-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2018; 6(1): 1-8
doi:10.5923/j.ijcp.20180601.01

Care Giver Burden & Assessment of Personality Profile in Primary Care Giver of Dementia of Alzheimer’s Type
1Post Graduate Junior Resident in Dept. of Psychiatry TMMC & RC, Moradabad (UP), India
2Associate Professor in Dept. of Psychiatry, TMMC & RC, Moradabad (UP), India
Correspondence to: Swati Singh, Post Graduate Junior Resident in Dept. of Psychiatry TMMC & RC, Moradabad (UP), India.
| Email: |  |
Copyright © 2018 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

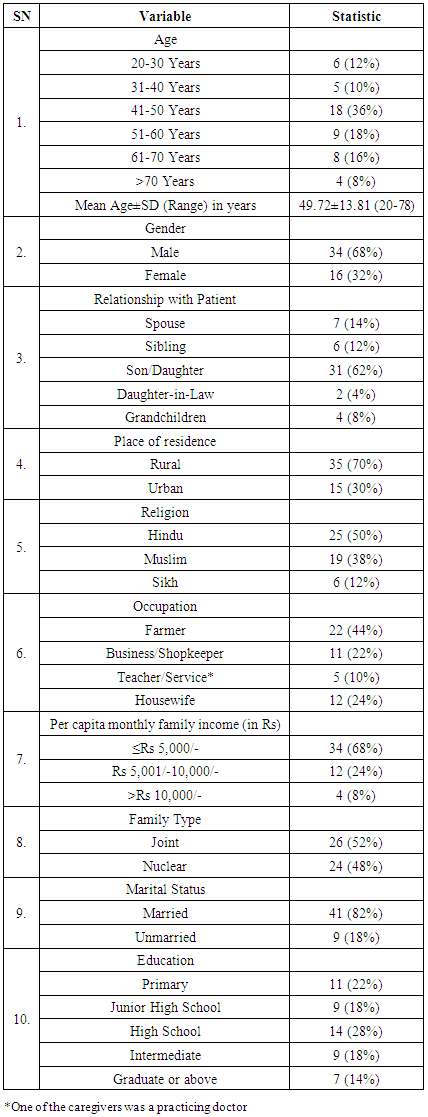
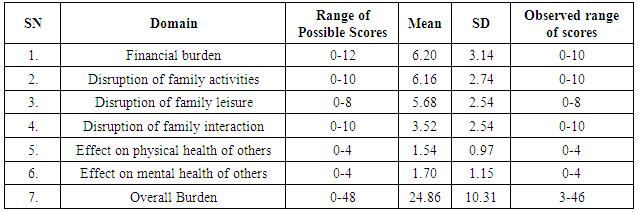
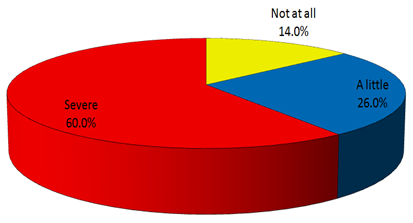
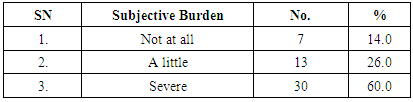
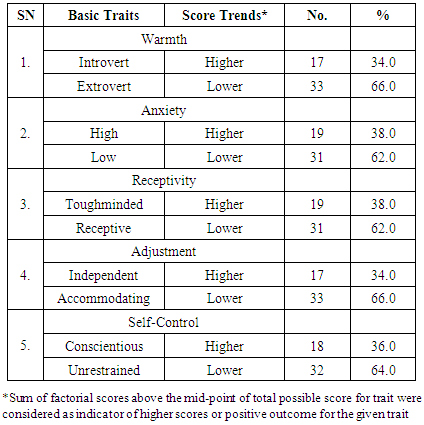
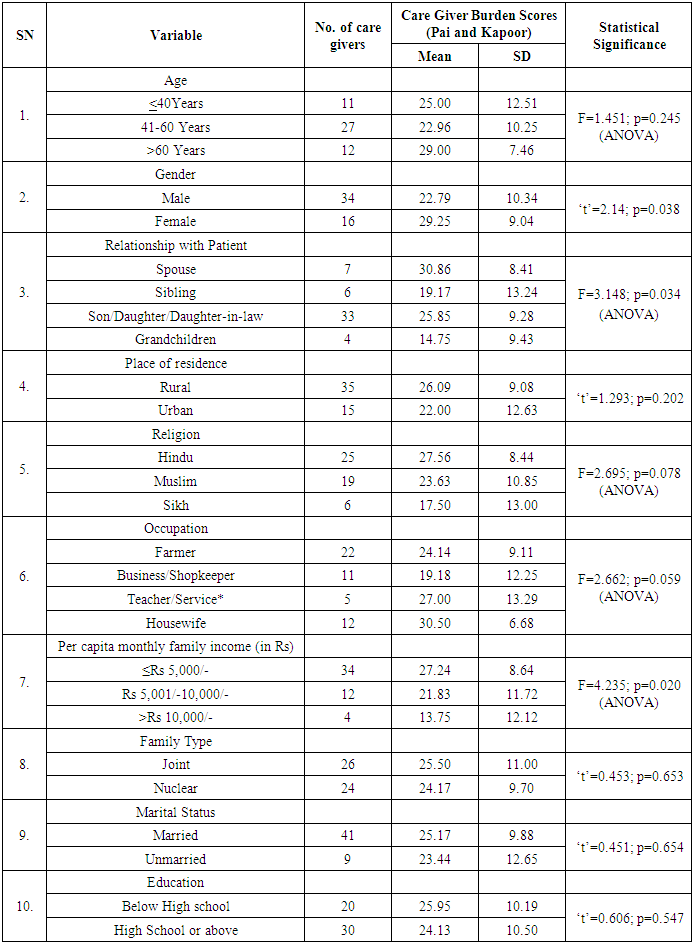
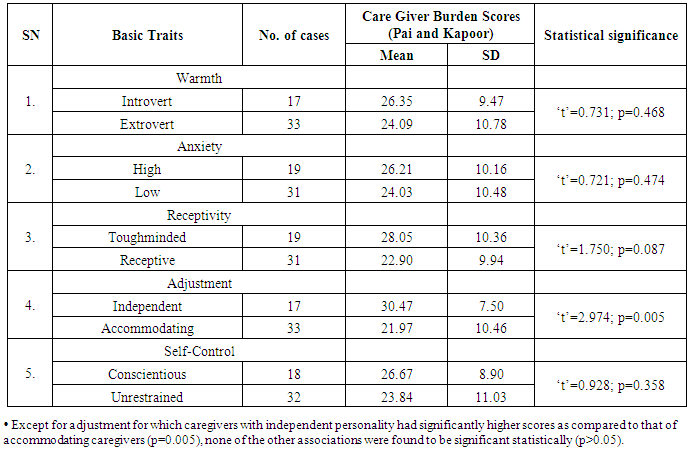
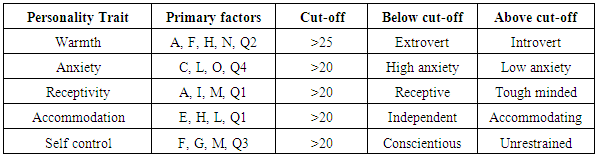
Background: Dementia is marked by severe impairment in memory, judgment, orientation and cognition. Alzheimer’s is the most common form of Dementia, usually occurs in person over 65 year of age Primary caregiver will be defined as a relative who has been staying with the patient for at least two years with continuous contact, and is actively involved in his or her care. “The overall impact of physical, psychological, social, and financial demands of caregiving has been termed caregiver burden. (3) The growing dependency associated with progression of Alzheimer’s, caregiver has to bear an increased level of burden and stress of care & management of Alzheimer’s patient. Aim: To Evaluate the Care Giver Burden & Personality in Primary Care Giver of Diagnosed cases of Dementia of Alzheimer’s type & Correlate Care Giver Burden Personality of Primary Care Giver. Materials and Methods: A cross-sectional study was conducted on a sample 50 Primary Care Giver of patients suffering from dementia of Alzheimer’s type fulfilling inclusion criteria for the study & visiting in Psychiatry, Medicine and Neurology OPD in TMMCRC, Moradabad using assessed by the KAPUR & PAI burden scale for care giver burden. 16 –PF scale will be used for personality assessment. Results: In present study, a total of 66%, 62%, 62%, 66% and 64% showed traits of extroversion, low anxiety, receptivity, accommodation and unrestrained authority respectively. In present study, overall burden of care scores ranged from 3 to 46 with a mean of 24.86±10.31. Subjective burden was stated as not at all, a little and severe by 14%, 26% and 60% of caregivers. Conclusion: The findings of present study showed that Caregivers of Alzheimer’s disease patients bear a heavy burden of care. It is essential that the impact of providing care on the family should be quantified and various characteristics affecting this caregiver burden need to be identified. This quantification and identification is essential from the point of view of formulating appropriate strategies to reduce this caregiver burden. A complete management plan for the patient of dementia includes a partnership building between health care professionals and caregivers of family, and psychosocial interventions as requiredd Although this is the First Study done in India to Assess the personality in Caregiver of Alzheimer’s patients. Personality factors also influence the level of burden probably owing to difference in coping strategies.
Keywords: Alzheimer's Dementia, 16-Personality Factor, Care Giver, Burden, Kapur & Pai
Cite this paper: Swati Singh, Prerana Gupta, Care Giver Burden & Assessment of Personality Profile in Primary Care Giver of Dementia of Alzheimer’s Type, International Journal of Clinical Psychiatry, Vol. 6 No. 1, 2018, pp. 1-8. doi: 10.5923/j.ijcp.20180601.01.
Article Outline
1. Introduction
- “Dementia is marked by severe impairment in memory, judgment, orientation and cognition. Alzheimer’s is the most common form of Dementia, usually occurs in person over 65 year of age.” [1]. Alzheimer’s is a general term for memory loss and other intellectual abilities serious enough to interfere with daily life. Alzheimer’s disease accounts for 50 to 80% of dementia cases. [1] Caregiver has been defined as a support to family members or relatives who are undergoing physical, psychological and developmental problems and are not able to perform certain tasks on their own. “A Primary caregiver will be defined as a relative who has been staying with the patient for at least two years with continuous contact, and is actively involved in his or her care.”The overall impact of physical, psychological, social, and financial demands of caregiving has been termed caregiver burden. [3] The growing dependency associated with progression of Alzheimer’s, caregiver has to bear an increased level of burden and stress of care & management of Alzheimer’s patient. [4] Caregiver of patients with Dementia of Alzheimer’s type is at risk of decreased psychological well-being as well as clinically significant psychiatric comorbities. Despite of large and growing body of data on caregiver burden, there are significant gaps in our understanding of the factor that contribute to individual differences in the caregiver stress, burden and including the role of personality and socio-demographic profile. [9] Caregiver often manage changing demands and unexpected problem behaviours. They often sacrifice their own needs, well-being to provide care for their loved ones. In this study we will review the consequences of caring for and individual with dementia in term of burden & impact of personality for dementia caregiver. A complete management plan for the patient of dementia includes a partnership building between health care professionals and caregivers of family, and psychosocial interventions as required [10] As Care Givers constitutes a major support system in the continuing care of chronic mentally ill in the community. Their share of physical and emotional distress cannot be ignored. It is important for us to be sensitive to the distress and burden experienced by caregivers, in order to plan a comprehensive treatment program. This would also facilitate the quality of life of both- the mentally ill and their families [11].
2. Aims & Objectives
- 1. To Evaluate the Care Giver Burden & Personality in Primary Care Giver of Diagnosed cases of Dementia of Alzheimer’s type.2. To Correlate Care Giver Burden Personality of Primary Care Giver.
3. Methodology
- 1. 50 outdoor co-resident caregiver of patient suffering from dementia of Alzheimer’s type will be included in the study after obtaining written informed consent.2. These groups will be assessed by the KAPUR & PAI burden scale for care giver burden.3. 16 –PF scale will be used for personality assessment.To be eligible for the study, the patients will have to fulfil all of the following:Inclusion criteriaa) Primary Care Giver of Patients with diagnosis of Alzheimer’s by DSM-5 criteria would be included in the studyb) A Primary caregiver will be defined as a relative who has been staying with the patient for at least two years with continuous contact, and is actively involved in his or her carec) Care giver of both sexes & should be above18 year of aged) Care Giver willing to give written informed consent regarding participation in study.e) Care Giver who does not have any psychiatric or medical/surgical illness.Exclusion criteriaa) Participants having major medical/psychiatric or surgical illness.b) Participants not giving written informed consent.c) Participants suffering from mental retardation or any other cognitive dysfunction.e) Care Giver living in family have > 1 dementia patient and other major medical or psychiatric illness will be excluded.Instruments16-PF: Personality Factor-16 Questionnaire (Catell and Mead, 2008)The Sixteen Personality Factor Questionnaire (16PF), is a self-report personality test. The 16PF provides a measure of normal personality and can also be used by psychologists, and other mental health professionals, as a clinical instrument to help diagnose psychiatric disorders, as well as help with prognosis and therapy planning. The 16PF instrument provides clinicians with a normal-range measurement of anxiety, adjustment, emotional stability and behavioral problems. The 16PF provides scores on 16 primary personality scales and 5 global personality scales, all of which are bi-polar (both ends of each scale have a distinct, meaningful definition). The primary factors of the scale include – warmth (A), reasoning (B), emotional stability (C), dominance (E), liveliness (F), Rule-consciousness (G), Social boldness (H), Sensitivity (I), Vigilance (L), Abstractedness (M), Privateness (N), Apprehension (O), Openness to change (Q1), Self reliance (Q2), Perfectionism (Q3) and Tension (Q4).For each item the scores can range from 1 to 10.On the basis of these primary factors, five personality traits were recognized as follows:
 KAPOOR & PAI BURDEN SCALE: Family Burden Interview Schedule (FBIS) (Pai & Kapur, 1981).This is a semi structured interview schedule comprising of 24 items grouped under 6 dimensions, i.e.Financial burden,Disruption of routine family activities,Disruption of family leisure,Disruption of family interaction, Effect on physical health of others and Effect on mental health of others.The burden has been rated on a three point scale (viz. severe burden, moderate burden and no burden) for each item and a standard question to assess the “Subjective” burden was also included in the schedule. This scale has been developed in Indian setup, keeping in mind the Socio economic and the cultural conditions in India. The reliability & validity of the scale have been found to be satisfactory. The interrelated consistency was more than 0.78 by the authors of the schedule, which clearly states that the scale is reliable. Validity of the scale was assessed by correlating objective burden rating with subjective burden, as reported by the relatives of the patient. The correlation found to be 0.72, which was considered significant. The scale though primarily devised for patients of psychotic disorder, can be used with neurotic patients, patients with alcohol or drug dependence, mental retardation and physical illness.Sample size & Statistical analysis:50 Primary Care Giver of patients suffering from dementia of Alzheimer’s type fulfilling inclusion criteria for the study & visiting in Psychiatry, Medicine and Neurology OPD in TMMCRC, Moradabad from 1st Jan 2016 – 31st Dec 2016.The obtained data will be tabulated and analysed by appropriate statistical tests.Permissions and Clearance:Clearance for the project was obtained from the Institutional Ethical Committee. Informed consent was obtained from all the patients participating in the study.
KAPOOR & PAI BURDEN SCALE: Family Burden Interview Schedule (FBIS) (Pai & Kapur, 1981).This is a semi structured interview schedule comprising of 24 items grouped under 6 dimensions, i.e.Financial burden,Disruption of routine family activities,Disruption of family leisure,Disruption of family interaction, Effect on physical health of others and Effect on mental health of others.The burden has been rated on a three point scale (viz. severe burden, moderate burden and no burden) for each item and a standard question to assess the “Subjective” burden was also included in the schedule. This scale has been developed in Indian setup, keeping in mind the Socio economic and the cultural conditions in India. The reliability & validity of the scale have been found to be satisfactory. The interrelated consistency was more than 0.78 by the authors of the schedule, which clearly states that the scale is reliable. Validity of the scale was assessed by correlating objective burden rating with subjective burden, as reported by the relatives of the patient. The correlation found to be 0.72, which was considered significant. The scale though primarily devised for patients of psychotic disorder, can be used with neurotic patients, patients with alcohol or drug dependence, mental retardation and physical illness.Sample size & Statistical analysis:50 Primary Care Giver of patients suffering from dementia of Alzheimer’s type fulfilling inclusion criteria for the study & visiting in Psychiatry, Medicine and Neurology OPD in TMMCRC, Moradabad from 1st Jan 2016 – 31st Dec 2016.The obtained data will be tabulated and analysed by appropriate statistical tests.Permissions and Clearance:Clearance for the project was obtained from the Institutional Ethical Committee. Informed consent was obtained from all the patients participating in the study.4. Result
|
|
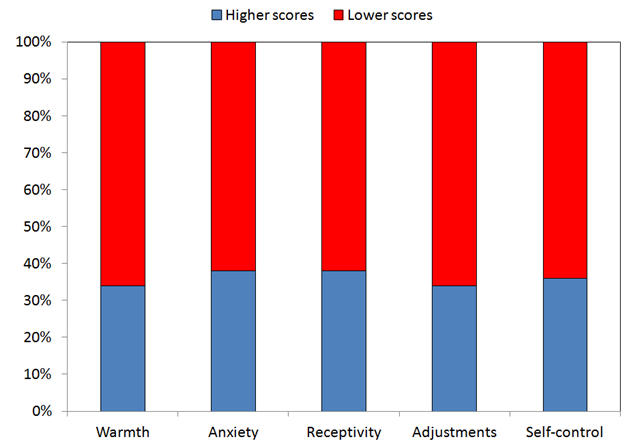 | Figure 2. Personality Pattern of caregivers for different traits |
|
|
|
|
5. Discussion
- In west, where psychiatric illness is considered to be as important as physical illness, remarkable work has been carried out on caregiver burden, among caregivers to Alzheimer patients, however, in India, where psychiatric illnesses are generally given less importance, there is limited or almost no work done on understanding the caregiver burden and its different dimensions. In present study we made an attempt in that direction.In present study majority of patients were females (62%). Epidemiological studies place the risk of Alzheimer’s disease to be twice as higher in females as compared to that in males [12, 13].Given the higher risk of Alzheimer disease among females, the higher proportion of female patients can be well explained, however, despite gender differences in occurrence as depicted in epidemiological studies, the gender differences in clinical studies might be attributable to difference in health care services utilization trends.In present study, duration of illness ranged from 1 to 6 years. Mean duration of illness was 1.61±0.83 years. The duration of disease in present study was relatively much lesser than that reported in several previous studies. Iavarone et al. [14]In present study per capital monthly family income was ≤Rs 5,000 in 34 (68%) cases, majority (52%) lived in a joint family, 82% were married and 60% were educated upto High school or above. Compared to present study, Pattanayak et al. [15] in their study showed dominance of urban (90.63%) caregivers, however, similar to present study they also showed a dominance of joint family (71.8%) and married (96.88%) caregivers.In present study, overall burden of care scores ranged from 3 to 46 with a mean of 24.86±10.31. Subjective burden was stated as not at all, a little and severe by 14%, 26% and 60% of caregivers. Although almost all the studies evaluating the caregiver burden report some burden on the caregivers yet the method of evaluation of this burden varies in different studies and so does the magnitude of the caregiver burden. Allegri et al. [16] evaluated this burden in terms of neuropsychiatric symptoms while Ferrera et al. [17] studied it in terms of stress, anxiety and depression. In present study, mean burden score was 24.86 out of a maximum possible score of 126, thus showing relatively much lower burden of care. Compared to this Pattanayak et al. [15] reported the mean burden of care score as 67.50 out of a maximum of 120, thus depicting a higher burden of care. Sung et al. [18] in their study also reported the mean care burden score of 51.09 out of a maximum of 110, thus depicting a higher care burden than observed in present study. There are multiple reasons for the lower care burden in present study. The first and foremost is the relatively shorter duration of illness in present study. Most of the previous studies have reported the duration of disease or care burden of longer duration. Pattanayak et al [15] in their study reported the mean duration of illness to be 3.31 years while Sung et al. [18] in their study had all the caregivers with at least 2 years or more of caregiving exposure. Compared to this, the present study had relatively much shorter duration of illness (1.61 years) and this could be responsible for relatively lesser burden of care. Secondly, the age of caregivers in present study was relatively younger, thus giving them more strength to cope with the burden. Thirdly, most of caregivers in present study had a rural background and had fewer occupational overlaps. These distinctions of the caregiver characteristic definitely have a detrimental role in lowering the care burden. Moreover, the role of social support extended by joint family can also not be ruled out. In present study, we had used PF-16 assessment for evaluating the personality traits of caregivers. Although, role of personality as a determinant of caregiving burden has been studied in several previous studies too, [18-20]. However, use of 16-PF scale among caregivers of Alzheimer’s patients has been done in only one study previously. In present study, we truncated the personality traits into five-major factors and found that majority of caregivers in present study had dominance of positive traits. In present study, a total of 66%, 62%, 62%, 66% and 64% showed traits of extroversion, low anxiety, receptivity, accommodation and unrestrained authority respectively. Presence of these positive personality traits in majority of caregivers in present study is another finding which can be attributed to lesser burden of care in our set of caregivers.In present study, among different personality traits, those having independent personality had significantly higher burden of care as compared to those having accommodating personality. As far as recognition of appropriate personality trait reducing the burden of care is concerned there are different outcomes in different studies. Melo et al. [18] in their study reported neuroticism as an enhancer and extraversion as a suppressor of caregiver’s burden Reis et al. [19] in their study showed that neuroticism is associated with higher burden of care. In present study, we had used PF-16 scale for evaluation of personality traits. In a previous study, Vista et al. [20] has also used PF-16 and reported that caregivers characterized by emotional instability, unable to stand frustration, high self-demanding and with difficulty in self abstracting from concrete problem solving perceived higher distress in caregiving persons with AD. In present study we also found that independent/self-demanding instead of accommodating caregivers experienced a significantly higher burden of care.
6. Conclusions
- The findings of present study showed that Caregivers of Alzheimer’s disease patients bear a heavy burden of care. Personality factors also influence the level of burden probably owing to difference in coping strategies. Although this is the First Study done in India to Assess the personality in Caregiver of Alzheimer’s patients. The limitation of study was absence of long-term caregiving experience (>5 years). Further studies on larger sample size among caregivers with prolonged history of Alzheimer’s disease care is recommended.
ACKNOWLEDGEMENTS
- I would like to thank Dr. A.Q Siddiqui Prof. & Head in dept. of psychiatry TMMC & RC, Dr Prerana Gupta, Associate professor in dept. of psychiatry, TMMC & RC, Dr Seema Singh, Assistant prof. in dept. of psychiatry TMMC & RC & Dr. Azfer Ibrahim Senior resident in dept. of psychiatry TMMC & RC and Ms. Shubhi Agarwal, clinical psychologist in dept. of psychiatry, TMMC & RC for allowing me to conduct the study as well as encouraging me towards the studies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML