-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2018; 6(1): 19-25
doi:10.5923/j.ijcp.20180601.03

Comparison of Sleep Quality Using Pittsburgh Sleep Quality Index (PSQI) on Patient with Anxiety Disorders Treated Using Long-Term and Short-Term Benzodiazepine Therapy
Faisal Idrus1, Sonny Teddy Lisal1, Idham Jaya Ganda2, Jumiarni3
1Department of Psychiatry, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia
2Department of Pediatric, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia
3Postgraduate, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia
Correspondence to: Jumiarni, Postgraduate, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Benzodiazepines are widely used and become the primary choice for sleep disorders. This study aims to determine the comparison of sleep quality in patients with anxiety disorders using long-term and short-term benzodiazepines. This study was a cross-sectional observational study conducted on anxiety disorder patients who undertake medical check-up in Hasanuddin University Hospital and its network. The study was conducted from October to November 2017. The subject of the study was 94 divided into two groups, the group of 64 subjects were taking benzodiazepine alprazolam, and the group of 30 subjects were taking clobazam. From each group, the quality of sleep of subjects taking alprazolam and clobazam for long-term (>6 months) and short-term (≤6 months) would be assessed. Data were analyzed statistically by using Mann-Whitney and Wilcoxon test. The results showed that sleep quality which was measured by using an Indonesian version of The Pittsburgh Sleep Quality Index (PSQI) to the group of subjects taking long-term alprazolam i.e >6 months (mean: 9.343.39) and taking short-term alprazolam i.e ≤6 month (mean: 4.061.07), had a very significant difference (p <0.001). The results of the study of the groups taking long-term clobazam i.e >6 months (mean: 4.401.50) and those taking short-term clobazam i.e ≤6 months (mean: 3.33±0.72) had significant differences (p= 0.021). This study concludes that sleep quality in subjects with anxiety disorders using long-term benzodiazepine therapy either on alprazolam or clobazam was worse than subjects who use short-term benzodiazepine therapy.
Keywords: Sleep quality, Alprazolam, Clobazam, PSQI
Cite this paper: Faisal Idrus, Sonny Teddy Lisal, Idham Jaya Ganda, Jumiarni, Comparison of Sleep Quality Using Pittsburgh Sleep Quality Index (PSQI) on Patient with Anxiety Disorders Treated Using Long-Term and Short-Term Benzodiazepine Therapy, International Journal of Clinical Psychiatry, Vol. 6 No. 1, 2018, pp. 19-25. doi: 10.5923/j.ijcp.20180601.03.
Article Outline
1. Introduction
- In 1996 the World Health Organization issued a "Rational Use of Benzodiazepine" program because in daily practice benzodiazepines is not only given to patients with psychiatric disorders, but most of these classification of drugs is 80% used by general practitioners and non-psychiatric physicians. Therefore, the use of benzodiazepines is irrational and against the rules of usage agreed upon by the world health organization. [1, 2]Benzodiazepines class of drugs known to the public as a tranquilizer is the most popular drug in the world. More than 100 million benzodiazepine-class drugs have been prescribed to treat symptoms associated with sleep disorders. Although in reality this drug is intended for short-term use which is for only a few weeks but many have been using it for years. [3, 4, 6] Benzodiazepines are widely used and become the primary choice for sleep disorders, both primary and secondary sleep disorders are sleep disturbances due to anxiety disorders and other mental disorders. However, long-term use should be limited because if used more than 6 months it may lead to some side effects such as addiction, sleep quality problems or may cover the underlying diseases of sleep problems, sleep apnea, cognitive impairment and motor coordination disorders. Therefore, the use of benzodiazepines should be with cautious, within medical supervision, and the dosage use should be as low as possible. [4, 11, 12, 13]Sleep is one important factor for basic human physiological needs. A recovery process for the body and brain for optimal health achievement occurs while sleeping. Sleep needs considered as the physiological needs or primary needs that are the basic requirement for human survival and this depend on the quality of sleep. Sleep quality will affect the psychological and physical health of a person. Various mental disorders are known to interfere with the disruption of a person's sleep quality, such as anxiety disorders, depression, and severe mental disorders. Sleep quality is measured using the Indonesian version of the Pittsburgh Sleep Quality Index (PSQI). The selection of the Indonesian version of the PSQI instrument is due to its practicality and is easily understood. Moreover, it has been widely used in Indonesia with a high degree of validity and extent of reliability. [5, 6, 15, 19, 20] Previous research by Holbrook et al (2000) state that the sleep quality on the short-time benzodiazepine use (24 weeks) is better than long-term use (52 weeks), but Collin et al (2012), states that there is an improvement in quality of sleep on the use of 24 weeks to 1 year. Researchers are interested in conducting this research due to the difference previous research and the absence of specific research in Indonesia that links the long-term use of benzodiazepines to sleep quality. Thus, this study aims to determine the comparison of sleep quality in patients with anxiety disorders using long-term and short-term benzodiazepines. [13, 16, 22]
2. Methods and Material
- The study was an observational analytic study with cross sectional design.
2.1. Subjects
- The subjects were recruited at the psychiatric polyclinic of Hasanuddin University Hospital and its networks on October-November 2017. The population of this study were patients with anxiety disorder receiving benzodiazepine therapy and met the inclusion criteria. All subjects were 30-55 years old. All subjects were provided with complete written and oral descriptions of the study, written informed consent was also obtained. The protocol was approved by the local ethics committee.
2.2. Procedure
- The Ethics Committee of Medical Faculty, Hasanuddin University approved the study, and all experiments performed in accordance with relevant guidelines and regulations. All subjects who met the inclusion criteria interviewed to obtain the sample identity data including initials of name, gender, age, educational level, occupation and duration therapy.We recorded the data of each patient who received benzodiazepine therapy and met the inclusion criteria in the study group. Those data are their personal identity and history of current and previous diseases. The scale of the Indonesian version of the Pittsburgh Sleep Quality Index (PSQI) for subjects receiving benzodiazepine therapy >6 months and those receiving benzodiazepine therapy ≤6 months was determined. Prior to conducting an assessment of the scale of the Pittsburgh Sleep Quality Index (PSQI) Indonesian version, firstly the validity and reliability are tested. The data collected statistically with computerized system were processed and analyzed. Data was analyzed using statistical program (SPSS) by Mann-Whitney and Wilcoxon test.
2.3. Instrument
- The sleep quality is measured by Indonesian version of the Pittsburgh Sleep Quality Index (PSQI). This instrument has been standardized and widely used in sleep quality studies as in Majid research (2014). The Indonesian version of Pittsburgh Sleep Quality Index (PSQI) Scale consists of 9 questions. In this variable using the ordinal scale with the overall score of the Pittsburgh Sleep Quality Index (PSQI) is 0 to 21 which is derived from 7 assessment components such as subjective sleep quality, the time required to start sleep (sleep latency) sleep duration, sleep efficiency, sleep disturbance, use of medication, and sleep disturbances that are commonly experienced during the day (sleep duration), sleep efficiency, daytime dysfunction. If the higher score is obtained, the worse the quality of someone's sleep. The advantage of this scale is having high validity and reliability. But there are also short comings of PSQI that is in the filling requires assistance to reduce the difficulty of respondents when filling questionnaire. Each component has a score range of 0 - 3 with 0 = never in the past month, 1 = 1 time a week, 2 = 2 times a week and 3 = more than 3 times a week. The score of the seven components is summed to 1 (one) global score with a range of 0 - 21 values. There are two interpretations on this Indonesian version of PSQI is good sleep quality if score ≤5 and sleep quality is poor if score >5. [5, 10, 21]
3. Result
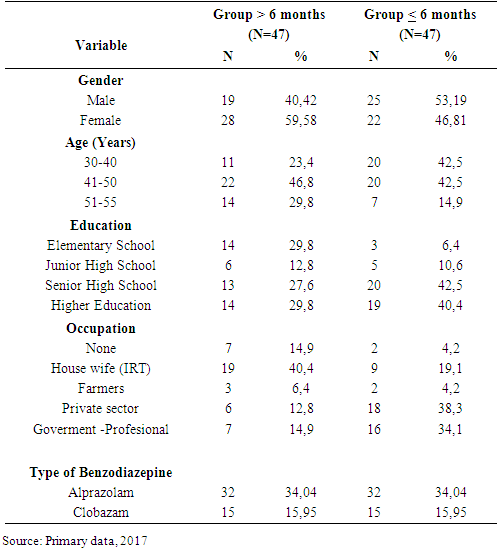
- The characteristics of both groups were taking benzodiazepine more than 6 months and less than 6 months. (see table 1)
|
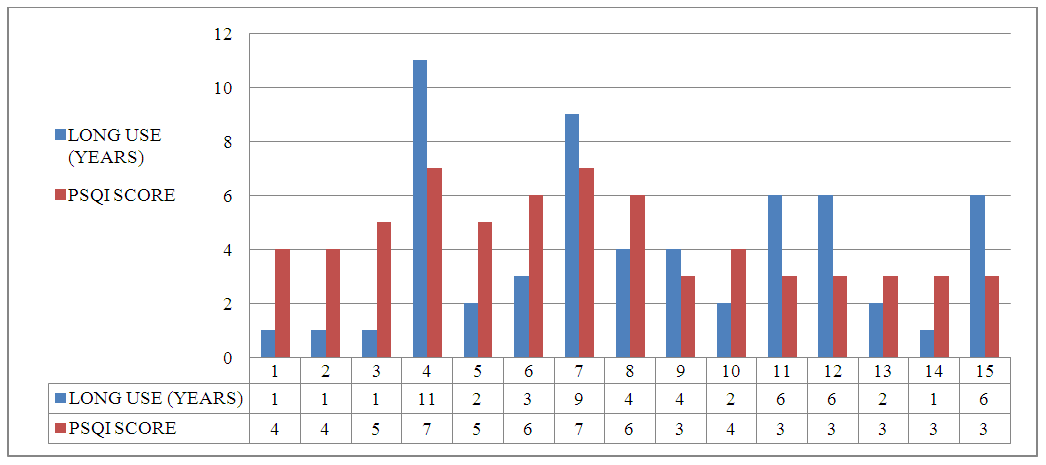
|
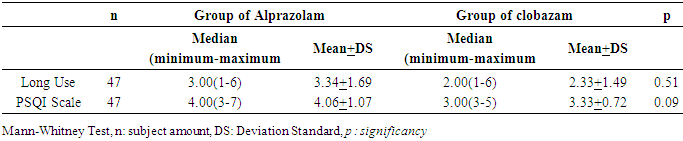
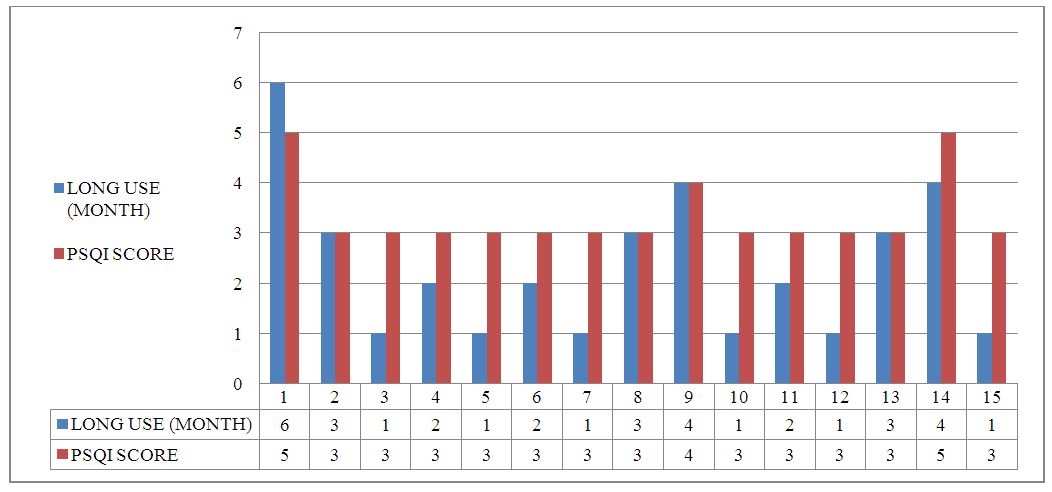
 | Figure 1. PSQI sleep quality scale on alprazolam used >6 months |
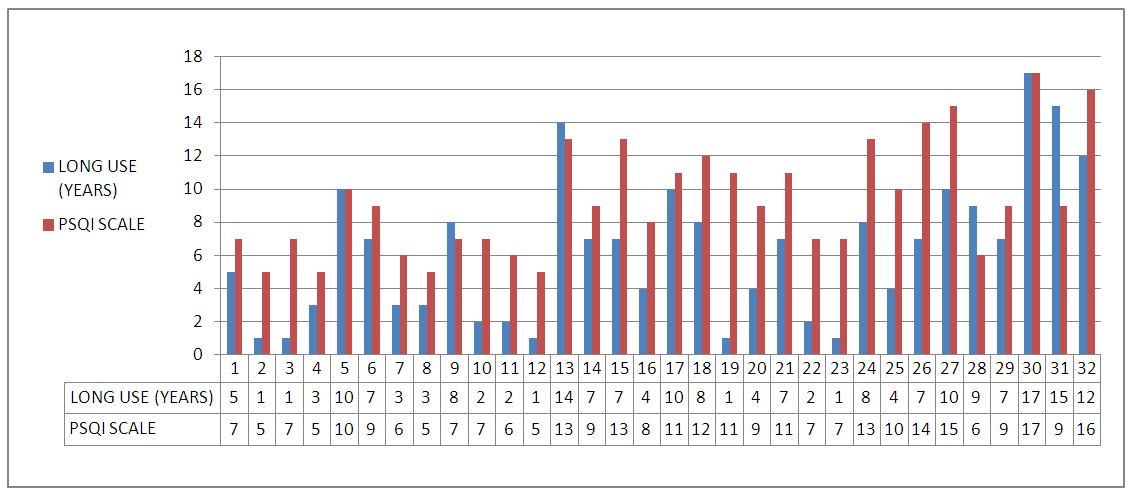
 | Figure 2. PSQI sleep quality scale on alprazolam used ≤6 months |
|
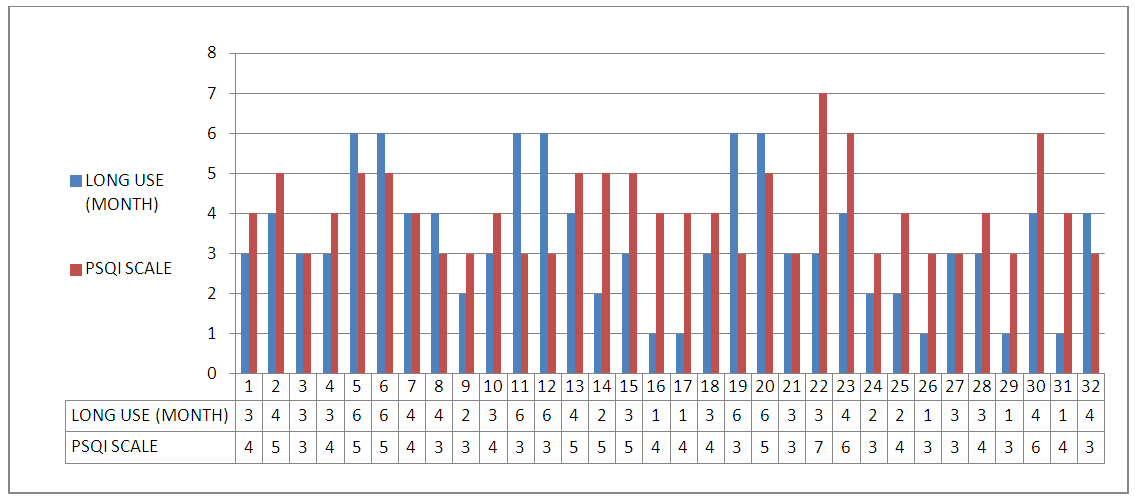
 | Figure 3. PSQI sleep quality scale on clobazam used >6 months |
 | Figure 4. PSQI sleep quality scale on clobazam used ≤6 months |
|
|
4. Discussion
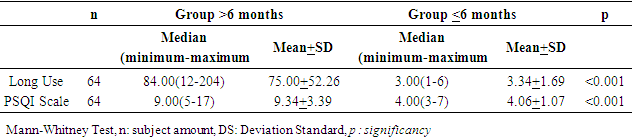
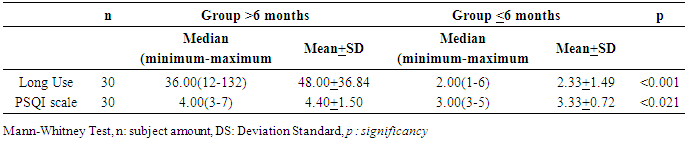
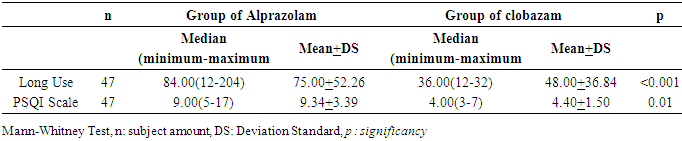
- This study showed the sleep quality in anxious disorder subjects who were taking long-term benzodiazepine therapy of both alprazolam and clobazam was worse than subjects who were taking short-term therapy. In this study, sleep quality assessment using the Indonesian version of PSQI was performed in subjects receiving benzodiazepine therapy >6 months and subjects receiving benzodiazepine therapy ≤6 months. Based on the data of the subjects characteristics, the number of sexes was almost equal in both groups, although statistically there were more females in the >6 month group. This is in accordance with the theory of anxiety disorders that epidemiologically women are twice more prone to experience anxiety disorders than men. Characteristics of the subjects by age group, it is seen that the number of subjects at the age group range from 41 to 50 years is bigger than other age groups. Based on the educational level the proportion of the distribution is almost the same. At the age level and education, it is mentioned that anxiety disorders can occur at all age levels and all social status and education. Although it is known most often this anxiety disorder develops in the adult age of 25 years and above. [7, 8]The results in this study were statistically tested using the Mann-Whitney and Wilcoxon test. Significant value in the groups receiving alprazolam therapy of p <0.001 was obtained. The above results were also reinforced by median data and mean values obtained that is; median value of sleep quality in groups >6 months receiving alprazolam therapy was 9.00, the mean value was 9,34 and standard deviation (SD) was 3,395. This value was higher than median value and mean in groups ≤6 months ie median=4.00, mean=4.06 and standard deviation (SD)=1.076. Similarly, in subjects receiving benzodiazepine type of clobazam therapy, there was a significant difference between groups >6 months and groups ≤6 months (p= 0.021) or significance p <0,05. For the value of sleep quality in groups >6 months, median value= 4.00, mean= 4.40 and standard deviation (SD)= 1.502 this value was higher than the value in groups ≤6 months with median= 3.00, mean= 3,33 and standard deviation (SD)= 0.724. This result is consistent with the initial hypothesis of sleep quality as measured by the Pitssburgh Sleep Quality Index (PSQI) score that sleep quality in patients receiving long-term benzodiazepine therapy for >6 months is worse than patients receiving short-term benzodiazepine therapy for ≤6 months.In each of the benzodiazepine therapy groups, both alprazolam and clobazam, indicated an increase in sleep quality scales measured using the Indonesian version of the PSQI scale in subjects receiving therapy >6 months and ≤6 months. But there are also some subjects whose PSQI sleep quality scales does not match the existing trend, which increases in the shorter time and decreases for a longer time than other subjects. This shows the varied response of each subjects to sleep quality after receiving benzodiazepine therapy. In addition, several factors such as biological factors, namely the body's response to pharmacotherapy and onset of the disturbance experienced, psychosocial factors or personality of the person in overcoming stressor and environmental factors, mistakes or lack of understanding in filling out the questionnaire given can also make the varied response. As is known, many factors might affect one’s quality of sleep, among others, health status, environment, psychological stress, diet, drugs, lifestyle. [15, 18]The difference in sleep quality results in alprazolam and clobazam may also be due to differences in chemical structure between the two. Alprazolam has a chemical structure of 8-chloro-1-methyl-6-phenyl-4H-triazole [4,3-α] -benzodiazepine and the formula (C17H13CIN4) while clobazam has a chemical structure of 7-chloro-1-methyl-5-phenyl-1,5 benzodiazepine-2,4 (3H, 5H) -dione and C16H13CIN2O2 formulas. Clobazam is the newest derivative of the benzodiazepine group used primarily for anxiolytic and more specific anti-convulsions having substituted 1.5 diazepine instead of the usual substitution of 1.4 diazepine, and has the least sedation effect compared to other benzodiazepines. [9, 14, 17, 23] Before conducting an assessment of the scale of the Pittsburgh Sleep Quality Index (PSQI) Indonesian version, then first tested was the validity and reliability. Validity test aims to measure the quality of research instruments. The instrument is said to be valid if the instrument can measure what should be measured. A research instrument is acceptable if the loading value of each item is ≥0.4. PSQI questionnaire in this study obtained loading of each item is ≥0,6, so the scale of Pitssburgh Sleep Quality Index (PSQI) Indonesian version used is valid. [5, 10]Reliability test aims to measure the reliability of a measuring instrument or questionnaire. The instrument is said to be reliable if used multiple times to measure the same object will produce the same data, a research instrument can be said to be reliable if it has a Cronbach’s Alpha value of ≥0.60. The closer to the number 1 cronbach’s alpha value, the better the instrument is. In this study, reliability testing was using Cronbach’s alpha analysis method with the help of SPSS, and was obtained Cronbach’s alpha of 0.810 so that the scale of Indonesian version of PSQI used in this research can be said reliable. [5, 10]Limitations and obstacles in this study were; no measurements of sleep quality scale of PSQI in subjects prior to therapy, no measurement of the degree scale of anxiety before the PSQI sleep scale measurement was performed, and the participants' subjectivity in filling out the questionnaire of PSQI quality of sleep.
5. Conclusions
- The results of this study are using the Indonesian version of the Pitssburgh Sleep Quality Index (PSQI), the sleep quality is worse in the subjects who take long-term benzodiazepine use (alprazolam and clobazam) compare to those who take short-term therapy. There was significantly difference sleep quality of the subjects who were taking long-term of both alprazolam and clobazam, otherwise there was no significant difference in sleep quality of the subjects who were taking short-term of both alprazolam and clobazam. The authors recommend analyzing the sleep quality of long-term use of other benzodiazepine derivatives such as lorazepam, estazolam, diazepam compared nonbenzodiazepine groups such as zolpidem, zaleplon, and ramelteon.
ACKNOWLEDGEMENTS
- The authors declare no potential conflict of interest in writing this original article. The authors would like to acknowledge the important support and contributions of Irfan Idris, M.D. (department of physiology) and Idham Jaya ganda, M.D. (Pediatrician; Research Methodology Advisor).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML