must ask to the patient and the informant in a separate interview. Each question item is assessed by 4 points of measurement scale, included: 1: none; 2: mild; 3: moderate; 4: severe. There is also possibility to inserting N / A (non-applicable) scale if for some reason related to the patient's condition, this question can not be applied. In addition to the 20 question items, there was also a global function scale assessment (1-10) to conclude globally the condition of cognitive dysfunction experienced by schizophrenic patients [13].
2.3.2. Statistical Analysis
- The data was analyzed using statistical program (SPSS) and presented as tables and graphs. All variables found to be not normally distribution using Shapiro-Wilk test, so it was analyzed using nonparametric test. Wilcoxon test was used to compare each group with pre and post test group.
3. Result
3.1. Subjects Characteristic
- The demographic characteristics of the subjects are shown in table 1.
|
3.2. Effect Non-computerized Cognitive Remediation to Cognitive Function and Clinical Symptoms
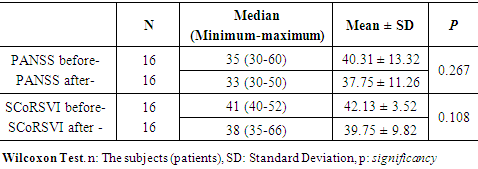
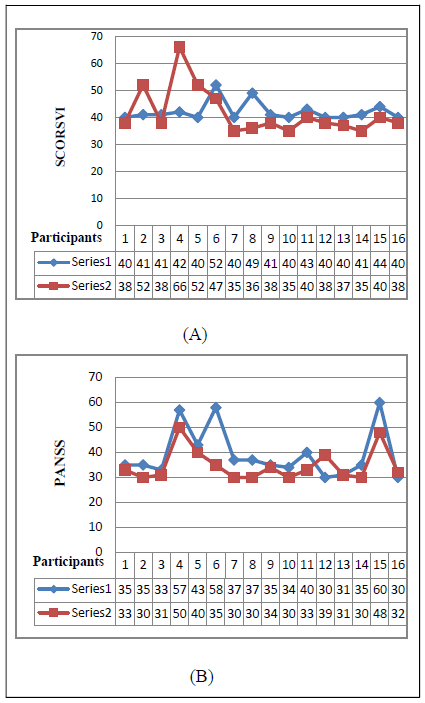
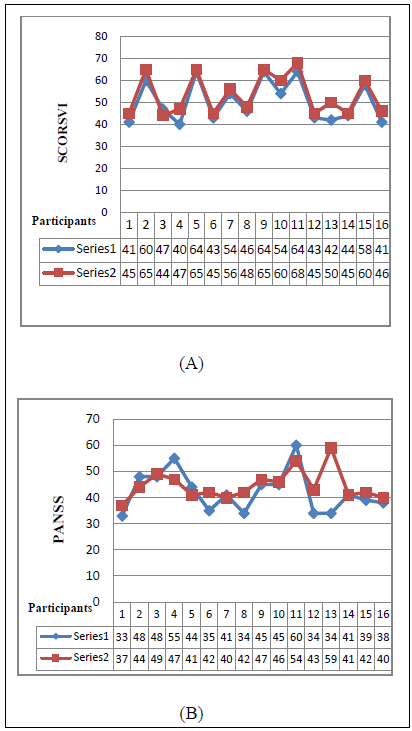
- In an experimental group, the wilcoxon test analysis showed that there was no significant difference in PANSS and SCORSVI scales before and after 12-sessions non-computerized cognitive remediation (pPANSS = 0.267 and p SCoRSVI = 0.108) because decrease of mean score in PANSS scale average only 2.56, while decrease of mean score in SCORSVI scale average only 2.38. The wilcoxon test results was shown in table. 2.
|
|
4. Discussion
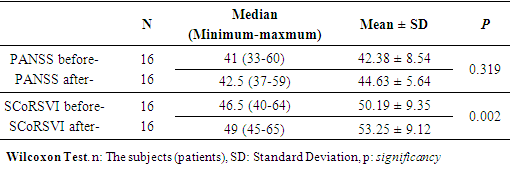
- In a meta-analysis study of cognitive remediation in schizophrenic patients, 26 studies were found with 1,151 schizophrenic patients, the mean duration of cognitive remediation was 12.8 weeks (SD = 20.9, range 1-104) had improved the dysfunctional of cognitive function domain in schizophrenic patients (attention and memory function). But, for social cognitive function, cognitive remediation will provide maximum results if accompanied by other psychosocial rehabilitation [14]. The duration of each session also varies, averaging 1 hour per session at a frequency of 2-3 times each week [14-16].Cognitive remediation initiated when positive symptoms (hallucinations, delusion, aggressive behavior and hostility) have been controlled by using antipsychotic drugs (PANSS scale approximately range from 30 to 60), sedation effects of antipsychotic medications was minimal and it was not combine with ECT (Electro Convulsive Therapy) therapy because patients who received ECT therapy might experience cognitive changes during and after ECT therapy [16]. On the table 1, the highest level of education was elementary schools, this can be explained by using a downward drift hypothesis. The hypothesis stated that highest prevalence of schizophrenia was in low socioeconomic or who fail to come out from lower socioeconomic groups, the economic condition was the main reason why the schizophrenic patient’s education only elementary school. Most of the subjects in this study were stopped their compulsory education without finishing it. According to neuroinflamation theory, the presence of intrauterine infection (especially the second trimester of pregnancy) could trigger the occurrence of inflammatory reactions. Immune responses involving type 2 cytokines (IL-6 and IL-10) might inhibit the indoleamine enzyme 2,3-dioxygenase (IDO) resulting increased production of kinurenic acid. Kinurenic acid is a natural NMDA antagonist in the human brain, blockade of NMDA receptors will cause a decrease in glutamanergic neurotransmitters. Decrease of glutamate neurotransmitters causes cognitive dysfunction in schizophrenic patients. Cognitive dysfunction of schizophrenic patient caused academic disability, so it is not uncommon for schizophrenic patients to be unable to continue their education, just as an elementary school [17]. Base on the wilcoxon test results in the experimetal group, it showed that there was no significant difference before and after 12 sessions of non-computerized cognitive remediation, but from the graph of each subjects showed there was a tendency of decrease the SCORSVI and PANSS scales, indicating improvement of cognitive dysfunction and clinical symptoms in schizophrenic patients, although the improvement is still minimal. 13 subjects had decreased on SCORSVI scale, it was consistent with the literature that tasks in the cognitive remediation was designed to improve the neurocognitive skills of the patient through cognitive remediation, it was expected an improvement of the brain structure and functional integrity through the neuroplasticity system. Clinical improvements indicated a change on cellular level and functional connectivity and neuronal tissue in the brain. Non-computerized cognitive remediation might also increase the Brain-Derived Neurotropin Factor (BDNF) levels. Schizophrenic patients showed a decreased BDNF which could cause failure of brain neuroplasticity mechanisms and other morphological and neurochemical changes in the brain. BDNF is a neurotropin, a protein which responsible for regulating the survival and differentiation of neuronal cells, regulating cellular maturation and stabilization, arrange the neurotransmitter release, enhancing the function of synapses between neurons, plays an important role in neuroplasticity in the brain and regulates the plasticity of dopaminergic, cholinergic and serotonergic neurons. BDNF expression have a positive impact on the formation of LTP (Long Term Potentiation) which important in memory function regulation. A polymorphism study on Val66met BDNF causes a change in brain volume characterized by decreased gray matter volume in the frontal lobes and an increase in lateral ventricular volume [5, 11, 20].There were 3 subjects showed an increase in SCORSVI Scale after non-computerized cognitive remediation was administered, this can be explained as follows:1. The different responses in patients who received cognitive remediation related to the genetic role. The studies by Bosia, et al (2014) was shown that the polymorphism of COMT (Cathecol-O-Methyltransferaase) gene rs 4680 might cause changes in dopamine regulation in the brain, it was cause changed the transmission of dopamine in the brain, synthesis neurotropic factors such as BDNF and also affect the activity of the prefrontal area of the cortex [18].2. Using typical antipsychotic with therapeutic dose had a major impact on cognitive function of the patient, it was worsen of cognitive function and cause negative symptoms of schizophrenic patients. This occurs through the blockade of D2 receptors in the mesocortical pathway, whereas dopamine in the mesocortical required to cognitive function. Giving 12 sessions of non-computerized cognitive remediation had not been able to resolved the impact of blockade of D2 receptors on mesolimbic due to the use of typical antipsychotic therapy [1, 8, 19].3. The possibility of mild or moderate mental retardation may aggravate the cognitive function of schizophrenic patients, it also make the patient does not provide improvement with non-computerized cognitive remediation [1].Based on wilcoxon test results in the control group showed a significant difference in the cognitive function of schizophrenic patients who only received typical antipsychotic therapy without 12 sessions of non-computerized cognitive remediation for 6 weeks. Based on the graph of each subjects, it was showed a tendency of increased of the SCORSVI scale, this is consistent with the literature that the use of typical antipsychotic has a major impact on cognitive function of the patient, it worsens cognitive functioning by blocking dopamine at dopamine D2 receptors in mesocortical pathways, whereas dopamine in the mesocortical required for cognitive function [1, 8, 19].This study had several limitation. The limitation including: (1). We are not measured of PANSS and SCORSVI scale periodically every week which it could be specific indicated the clinical symptoms and cognitive function of subjects, and influenced greatly affect to the patient's ability to perform cognitive remediation task, (2). There were no screening for mild to moderate mental retardation accurately in subjescts. Mental retardation may also lead to cognitive dysfunction of schizophrenic patients.The obstacle of this study including: (1). The level of the patient’s boredom in performed tasks was varied, so it takes effort for directing the attention of patients by giving positive reinforcement, (2). The condition of environment sometimes not conducive for non-computerized cognitive remediation because of interference from other patients.
5. Conclusions
- In conclusion, 12-sessions non-computerized cognitive remediation had a tendency to improve the cognitive dysfunction of schizophrenic patients who received therapeutic dose of typical antipsychotic, so we suggested more session of non-computerized cognitive remediation while schizophrenic patients received a typical antipsychotic because there was a tendency of decreased SCORSVI scale concomitantly with more session of non-computerized cognitive remediation in this study [14, 19]. Using typical antipsychotic could worsen the cognitive dysfunction of schizophrenic patients, so we suggest a decrease of dosage of the drug if there had been improvement of clinical symptoms or switching the typical antipsychotics to atypical antipsychotics by considering the dosage equivalence [1, 8, 19]. Brain Derived Neurotrophin Factor (BDNF) was necessary to determine the effectiveness of non-computerized cognitive remediation [5, 11, 20, 21].
ACKNOWLEDGEMENTS
- The authors declare that there is no conflict of interest regarding the publication of this paper. The authors would like to acknowledge the important support and contibutions of Idham Jayaganda, M.D (Pediatrician; Research Methodology).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML